Postherpetic neuralgia can be a daunting term, but breaking it down reveals a condition that affects many people globally. Particularly, it arises in the aftermath of a shingles infection, where nerve damage takes control.
The journey from an irritating rash to persistent pain is often marked by several stages, each with its own challenges. Many people experience only the acute stage, while a significant number progress to chronic issues that linger, demanding a life of strategic management.
By understanding both the acute and chronic phases, sufferers are better equipped to handle the discomfort and find effective solutions to maintain their quality of life. The key lies in early intervention and employing evidence-based strategies to mitigate symptoms.
- Introduction to Postherpetic Neuralgia
- The Transition from Shingles to Neuralgia
- Understanding Acute Stage Symptoms
- Chronic Stage Complexities
- Managing and Alleviating Pain
Introduction to Postherpetic Neuralgia
Postherpetic neuralgia is more common than most people think, often sneaking into lives in the aftermath of what seems like a resolved affliction—shingles. This nerve pain condition can sometimes lurk beneath the shadows of a healed rash, presenting as persistent pain without rhyme or reason. But there is a good reason. Understanding it starts with shingles itself, a disease caused by the varicella-zoster virus, the same culprit responsible for chickenpox. After chickenpox runs its course, the virus doesn’t leave; it retreats into the nervous system, lying dormant sometimes for decades. It can reactivate, often in older adults or when immune systems weaken, leading to a painful, blistering rash known as shingles.
Shingles are typically localized, often to one side of the face or body, its infamy captured in tales of burning and itchy discomfort. Yet, for many, the true trial begins after the rash subsides. Postherpetic neuralgia sets in when nerve fibers have suffered damage and become confused, their signals to the brain exaggerated, producing intense, incurable pain. This chronic pain can manifest where the shingles rash once lay, lasting months, years, or, for some, indefinitely. A survey from the Mayo Clinic found that about 15% to 20% of those with shingles develop postherpetic neuralgia. This statistic climbs steeply for seniors, with 10% to 18% of adults over 60 experiencing the long-term nerve pain.
A significant factor in determining the risk is age. The older a person is when shingles strikes, the more likely they are to experience postherpetic neuralgia. This condition doesn't discriminate by sex or race, showing a ubiquitous presence across all demographics. While women and men seem equally affected by shingles, women may be more vulnerable to the development of postherpetic neuralgia. Recognizing these patterns allows for early interventions and can guide the therapeutic strategies used to mitigate its impact.
“The herculean challenge in managing postherpetic neuralgia doesn’t just lie in the pain but in understanding its mechanism - a hyperactive nerve network gone askew,” says Dr. Laura Stone, a renowned researcher in neural pathologies.
Medically, several tools are employed to understand and manage this vexing condition. MRI scans and nerve conduction studies may be utilized to assess the extent of nerve damage. Early engagement with healthcare providers is crucial, as treatment initiated within 72 hours of the onset of shingles rash is shown to reduce the likelihood and severity of the chronic condition. Knowing the potential for shingles to turn into postherpetic neuralgia emphasizes the need for preventive measures, like the shingles vaccine, recommended for individuals over 50. In a study published in the New England Journal of Medicine, the vaccine reduced the incidence of shingles by about 50% and also lessened the risk for subsequent neurogenic pain.
The Transition from Shingles to Neuralgia
The path from having shingles to developing postherpetic neuralgia is not a simple one, often marked by complexities that catch many by surprise. Shingles itself starts with an itchy, blister-like rash caused by the reactivation of the varicella-zoster virus, the same culprit behind chickenpox. Most people who contract shingles arrive at varying degrees of pain and discomfort during the course of the affliction, but for some, the pain lingers well after the blisters have subsided. This persistence of pain ushers in the condition known as postherpetic neuralgia, mainly driven by nerve damage sustained during the viral attack.
In a fascinating transition, nerve endings affected during a shingles outbreak become hypersensitive. It's as though these nerves reset themselves to a new normal, amplifying even the most benign stimuli into excruciating pain. This transition from acute to chronic pain doesn't occur overnight; it is a gradual process for many individuals. The acute phase of shingles might induce severe burning or stabbing sensations, but when it morphs into a chronic issue, the situation becomes emotionally and physically draining. The nerves scream pain signals even when there's no obvious injury. Studies suggest that about 10 to 18 percent of shingles patients will confront postherpetic neuralgia.
"The lasting impact of postherpetic neuralgia is vastly underestimated and misunderstood," remarks Dr. Cheshire from the Mayo Clinic, emphasizing how the neuralgia prolongs suffering for many.
