Diarrhea isn’t just a bad day at the bathroom-it’s a symptom that can signal anything from a quick virus to a serious, long-term condition. If you’ve had three or more loose stools in a day, you’re experiencing diarrhea. But here’s the key: not all diarrhea is the same. The difference between acute and chronic diarrhea isn’t just about how long it lasts-it changes everything about how you treat it, what tests you need, and whether you should even reach for an over-the-counter pill like Imodium.
What Exactly Is Acute Diarrhea?
Acute diarrhea hits fast and usually leaves just as quickly. It’s defined as lasting 14 days or less. Most of the time, it starts with a sudden bout of watery stools, cramps, maybe a low fever, and an urgent need to get to the toilet. It’s the kind of thing you get after eating bad sushi, drinking contaminated water, or catching a stomach bug from your kid.
In the U.S., about 179 million cases happen every year. Globally, it’s worse-1.7 billion cases annually, and it’s the second biggest killer of children under five. Rotavirus used to be the main culprit, but thanks to vaccines like RotaTeq and Rotarix, hospitalizations from it have dropped by 80-94% in countries with full immunization programs.
Most cases (70-80%) are viral. Bacteria like Salmonella or Campylobacter cause 10-20%, and parasites like Giardia make up the rest. The good news? About 90% of acute cases clear up on their own in 5-7 days. You don’t need antibiotics. In fact, using them unnecessarily can make things worse by killing off good gut bacteria and increasing the risk of antibiotic-resistant infections.
What Makes Chronic Diarrhea Different?
Chronic diarrhea doesn’t go away. It lasts more than 14 days-often weeks or months. It’s not something you catch; it’s something you develop. About 5% of adults in developed countries live with it. And unlike acute diarrhea, it’s rarely caused by an infection.
The real causes? Inflammatory bowel disease (IBD), like Crohn’s or ulcerative colitis, affects 1.6 million Americans. Irritable bowel syndrome with diarrhea (IBS-D) hits 10-15% of people worldwide. Bile acid malabsorption after gallbladder removal affects 25-30% of those patients. Medications-especially antibiotics, metformin, or certain blood pressure drugs-can trigger it too. And don’t forget celiac disease: 40% of cases are first misdiagnosed as IBS.
Chronic diarrhea has patterns. If you’re having watery stools at night, that’s a red flag for secretory diarrhea-something your body is producing too much of. If your stools are greasy and float, that’s steatorrhea, pointing to pancreatic or bile problems. Blood or mucus in the stool? That’s inflammation. These clues tell doctors what to test for.
Why the Difference Matters
Here’s where people get hurt: treating chronic diarrhea like it’s acute. If you take loperamide for weeks because you think it’s just a "bad stomach," you could be masking something serious-like colon cancer, Crohn’s, or a hidden infection. Doctors won’t order a colonoscopy or blood tests for a 3-day bout of diarrhea. But if it’s been going on for 6 weeks? That’s a full diagnostic workup.
Acute diarrhea? Focus on hydration. Oral rehydration solution (ORS)-a precise mix of salt, sugar, and water-is the gold standard. The WHO formula has been proven to cut child deaths from diarrhea by 93%. Forget the BRAT diet. Experts now say: eat normally as soon as you can. Bananas and toast won’t fix the problem, but food helps your gut heal faster.
Chronic diarrhea? You need answers. Blood tests (CBC, CRP, thyroid), stool tests (calprotectin for inflammation), breath tests for SIBO, and sometimes a colonoscopy. Without this, you’re just treating symptoms-not the disease.
Antimotility Agents: When They Help and When They Hurt
Loperamide (Imodium) is the most common antimotility drug. It slows down your gut, reduces stool frequency, and can make life bearable. For someone with IBS-D, it’s a game-changer. One patient reported going from 10 bowel movements a day to just 2-3 after taking 2mg before meals. That’s the kind of result that lets people go back to work, travel, or even have a date without panic.
But here’s the catch: loperamide isn’t safe for everyone. If you have a fever, bloody stools, or suspect a bacterial infection like Shiga-toxin E. coli, taking loperamide can trap toxins in your colon. That’s how you get hemolytic uremic syndrome-a life-threatening condition that can cause kidney failure. The FDA warns against it in children under 2 and says to use extreme caution in kids 2-5.
And then there’s abuse. Between 2011 and 2021, the FDA recorded 1,247 cases of loperamide misuse, including 57 deaths. People took 10, 20, even 50 tablets a day trying to get high or self-treat opioid withdrawal. That’s why, since 2018, loperamide packages in the U.S. are limited to 48mg per box (24 tablets of 2mg).
