Ever opened a medicine bottle and wondered if it’s still good? Maybe you left your antibiotics in the car on a hot day, or kept your insulin in the bathroom cabinet. You’re not alone. A 2023 survey found that nearly 7 out of 10 people sometimes store their meds in places that could make them less effective-or even dangerous. But the answer isn’t guesswork. It’s right there on the label, if you know where to look.
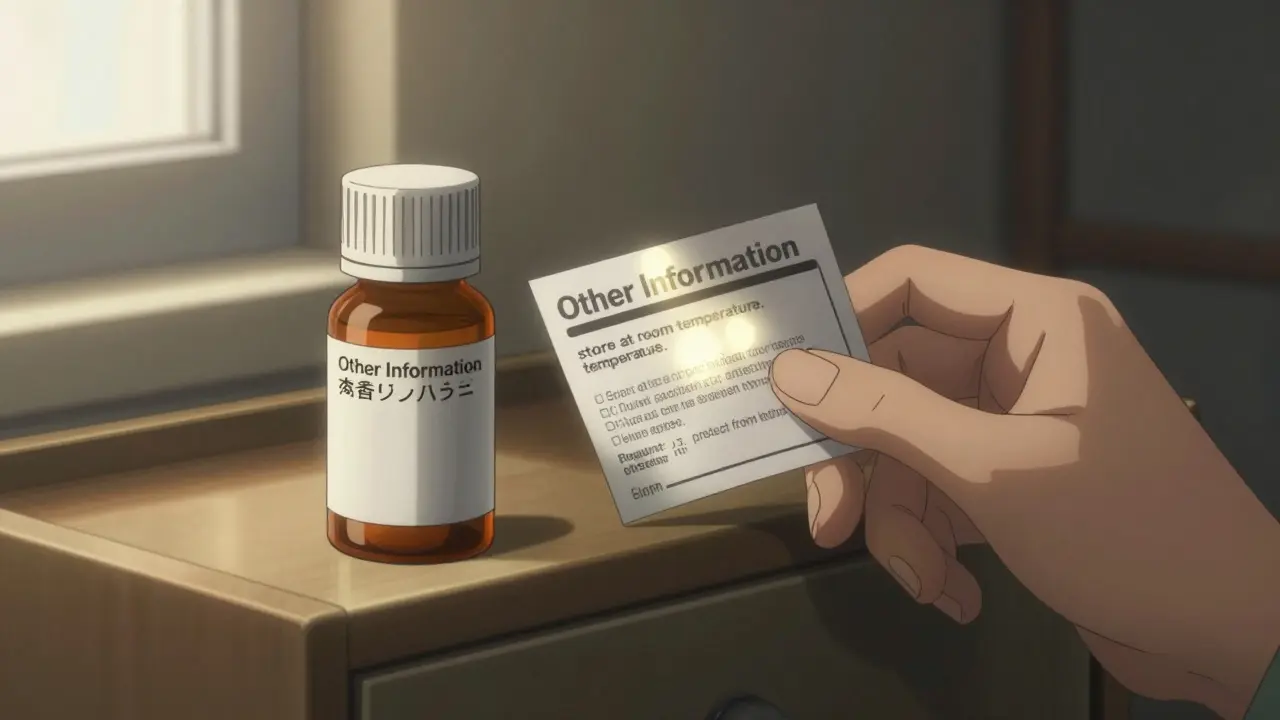
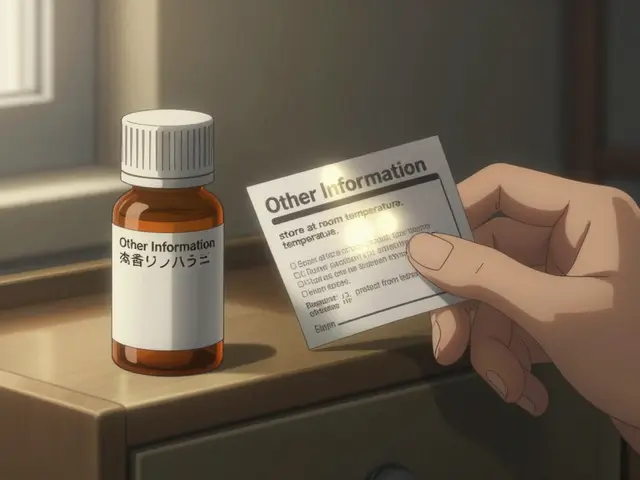
Where to Find Storage Instructions on the Label
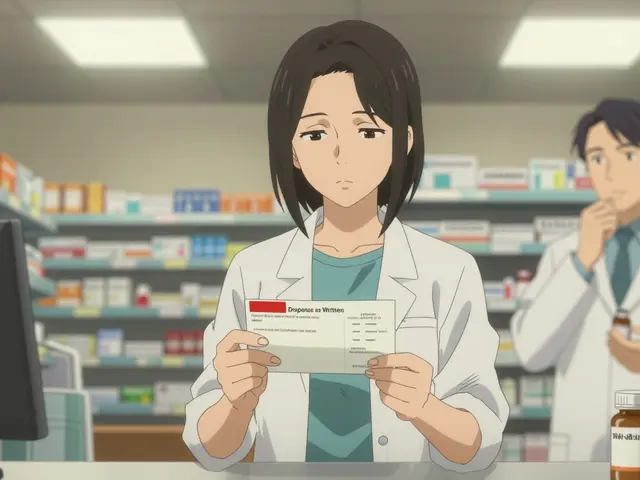
Storage instructions aren’t buried in tiny print. They’re placed where regulators require them to be easy to find. For over-the-counter (OTC) drugs like pain relievers or allergy pills, look at the Drug Facts label. That’s the standardized box you see on every box of Tylenol, Advil, or Claritin. Under the section labeled Other information, you’ll find storage details. It’s usually right after the directions for use and before the inactive ingredients. For prescription meds, the label might look different. Pharmacies print their own labels, but the information still follows federal rules. Look for a section titled Storage Instructions, or check the fine print near the bottom. Sometimes it’s grouped under How Supplied or Handling. If you’re unsure, the pharmacist who filled your script can point it out in seconds.What the Words Actually Mean
Don’t just skim. Read the exact wording. Terms like “store at room temperature” sound simple-but they mean something specific. The U.S. Pharmacopeia defines room temperature as 20°C to 25°C (68°F to 77°F). That’s your bedroom or kitchen counter, not your car or the windowsill. If it says “refrigerate,” that means between 2°C and 8°C (36°F to 46°F). Not the fridge door. The door swings in temperature every time you open it. Put refrigerated meds in the main compartment, where it’s coldest and most stable. This matters for insulin, liquid antibiotics, and some