An intriguing aspect of this transition lies in the role of the immune system. An overly aggressive response to the virus may inadvertently contribute to nerve damage. Factors such as age, pre-existing health conditions, and even the intensity of the original shingles outbreak can influence whether someone moves on to develop chronic nerve pain. People over 60 have a higher predisposition toward experiencing this transition, partly due to changes in immune response capabilities as the body ages. As these processes unfold, the quality of life can seriously diminish; simple activities become daunting when pain is a constant companion.
Managing this transition is crucial. Doctors often recommend early intervention strategies during the acute phase of shingles, which can help minimize the risk of progression to neuralgia. These include antiviral medications to quell the virus and pain management strategies—like nerve blockers and analgesics—that curtail both inflammation and pain transmission. By addressing the pain early, it's sometimes possible to significantly reduce or even prevent the chronic stage from taking hold. In addition to pharmacological approaches, complementary therapies such as acupuncture or physical therapy might also help in mitigating severe symptoms.
Understanding Acute Stage Symptoms
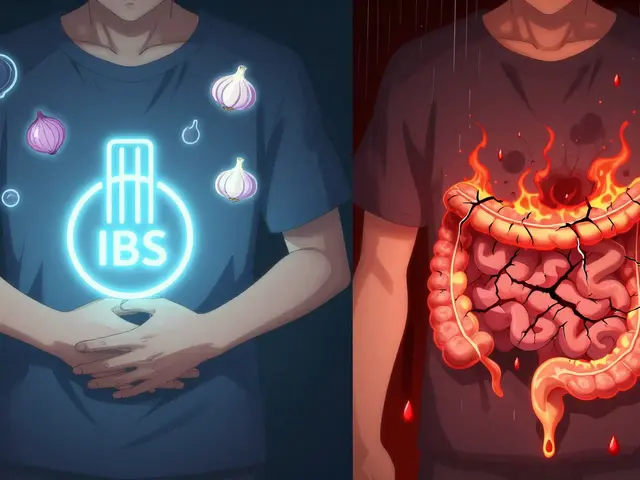
When it comes to Postherpetic Neuralgia (PHN), the acute stage is the initial threshold at which sufferers first experience the distinct aftershocks of a shingles infection. This stage usually manifests just after the shingles rash begins to heal, yet the discomfort it brings can be profoundly intense. Nerve fibers that have been damaged by the viral infection start sending mixed signals to the brain, often resulting in a sharp, burning sensation that lingers long after the blistered rash has disappeared.
Acute PHN differs from general nerve pain as it can cause a debilitating sensitivity that appears to linger disproportionately compared to visible symptoms. People often describe this stage as having areas of their skin that are both numb and excruciatingly sensitive at the same time. Compounding the issue, regular touches or gentle pressure, such as clothes brushing against the skin, can provoke heightened pain sensations, making even simple daily tasks a challenge. An intriguing aspect of the acute stage is its unpredictable nature; someone might feel only minor discomfort for some time, only to suddenly experience intense pain spikes.
Many individuals report difficulty sleeping and constant discomfort, which can severely impede daily functioning and overall quality of life. This kind of nerve pain is sometimes called "allodynia," a condition where innocuous stimuli cause pain. This unpleasant sensation isn't confined to a small area; it may spread along the nerve path in question, which in shingles usually means across areas supplied by affected nerves, often involving the torso. This unpredictability is a hallmark of the acute symptoms of PHN and one that confounds many patients and physicians alike, often delaying effective management strategies. As Dr. Kent Todd from the Pain Research Foundation famously said,
"Individuals affected by postherpetic neuralgia tend to find themselves in a perplexing cycle of managing pain signals that the brain insists are real, even when the skin appears healed."
Several studies suggest strategies to tackle or at least minimize these acute symptoms early on. First-line options often include antiviral medications prescribed during the initial shingles outbreak to attempt shortening the virus's duration and limit nerve damage. However, once in the acute PHN stage, patients might find additional help through topical treatments – such as capsaicin cream, which is manufactured from chili peppers and may help desensitize nerve endings over time. Another important therapy option includes numbing patches, particularly those containing lidocaine, which can provide direct relief to troublesome skin areas, effectively easing pain.
Data from various health research reports shows that about 20% of individuals above the age of 50 who suffer from shingles end up developing PHN, emphasizing the importance of early intervention. It is crucial for healthcare providers to advocate for vaccination against shingles, as this can be an effective preventive measure against PHN. Understanding these early symptoms and responses allows patients and doctors alike to attack the pain from every angle, ensuring a strategic battle plan is in place. By focusing on comprehensive management approaches, it is possible to reduce the impact of the acute stage, paving the way for smoother sailing through the chronic phases that may follow.