Bismuth subsalicylate (Pepto-Bismol) is another option. It’s less potent than loperamide but has mild antibacterial effects. It’s okay for short-term use in acute cases. But if you’re on blood thinners or aspirin-sensitive, skip it.
What to Do When Diarrhea Won’t Quit
If your diarrhea lasts more than two weeks, don’t wait. See a doctor. Don’t self-diagnose as IBS. Don’t keep increasing your loperamide dose. One Reddit user reported needing 8mg daily just to have three bowel movements a week. That’s not control-that’s dependence.
Start tracking: When does it happen? After meals? At night? With stress? What does the stool look like? Is it greasy? Bloody? Do you lose weight? These details matter. A 2022 study found patients waited an average of 6 months and saw 3.7 doctors before getting the right diagnosis.
For IBS-D, the low-FODMAP diet works for 50-75% of people-but it’s not simple. It takes 6-8 weeks under a dietitian’s guidance. For bile acid malabsorption, drugs like cholestyramine can help. For celiac disease, a strict gluten-free diet is the only treatment.
The Bigger Picture
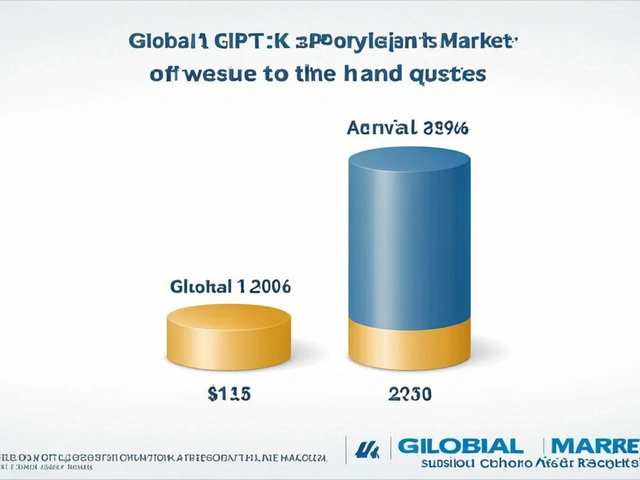
Diarrhea isn’t just a nuisance-it’s a global health crisis. In low-income countries, it kills over 500,000 children a year. In the U.S., it costs $2.8 billion annually in medical bills and lost productivity. The market for antimotility drugs hit $1.27 billion in 2022, with loperamide making up nearly 70% of sales.
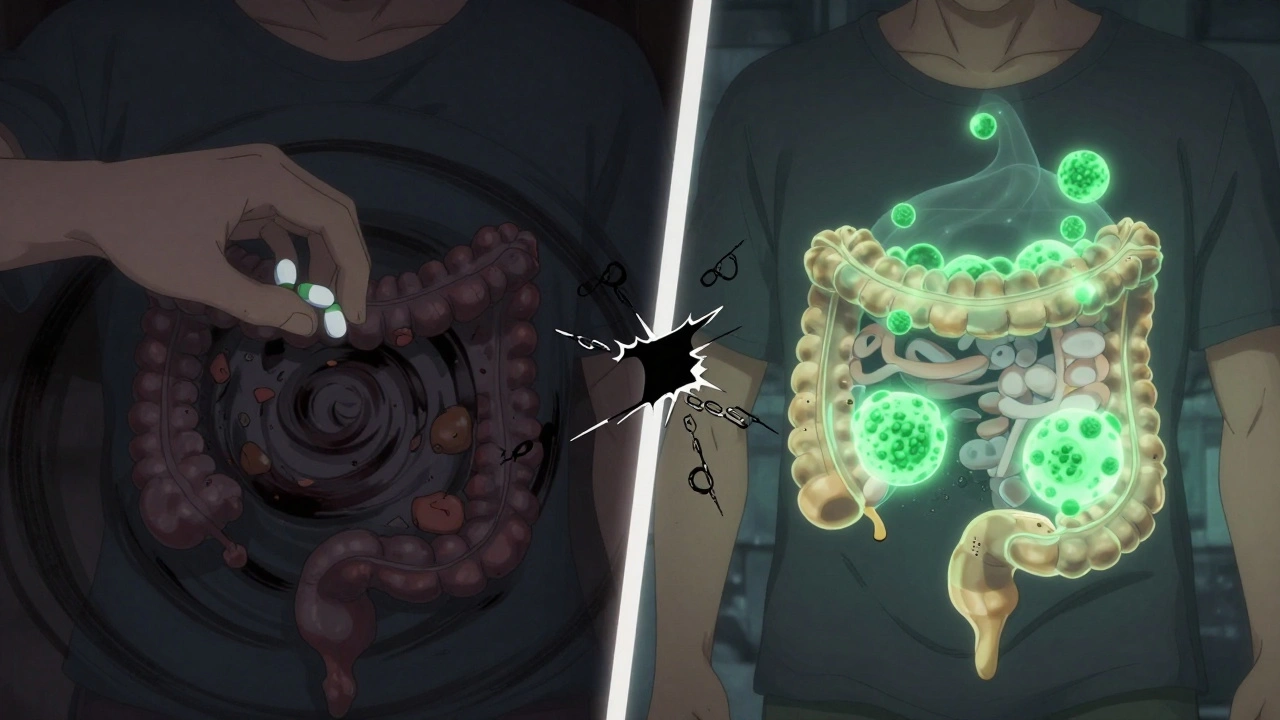
But the future is changing. New extended-release loperamide formulations aim to reduce abuse. The WHO updated its ORS formula in 2022 to be more effective. And research into fecal microbiota transplants (FMT) for recurring C. diff infections is showing 85-90% success rates.