biologics. If you don’t, they break down fast. One study showed liquid antibiotics lose up to 30% of their potency after just 7 days if left unrefrigerated. “Protect from light” means keep it in its original bottle. Don’t transfer pills to a daily pill organizer unless it’s opaque. Sunlight and even bright indoor lights can degrade certain drugs like nitroglycerin or certain antibiotics. “Store in a dry place” is code for: avoid the bathroom. Humidity from showers and sinks can turn tablets into mush or make capsules stick together. Moisture doesn’t just ruin the pill-it can change how your body absorbs it. “Avoid freezing” is just as important as “refrigerate.” Some meds, like certain injectables or liquid suspensions, can permanently break down if they freeze. Even if they thaw out, they won’t work the same.What Happens If You Ignore These Instructions
You might think, “It’s just a pill. It’ll be fine.” But that’s where things get risky. Acetaminophen (Tylenol) can break down into a toxic compound if stored too hot or too humid. Insulin, if exposed to heat, stops working. People with diabetes have ended up in the ER because their insulin was left in a hot car. Nitroglycerin tablets-used for chest pain-lose effectiveness in as little as 3 months if not kept in their original glass bottle away from light and moisture. That’s not theoretical. It’s documented in FDA reports. The FDA tracked medication errors between 2020 and 2022 and found that 1.2% of all reported errors were linked to improper storage. That number is likely way higher because most people never report it. If your headache medicine doesn’t work, you don’t call the doctor-you just take another. But if that pill has degraded, you’re not getting the dose you think you are. And it’s not just about effectiveness. Some drugs become more toxic when they break down. One 2022 survey found that over a third of patients couldn’t tell if their temperature-sensitive meds had been compromised. That’s a hidden danger.