Chronic Stage Complexities
When discussing the chronic stage of Postherpetic Neuralgia, it is important to realize just how deeply this condition can affect an individual's daily life. Chronic pain, by nature, is unyielding, persisting for months or even years after the initial shingles outbreak has healed. Individuals often describe it as a constant burning or aching pain, occasionally punctuated by sharp, jolting pain, affecting not just the physical but emotional and mental states as well.
The mechanisms that underpin this relentless nerve pain stem from the damage inflicted upon sensory nerve fibers during the initial viral infection. This damage leads to the misinterpretation of normal stimuli as painful, a condition known as allodynia. In many cases, the skin becomes extraordinarily sensitive, eliciting pain from mere touches or changes in temperature that wouldn't normally cause discomfort. This hypersensitivity can leave individuals grappling with both the physiological discomfort and the psychological toll it brings.
Compounding these challenges is how the chronic nature of the pain often leads to additional complications such as insomnia, weight loss, social withdrawal, and depression. For many, the struggle is not merely about controlling the pain but also managing the ripple effects it has across various facets of life. A study conducted by the University of Oxford noted that around 20% of patients with Postherpetic Neuralgia report a substantially reduced quality of life, often attributing this not just to the intensity of pain, but its persistence.
"Chronic pain can overshadow one's entire existence, turning once simple tasks into formidable challenges," remarks Dr. Julia Harris, a specialist in chronic pain management.
One of the key strategies to managing chronic Postherpetic Neuralgia effectively is adopting a multifaceted approach. This often involves a combination of medications, such as anticonvulsants or tricyclic antidepressants, physical therapy, and psychological support. Each plays its part in addressing the diverse ways this condition impacts an individual. By treating both the symptoms and the emotional fallout, patients may find a noticeable improvement in their day-to-day functioning.
Another critical element to chronic pain management is lifestyle adaptation. This means making incremental, patient-specific changes to daily habits and routines. Practicing mindfulness or meditation can help in developing a healthier response to pain, while maintaining regular physical activity can alleviate some of the stiffness and discomfort associated with the condition. Exploring alternative therapies, like acupuncture, has provided relief for some patients, though effectiveness can vary.
- Medications, including nerve pain medications like Gabapentin or Pregabalin.
- Alternative therapies, which can include acupuncture and massage therapy.
- Behavioral strategies to manage emotional health.

Managing and Alleviating Pain
Tackling the pain from postherpetic neuralgia requires both a strategic approach and a bit of patience. It’s the kind of journey where endurance and adaptability play a big role. Managing this persistent nerve pain isn’t just about popping pills; it’s a comprehensive plan that takes into account the uniqueness of your body’s response to therapy. Different people react differently, so it often involves trying various approaches until you find the one that works best. The goal is to not only reduce pain but also regain control over your life, allowing you to participate in activities you enjoy without being hindered by discomfort.
People with chronic pain from this condition often benefit from a combination of medications and non-drug therapies. Prescription medications might include antiepileptic drugs such as gabapentin or pregabalin, which are known to calm nerve activity. Antidepressants, particularly tricyclics, have been found effective too, even for those without depression, due to their ability to alter the brain's way of processing pain signals. Topical treatments like lidocaine patches or capsaicin cream can be directly applied to painful areas, providing localized relief. The pursuit of relief doesn't stop at the pharmacy or doctor’s office; incorporating holistic practices is increasingly recognized as a valuable component of pain management.
On the holistic front, regular exercise can't be overstated. Engaging in low-impact aerobic activities like swimming or walking increases endorphin levels, which naturally counteract pain. Stretching as part of a daily regime can help prevent muscle stiffness that often accompanies chronic pain. Moreover, practices such as yoga or tai chi can improve flexibility and balance, while also mentally preparing individuals to better cope with pain levels. But beyond physical activity, mental therapies too hold significant value. Cognitive-behavioral therapy (CBT) has been shown to effectively shift the focus from pain, enabling sufferers to challenge negative thoughts and develop coping strategies. In the words of Dr. Smith, a well-respected neurologist, "Pain is a complex experience, and understanding its psychological component is half the battle in finding relief."
Patients are encouraged to keep a pain diary. By documenting pain levels and any associating factors on a daily basis, it's easier to identify triggers or effective relief strategies over time. Diet also plays a role that shouldn’t be overlooked. A balanced diet rich in omega-3 fatty acids can contribute positively and possibly reduce inflammation, indirectly impacting nerve pain. It’s crucial for patients to discuss any new dietary changes or supplement use with their healthcare provider to ensure there are no interactions with their treatment regimen.
The importance of an adequate support system cannot be understated. Actively involving family and friends in the journey helps to create a psychological buffer against potential hopelessness. Joining support groups, either online or locally, can offer emotional experiences shared by others and assure individuals that they are not alone in their hardships. It's crucial to understand that managing nerve pain is a marathon, not a sprint. Consistency, alongside an open mind towards trying different strategies, is often key to experiencing significant improvement and achieving a fulfilling life despite the challenges.






