Multiple Sclerosis is a chronic autoimmune disease where the body's immune system mistakenly attacks the central nervous system. Over 2.8 million people worldwide live with this condition, and in Australia alone, about 25,000 individuals are affected. Unlike infections where the immune system fights external threats, MS is a case of the body's defense system turning against itself. Imagine your nerves as electrical wires. The myelin sheath is like the plastic coating around those wires. When the immune system damages this coating, signals get scrambled or blocked, causing symptoms like numbness, vision problems, or trouble walking.
How the Immune System Attacks Your Nervous System
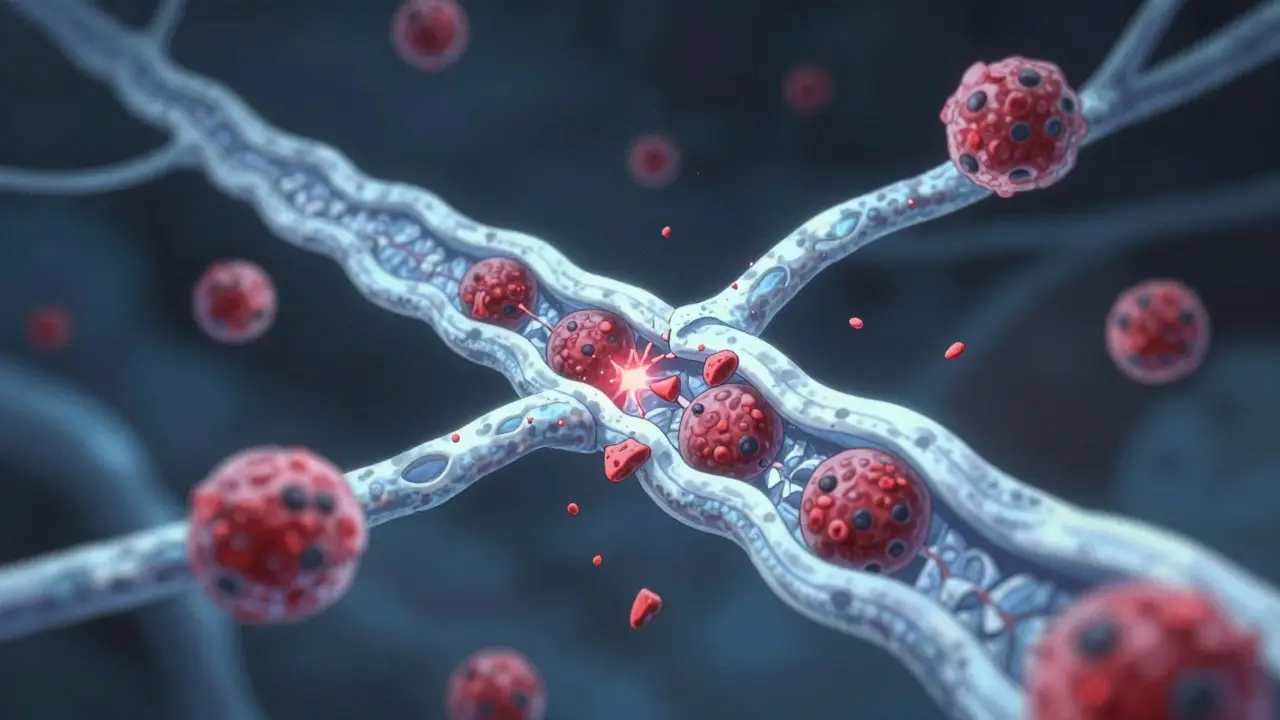
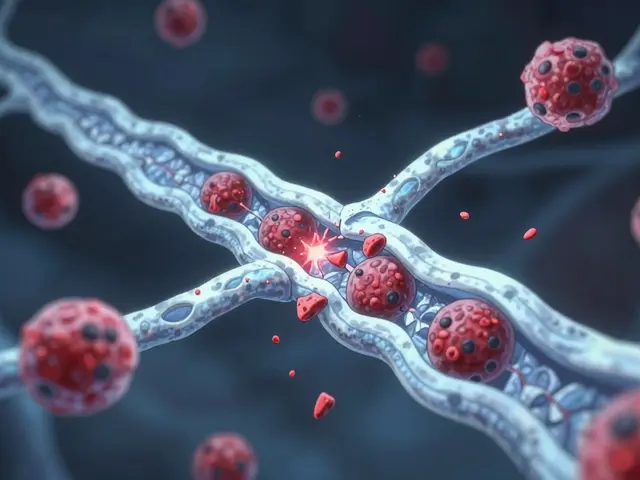
Multiple sclerosis begins when immune cells breach the blood-brain barrier-a protective layer that normally keeps harmful cells out of the brain and spinal cord. Once inside, these cells target the myelin sheath, the fatty insulation around nerve fibers. This process, called demyelination, disrupts electrical signals traveling along nerves.