Common Mistakes (And How to Avoid Them)
Here are the top 5 storage mistakes people make-and how to fix them:- Mistake: Storing meds in the bathroom. Fix: Move them to a bedroom drawer or kitchen cabinet away from the sink.
- Mistake: Leaving pills in the car. Fix: Even on a mild day, a car’s interior can hit 140°F (60°C) in 30 minutes. That’s hotter than an oven. Keep meds with you, not in the glovebox or trunk.
- Mistake: Keeping refrigerated meds in the fridge door. Fix: Put them on a middle shelf. The door is the warmest part.
- Mistake: Transferring pills to clear containers. Fix: If you use a pill organizer, make sure it’s dark or opaque. Or, keep the original bottle and use a daily pill box only for the day’s dose.
- Mistake: Assuming all meds are fine in the same spot. Fix: If you take multiple drugs, create zones. One drawer for room-temp meds, one shelf in the fridge for refrigerated ones.
Special Cases: Kids, Travel, and Seniors
Children’s medications often have different storage rules than adult versions. A liquid amoxicillin for a toddler might need refrigeration after mixing, while the adult version doesn’t. Always check the label-and ask your pharmacist if you’re unsure. Traveling? If you’re flying or driving through hot climates, pack temperature-sensitive meds in a small insulated cooler with a cold pack. Don’t check them in luggage. The cargo hold can get extreme. The FDA recommends this for insulin, epinephrine pens, and some migraine meds. Seniors living in homes without air conditioning face real challenges. If your home regularly hits 30°C (86°F), your meds might be at risk. Talk to your pharmacist. Some drugs come in alternative forms-like patches or injections-that don’t require refrigeration. Medicare’s 2023 safety guide says pharmacists should offer these options when standard storage isn’t possible.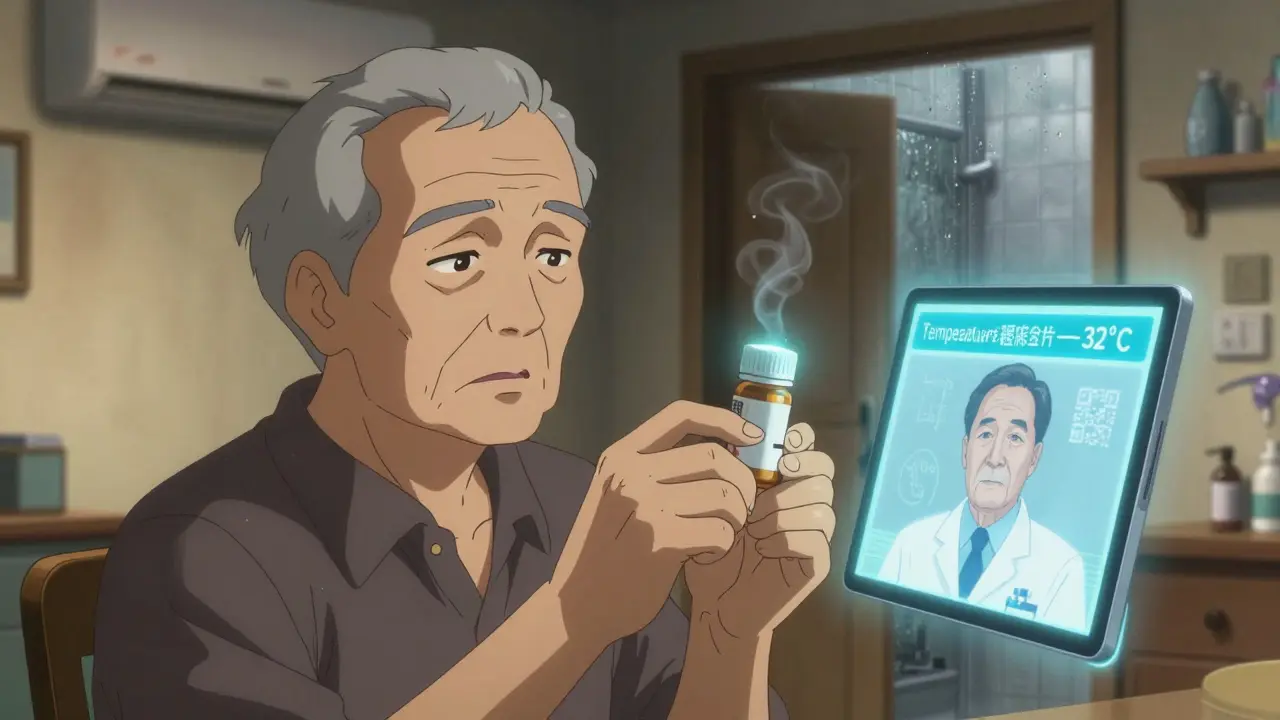
What to Do When You’re Not Sure
If the label says “store in a cool place” but you don’t know what that means, or if instructions seem conflicting, call your pharmacist. They’ve seen this before. They know if your medicine can handle a warm house, or if it needs a special setup. Don’t rely on Google. Don’t guess. Don’t assume your friend’s same medication works the same way. Each brand, each formulation, each batch can have different requirements. A 2023 study showed that people who asked their pharmacist about storage had 18.7% better adherence to their medication schedule. Why? Because they knew their meds were still good. Confidence leads to consistency.The Future Is Smarter Packaging