What’s next? Personalized treatment. Doctors are starting to use stool biomarkers to tell if your diarrhea is caused by bile acids, inflammation, or a gut microbiome imbalance. In five years, you might get a test that tells you exactly which drug-or diet-will work for you.
When to Worry
Here’s your quick checklist: Go to the doctor if you have:
- Diarrhea lasting more than 14 days
- Bloody or black stools
- Fever over 38.5°C (101.3°F)
- Unexplained weight loss
- Nocturnal diarrhea (waking up to go)
- Severe dehydration (dizziness, dry mouth, no urine for 8 hours)
If you’re over 50 and new to diarrhea, get checked. Cancer risk rises with age.
What You Can Do Right Now
For acute diarrhea:
- Drink oral rehydration solution (ORS) or a mix of 1 liter water + 6 tsp sugar + 1/2 tsp salt
- Eat bland, easy-to-digest foods (rice, bananas, chicken broth)
- Avoid dairy, caffeine, alcohol, and high-fat foods until it passes
- Use loperamide only if needed, and never exceed 16mg in 24 hours
For chronic diarrhea:
- Keep a food and symptom diary
- Stop self-medicating with loperamide
- Ask your doctor about stool calprotectin, thyroid tests, and celiac screening
- Consider seeing a dietitian for low-FODMAP or bile acid diet guidance
Is loperamide safe for long-term use?
Loperamide is not meant for long-term use. While it can help manage symptoms of IBS-D or bile acid diarrhea, taking it daily for months can lead to tolerance (needing higher doses), constipation, and masking serious conditions like Crohn’s disease or colon cancer. The FDA warns against using it beyond a few days without medical supervision.
Can stress cause chronic diarrhea?
Yes. Stress doesn’t cause diarrhea directly, but it can trigger or worsen IBS-D, a functional bowel disorder. The gut and brain are closely connected. Anxiety can speed up gut motility, increase sensitivity, and make stools looser. Managing stress through therapy, mindfulness, or medication can improve symptoms-sometimes as much as diet changes.
Why does diarrhea happen at night?
Nocturnal diarrhea is a red flag. Normal diarrhea usually improves at night because your gut slows down. If you’re waking up to go, it suggests secretory diarrhea-where your body is actively producing excess fluid, often due to hormonal imbalances, bile acid malabsorption, or tumors. This isn’t typical IBS. It needs medical evaluation.
Is diarrhea always caused by an infection?
No. While infections cause most acute cases, chronic diarrhea is rarely infectious. Common causes include IBS, IBD, celiac disease, bile acid malabsorption, medication side effects, and pancreatic insufficiency. If diarrhea lasts more than two weeks, an infection is unlikely to be the main cause.
What’s better for diarrhea: loperamide or Pepto-Bismol?
Loperamide is stronger at reducing stool frequency and is preferred for chronic diarrhea like IBS-D. Pepto-Bismol has a milder effect but also kills some bacteria and reduces inflammation, making it useful for short-term acute cases, especially if you suspect food poisoning. But Pepto-Bismol contains salicylates, so avoid it if you’re allergic to aspirin or on blood thinners.
Can probiotics help with diarrhea?
Yes, but not all probiotics are the same. For antibiotic-associated diarrhea, strains like Lactobacillus rhamnosus GG and Saccharomyces boulardii have strong evidence. For IBS-D, the evidence is mixed. Align (Bifidobacterium infantis) helped some patients in trials, but results vary. Probiotics aren’t magic-they’re support tools. They won’t fix celiac disease or Crohn’s.