Key players in this attack include CD4+ T cells and B cells. Research from the Paris Brain Institute shows that T cells become activated by myelin proteins, then travel to the central nervous system. There, they recruit other immune cells like macrophages and microglia. B cells contribute by producing antibodies and inflammatory cytokines. A 2023 study found B cells from MS patients produce 47% more TNF-α (a pro-inflammatory molecule) when exposed to interferon-gamma compared to healthy controls.
Over time, repeated attacks leave scar tissue (sclerosis), which further blocks nerve signals. This damage can occur in both white matter (where nerve fibers connect) and gray matter (where nerve cell bodies reside). The result? Communication between the brain and body breaks down.
Symptoms Explained by Nerve Damage
Symptoms of multiple sclerosis directly result from damaged myelin and nerve fibers. The location of damage determines what you experience. For example, optic neuritis-where the optic nerve's myelin is attacked-causes blurred vision or blindness in one eye over 24-48 hours. This affects 37% of MS patients, according to the Multiple Sclerosis Association of America.
- Fatigue: Affects 80% of people with MS. This isn't normal tiredness-it's an overwhelming exhaustion that makes daily tasks difficult.
- Numbness or tingling: Occurs in 58% of cases, often in limbs or face. This happens when sensory nerves lose their myelin coating.
- Walking difficulties: 42% of patients struggle with balance or coordination due to spinal cord damage.
A unique symptom called Lhermitte's sign causes electric shock sensations when bending the neck. This happens because demyelinated nerves in the cervical spine send abnormal signals when stretched. Patients on forums like Reddit often describe this as "a sudden jolt down the spine" during simple movements.
Triggers Behind the Autoimmune Attack
MS doesn't happen without a mix of genetic and environmental factors. Scientists have identified several key triggers:
- Epstein-Barr virus (EBV): A 2022 Harvard study found EBV infection increases MS risk by 32-fold. Nearly all MS patients have been exposed to EBV, suggesting it plays a critical role in triggering the autoimmune response.
- Vitamin D deficiency: People with serum levels below 50 nmol/L have a 60% higher risk of developing MS. This is why MS is more common in regions farther from the equator with less sunlight.
- Smoking: Smokers with MS experience 80% faster disease progression. Quitting can slow this decline significantly.
Genetics also play a role. Having a parent with MS increases your risk by 2-3%, but it's not a simple inheritance pattern. Over 200 genes are linked to MS susceptibility, many related to immune function.
Current Treatments Targeting the Immune System
Disease-modifying therapies (DMTs) are the cornerstone of MS treatment. These drugs target specific parts of the immune response to reduce attacks and slow progression:
- Ocrelizumab: Approved in 2017, this drug targets CD20+ B cells. In clinical trials, it reduced relapse rates by 46% compared to interferon beta-1a in relapsing MS and slowed disability progression by 24% in primary progressive MS.