Manju priya January 22, 2025
Early intervention is the cornerstone of preventing chronic postherpetic neuralgia, and the shingles vaccine remains one of the most effective tools we have. By vaccinating individuals over the age of 50, we can significantly reduce both the incidence of shingles and the subsequent risk of neuralgia. Moreover, prompt antiviral therapy within 72 hours of rash onset can limit nerve damage and improve outcomes. Stay proactive and consult your healthcare provider about vaccination today 😊
Jesse Groenendaal February 3, 2025
We have a moral duty to inform everyone that delaying treatment is simply irresponsible it prolongs suffering and burdens the healthcare system. It is unacceptable to ignore the proven benefits of early antiviral use and vaccination.
Persephone McNair February 14, 2025
From a neurophysiological perspective the hyperexcitability of dorsal root ganglion neurons post‑VZV reactivation underlies the allodynia and hyperalgesia observed in PHN patients. The upregulation of sodium channel Nav1.7 and the maladaptive plasticity of central pain pathways constitute a maladaptive sensitization loop. This mechanistic insight underscores the importance of targeted pharmacologic modulation early in the disease course.
siddharth singh February 26, 2025
Let me lay out a comprehensive framework for managing postherpetic neuralgia that integrates pharmacologic, interventional, and lifestyle strategies. First, antiviral agents such as famciclovir or valacyclovir should be commenced within the first 72 hours of rash onset to curtail viral replication and limit neuronal injury. Second, for patients who progress to the acute pain phase, initiating a gabapentinoid like gabapentin can attenuate ectopic firing of damaged afferents. Third, a tricyclic antidepressant such as amitriptyline may be added to address both neuropathic pain and comorbid insomnia. Fourth, topical lidocaine patches or high‑concentration capsaicin can provide localized analgesia with minimal systemic side effects. Fifth, consider nerve blocks or epidural steroid injections for refractory cases, which can interrupt the peripheral sensitization cascade. Sixth, physical therapy focused on gentle range‑of‑motion exercises helps preserve function and prevents secondary musculoskeletal complications. Seventh, incorporate mindfulness‑based stress reduction or cognitive‑behavioral therapy to address the emotional burden of chronic pain, which can amplify nociceptive signals. Eighth, ensure adequate nutrition rich in omega‑3 fatty acids and antioxidants, as systemic inflammation can exacerbate neural hyperexcitability. Ninth, regular aerobic activity such as brisk walking or swimming promotes endogenous endorphin release, which naturally modulates pain perception. Tenth, maintain a detailed pain diary to identify triggers, efficacy of interventions, and temporal patterns, thereby empowering both patient and clinician to fine‑tune the regimen. Eleventh, screen for depression and anxiety, because untreated mood disorders can significantly worsen pain outcomes and reduce adherence to therapy. Twelfth, explore complementary modalities like acupuncture or low‑level laser therapy, which have shown modest benefits in some trials. Thirteenth, educate patients about the importance of sleep hygiene, as fragmented sleep can heighten pain sensitivity through dysregulation of descending inhibitory pathways. Fourteenth, engage family members and support groups to provide social reinforcement, reducing isolation and fostering resilience. Finally, schedule regular follow‑up visits to reassess pain levels, medication side effects, and functional status, ensuring the management plan remains dynamic and patient‑centered. By adhering to this multimodal algorithm, clinicians can substantially improve quality of life for individuals suffering from both acute and chronic phases of postherpetic neuralgia.
Angela Green March 9, 2025
The information presented is thorough and well‑structured; I especially appreciate the clear separation of acute versus chronic management strategies. It is essential to emphasize that early antiviral therapy is not merely optional but evidence‑based. Additionally, the inclusion of lifestyle interventions rounds out a holistic approach. Thank you for the detailed overview.
April Malley March 21, 2025
Absolutely, I completely agree, the multimodal plan really covers every angle, from meds, to physical therapy, to diet, and even mental health, it's a solid strategy, and I think anyone dealing with PHN will find it incredibly helpful, great job on summarizing it all, keep it up!
scott bradshaw April 2, 2025
Oh great another miracle cure for nerve pain.
Crystal Price April 13, 2025
Isn't it fascinating how we chase quick fixes while the real battle is within? The pain becomes a teacher, showing us the fragility of our bodies and the strength of our spirits.
Murhari Patil April 25, 2025
What they don't tell you is that the so‑called "vaccines" are part of a larger agenda to control not just disease but also the narrative around suffering, keeping us distracted while larger forces manipulate the data and the options we have for real relief.