You might think labels won’t change much. But they are. Major pharmacies like CVS and Walgreens are testing QR codes on medication bottles. Scan it, and your phone shows real-time storage advice based on your location and current weather. If it’s 38°C outside, the app tells you to keep your insulin cool. In the next five years, some high-risk medications will come with built-in temperature sensors. If the pill bottle got too hot during delivery, the sensor will change color or send a warning to your phone. The FDA predicts this will become standard for insulin, biologics, and cancer drugs. Until then, the label is your best tool. It’s not just fine print. It’s a safety instruction.Quick Checklist: Storage Do’s and Don’ts
- DO: Store most meds in a cool, dry, dark place (like a bedroom drawer).
- DO: Keep refrigerated meds on the main fridge shelf, not the door.
- DO: Use original containers with child-resistant caps.
- DO: Ask your pharmacist if you’re unsure.
- DON’T: Store meds in the bathroom, car, or near the stove.
- DON’T: Transfer light-sensitive meds to clear containers.
- DON’T: Use expired meds-even if they look fine.
Medications aren’t like food. You can’t just smell them to tell if they’re bad. The only way to know they’re safe and effective is to follow the label. And that’s not just advice-it’s your health on the line.
What does "store at room temperature" really mean?
"Store at room temperature" means between 20°C and 25°C (68°F to 77°F). This is the range your home should naturally stay in-like a bedroom or kitchen cabinet away from windows or appliances. Avoid places that get too hot, like near the oven or in direct sunlight.
Can I store my insulin in the fridge door?
No. The fridge door opens and closes often, causing temperature swings that can damage insulin. Always store insulin on a middle shelf where the temperature stays steady between 2°C and 8°C (36°F to 46°F).
Why shouldn’t I keep pills in the bathroom?
Bathrooms are humid because of showers and sinks. Moisture can make pills crumble, capsules stick together, or cause chemical changes that reduce effectiveness. Even if the pill looks fine, it may not work as intended.
What if my medication label says "protect from light"?
Keep it in its original bottle, which is usually dark or opaque. Don’t transfer it to a clear pill organizer unless it’s also light-blocking. Sunlight and bright indoor lights can break down drugs like nitroglycerin, certain antibiotics, and some heart medications.
Is it safe to use expired medication if it looks okay?
No. Even if it looks normal, expired meds can lose potency or break down into harmful substances. The expiration date is based on how long the drug stays stable under proper storage. If it’s expired, dispose of it safely and get a new supply.