- Natalizumab: This medication blocks immune cells from crossing the blood-brain barrier. It cuts annual relapses by 68%, but carries a 1 in 1,000 risk of progressive multifocal leukoencephalopathy (PML) after 24 months of treatment.
- Clemastine fumarate: An emerging treatment in clinical trials, this drug shows promise for remyelination. Phase II studies reported a 35% improvement in visual evoked potentials, indicating potential nerve repair.
Doctors now personalize treatment based on disease type, severity, and patient health. For example, natalizumab is typically reserved for severe cases due to PML risks, while ocrelizumab is used for both relapsing and progressive forms.

New Research on Repairing Nerve Damage
Current treatments focus on suppressing the immune system, but scientists are now targeting repair mechanisms. Recent breakthroughs include:
- Dendritic cell involvement: A 2025 study in Frontiers in Immunology found dendritic cells accumulate in perivascular regions of the brain in MS patients. These cells present myelin antigens to T cells, perpetuating inflammation. Targeting them could reduce neuroinflammation.
- Neutrophil extracellular traps (NETs): Elevated NET biomarkers were found in 78% of acute MS relapses. These NETs break down the blood-brain barrier and activate microglia, worsening damage.
- Serum neurofilament light chain (sNfL): This biomarker predicts disease activity. Levels above 15 pg/mL indicate active inflammation with 89% sensitivity, helping doctors adjust treatments early.
The International Progressive MS Alliance has invested $65 million in research since 2014. Projects across 14 countries aim to understand progressive MS mechanisms and develop remyelination therapies.
Living with MS Today
While MS is a lifelong condition, modern treatments have dramatically changed outcomes. Without treatment, 50% of relapsing-remitting MS patients need walking assistance within 15-20 years. With current DMTs, that number drops to about 30% at 20 years.
Many people with MS lead full lives with proper management. Physical therapy, occupational therapy, and lifestyle adjustments like stress reduction and exercise help maintain mobility and independence. Support groups and online communities-like those on Reddit's r/MS-provide invaluable emotional and practical support.
Early diagnosis and treatment are crucial. If you experience symptoms like vision changes, numbness, or unexplained fatigue, see a neurologist. Early intervention can prevent irreversible nerve damage and improve quality of life.
Is multiple sclerosis curable?
No, there's currently no cure for MS. However, disease-modifying therapies (DMTs) can significantly slow progression and reduce relapse rates. For example, ocrelizumab lowers relapses by 46% in relapsing MS and slows disability progression by 24% in primary progressive MS. Research into remyelination therapies, like clemastine fumarate, offers hope for future treatments that repair nerve damage.
What causes multiple sclerosis?
MS results from a combination of genetic susceptibility and environmental triggers. Key factors include Epstein-Barr virus infection (which increases risk 32-fold), vitamin D deficiency (60% higher risk with low levels), and smoking (80% faster progression). Research shows nearly all MS patients have been exposed to EBV, suggesting it plays a critical role in triggering the autoimmune response.
How does MS affect the nervous system?
In MS, immune cells attack the myelin sheath-the protective coating around nerve fibers in the brain and spinal cord. This demyelination disrupts electrical signals, causing symptoms like numbness, vision problems, and mobility issues. Over time, repeated attacks lead to scar tissue (sclerosis) and axonal damage, which can result in permanent disability. The National Multiple Sclerosis Society confirms that nerve damage is the primary cause of MS symptoms.
Can lifestyle changes help with MS?
Yes, lifestyle changes can improve quality of life and slow progression. Quitting smoking reduces progression risk by 80%, while maintaining vitamin D levels through sunlight or supplements lowers relapse rates. Regular exercise, stress management, and a balanced diet also help manage symptoms. The Multiple Sclerosis Association of America recommends these strategies alongside medical treatment for optimal outcomes.
What's the latest research on MS?