Final Thoughts
Diarrhea is common. But it’s not always harmless. Knowing whether it’s acute or chronic changes your next move. Don’t ignore it. Don’t overuse loperamide. Don’t assume it’s just stress or bad food. If it’s lasting longer than two weeks, get checked. The right diagnosis doesn’t just stop the diarrhea-it can save your life.






William Chin December 5, 2025
The author has presented a clinically accurate, evidence-based overview of acute versus chronic diarrhea - a topic often misunderstood by the public. However, the complete omission of antibiotic stewardship guidelines from the CDC and WHO in the context of traveler’s diarrhea is a significant oversight. In high-risk regions, empiric azithromycin is still first-line for suspected bacterial etiology, even with loperamide use. This omission could mislead readers into thinking antibiotics are universally contraindicated - which is dangerously incorrect in certain epidemiological contexts.
Lucy Kavanagh December 6, 2025
Did you know the FDA limits loperamide because Big Pharma doesn’t want you curing yourself? They’d rather you pay for colonoscopies and expensive blood tests. I’ve been taking 10 tablets a day for 3 years - no doctor ever asked why. My gut’s fine. The real problem? They’re hiding the truth about gut flora and glyphosate. Your microbiome is being poisoned by Roundup in your bread, your water, your vaccines. Wake up. The WHO is complicit.
Chris Brown December 7, 2025
While the article is technically sound, it indulges in a dangerous trend of normalizing chronic loperamide use under the guise of ‘IBS management.’ This is not medicine - it’s pharmacological appeasement. Patients are being taught to medicate symptoms rather than confront root causes. The normalization of self-medication with Schedule V drugs under the banner of ‘quality of life’ is a moral failure of modern gastroenterology. If you need Imodium to function, you’re not managing IBS - you’re avoiding the truth about your diet, your stress, or your unresolved trauma.
Michael Dioso December 8, 2025
Lol, this article is so basic. Everyone knows you don’t take Imodium with fever - that’s like putting a bandaid on a bullet wound. But here’s the real secret: 80% of chronic diarrhea cases are from bile acid malabsorption and nobody talks about it because it’s not profitable. Cholestyramine costs $5 a month. Insurance doesn’t cover it. So doctors push expensive stool tests and then prescribe expensive meds. Meanwhile, I took 4g of cholestyramine daily for 3 weeks and my diarrhea vanished. No colonoscopy needed. Just ask your pharmacist for the powder. Not the pills. The powder.
Krishan Patel December 10, 2025
One must recognize the metaphysical dimension of gastrointestinal distress. The bowels are not merely an organ system - they are the physical manifestation of emotional digestion. Chronic diarrhea, in my view, is the body’s rebellion against a life lived inauthentically. When one suppresses truth, avoids confrontation, or lives under the weight of societal expectation, the colon becomes the site of expulsion - of toxins, yes, but also of accumulated spiritual residue. The modern obsession with loperamide is a symptom of our collective refusal to confront inner chaos. Healing begins not with a stool test, but with silence, fasting, and the courage to sit with discomfort.
Carole Nkosi December 11, 2025
You people are obsessed with drugs and tests. In my village in South Africa, we use ginger, lemon, and honey. No doctor. No lab. No Imodium. We eat when we’re hungry, rest when we’re tired, and drink clean water. Diarrhea comes, diarrhea goes. It’s nature. You think your $300 colonoscopy is better than a grandmother’s wisdom? You’re poisoning your gut with your fear and your processed food. Stop looking for pills. Look inward.
Mark Curry December 13, 2025
Thanks for this. Really helpful. I had chronic diarrhea for 8 months and thought it was stress. Turned out it was bile acid malabsorption. Cholestyramine saved me. Just wanted to say - if you’ve had it for over 2 weeks, don’t wait. Go get tested. And don’t be embarrassed. Your gut doesn’t care if you’re ‘embarrassed.’ It just wants to work right. :)
Manish Shankar December 14, 2025
Thank you for this comprehensive and meticulously referenced exposition. I would like to respectfully supplement the discussion by highlighting the underappreciated role of vitamin D deficiency in chronic diarrhea, particularly in populations with limited sun exposure. A 2021 meta-analysis in the Journal of Clinical Gastroenterology demonstrated a 68% improvement in stool consistency following vitamin D repletion in patients with IBS-D and baseline levels below 20 ng/mL. This biochemical pathway - mediated through the VDR receptor in intestinal epithelial cells - warrants routine screening prior to initiating pharmacological or dietary interventions. The integration of nutritional biochemistry into gastroenterological practice remains woefully underdeveloped.