Sarthak Jain December 16, 2025
man i used to keep my antibiotics in the bathroom till i got sick again and realized the pills were kinda mushy. never again. humidity is the silent killer of meds.
Dwayne hiers December 17, 2025
Room temperature according to USP is 20–25°C, but most people don’t realize that ‘cool place’ means 8–15°C. That’s why insulin fails in summer cars - it’s not just heat, it’s thermal cycling. Stability data is non-negotiable.
Edward Stevens December 18, 2025
So let me get this straight - we’re being told to read labels now? Next they’ll tell us to brush our teeth and not lick the microwave.
Alexis Wright December 20, 2025
Here’s the uncomfortable truth: 87% of patients don’t understand ‘refrigerate’ means ‘don’t put it next to the milk.’ The FDA doesn’t regulate stupidity, and we’re paying for it in ER visits. This isn’t about education - it’s about systemic negligence. You think a QR code will fix this? It won’t. People still won’t scan it.
And let’s not forget: expired meds aren’t just ineffective - they’re biohazards. That Tylenol you kept since 2019? It’s producing p-aminophenol. You’re not saving money. You’re poisoning yourself.
Pharmacies are complicit. They hand you a bottle without context. No one teaches you how to read this stuff in school. This isn’t a labeling issue - it’s a cultural failure.
Rich Robertson December 20, 2025
Just got back from Cape Town - we don’t have AC in half the houses here, and people still take their ARVs like clockwork. They keep them in clay pots buried in the shade. It’s not fancy, but it works. Culture adapts. Regulations don’t always account for that.
Maybe the real solution isn’t smarter bottles - it’s smarter community support. Someone with a fridge should help someone without one. That’s the kind of innovation we need.
Jonny Moran December 21, 2025
My grandma used to keep her nitroglycerin in her purse. I thought she was nuts - till I read the label. Original bottle. Dark. Dry. She’s 84 and still hiking. That’s wisdom, not luck.
Thomas Anderson December 22, 2025
if you’re not sure, just ask your pharmacist. they’re not there just to hand you pills. they’re your free medical advisor. seriously, call them. it takes 30 seconds.
jeremy carroll December 23, 2025
omg i just checked my medicine cabinet and my insulin was in the door 😳 i’m moving it rn. thanks for the wake up call!!
Rulich Pretorius December 25, 2025
There is a deeper truth here: we treat our bodies like machines, yet we neglect the very tools that keep them running. The label is not a suggestion - it is a covenant between chemistry and life. To ignore it is to betray your own biology.
What we call ‘storage’ is, in fact, stewardship. And stewardship requires mindfulness. Not just of temperature, but of intention.
Daniel Wevik December 27, 2025
Proper storage isn’t about following rules - it’s about respecting the science behind your medication. If you’re skipping this step, you’re not just risking efficacy - you’re undermining the entire pharmacological process. This isn’t opinion. It’s pharmacokinetics.
Daniel Thompson December 27, 2025
I’ve noticed that people who don’t read labels also don’t read consent forms, terms of service, or nutrition facts. It’s not about medication - it’s about cognitive laziness. We’ve outsourced responsibility to corporations, and now we’re surprised when they fail us.
Sinéad Griffin December 28, 2025
THE GOVERNMENT IS HIDING THE TRUTH ABOUT MED STORAGE 😱 I heard from a friend who works at Walgreens - they’re being told to stop warning people about heat damage because it ‘confuses customers.’ This is why America’s health is collapsing. 💥🇺🇸
Natalie Koeber December 28, 2025
QR codes? lol. they’re just tracking us. next thing you know, your phone will report you to the FDA if you leave your pill bottle in the car. they’re turning meds into surveillance tech. #BigPharmaIsWatching
Wade Mercer December 30, 2025
If you’re storing meds wrong, you’re not just irresponsible - you’re a danger to society. People who don’t follow basic instructions shouldn’t be allowed to take prescription drugs. This isn’t a matter of education. It’s a matter of public safety.