Recent studies focus on repairing nerve damage and understanding immune triggers. Researchers identified dendritic cells in perivascular brain regions that perpetuate inflammation by presenting myelin antigens to T cells. Another discovery is neutrophil extracellular traps (NETs), which break down the blood-brain barrier and are elevated in 78% of acute relapses. The International Progressive MS Alliance is funding 47 projects globally to develop remyelination therapies and personalized treatment approaches.




Joyce cuypers February 6, 2026
This is such an important topic. I've been living with MS for 10 years and it's really hard. But knowing how the immune system attacks the nerves helps me understand what's happening. The myelin sheath is like the plastic coating around wires, right? When it's damaged, signals get scrambled or blockd. It's scary, but there's hope with new treatments. Thanks for sharing this info!
Nancy Maneely February 6, 2026
This article is full of lies. It's all the fault of the EUs policies. They're poisoning us with vaccins. The US needs to take action now. Why isn't anyone talking about this? Like, seriously, it's obvious. They're hiding the truth. This is why we need to stop trusting foreign countries.
Albert Lua February 8, 2026
I'm from the Philippines and I've seen how MS affects communities globally. It's amazing how much research is happening worldwide. We need more collaboration between countries to tackle this. I've met people from different cultures who are managing MS with traditional medicine alongside Western treatments. It's a great example of cultural exchange in healthcare.
Samantha Beye February 9, 2026
This is really helpful information. I appreciate the detailed breakdown of how MS works. It's good to know there are treatments available. I hope this helps others understand their condition better. Keep up the good work.
Phoebe Norman February 11, 2026
The demyelination process involves CD4+ T cells and B cells infiltrating the CNS the blood-brain barrier breach allows immune cells to attack myelin this leads to inflammation and axonal damage sNfL biomarkers are crucial for monitoring disease activity but no one cares about the real science just more fluff
Tehya Wilson February 12, 2026
The article presents a comprehensive overview of MS. However, the data lacks sufficient context regarding global disparities. The focus on Western medicine overlooks alternative treatments prevalent in other regions. This is a significant oversight. Further research is required.
lance black February 13, 2026
Great info! Keep pushing forward! There's hope! Stay strong!
Pamela Power February 15, 2026
This article is amateurish. Real scientists would know better. The author clearly has no grasp of immunology. Myelin sheath? Please. It's all about the glial cells. And why are they ignoring the role of gut microbiota? Pathetic.
anjar maike February 16, 2026
What about the role of EBV in MS? 🤔 I've read that it's a big factor. Also, what's the latest on remyelination therapies? 🌍🌍
Cole Streeper February 18, 2026
This is all a hoax. The real cause is 5G towers. They're using MS to control people. Why isn't the government talking about this? It's a cover-up. The CDC is hiding the truth. I have proof. Check out the links.
Arjun Paul February 18, 2026
The article fails to address the socioeconomic factors contributing to MS prevalence. A thorough analysis is required. The current research is superficial.
Katharine Meiler February 20, 2026
The demyelination process involves complex interactions between adaptive and innate immune responses. Current DMTs target specific pathways, but there's a need for more personalized approaches based on biomarkers like sNfL.
Danielle Vila February 21, 2026
This is all part of the Big Pharma agenda. They don't want a cure because it's too profitable. The real cause is chemtrails and vaccines. I've done my own research. Check out the studies on the internet. They're hiding the truth!
Thorben Westerhuys February 23, 2026
Oh my goodness... this is so heartbreaking
I can't believe how the immune system attacks itself
it's like the body is fighting against itself
the myelin sheath damage... it's just so tragic
but there is hope with new treatments
I just feel so sad for everyone...
Laissa Peixoto February 24, 2026
It's fascinating how the immune system, meant to protect us, becomes our enemy. The complexity of MS shows the delicate balance of our biology. Perhaps understanding this paradox can lead to better treatments. We must keep researching with compassion.