Medication Safety Risk Calculator
Assess Your Medication Risk
Risk Assessment Results
Select a medication and enter dosage/duration to see risk assessment.
Most people assume that if a medication is approved by the FDA, it’s safe for everyone. But the truth is, some drugs don’t just treat your illness-they can quietly damage your organs. Organ-specific side effects aren’t rare accidents. They’re predictable, measurable, and often missed until it’s too late. Every year, over 2 million serious reactions happen in the U.S. because of these hidden risks. And the liver, kidneys, heart, and nervous system are the most common targets.
Liver Damage: The Silent Killer
Your liver processes almost every drug you take. That makes it the most vulnerable organ. Acetaminophen, the active ingredient in Tylenol, is the leading cause of acute liver failure in the U.S. Taking just 7.5 to 10 grams in one day-less than 20 regular tablets-can overwhelm your liver’s detox system. The result? A toxic byproduct called NAPQI builds up, destroying liver cells. Around 56,000 ER visits each year are due to accidental overdose. But it’s not just overdoses. Even normal doses can hurt. Isoniazid, used to treat tuberculosis, causes liver injury in 1 to 2% of people. The risk spikes if you’re a slow acetylator-a genetic trait that slows how fast your body breaks down the drug. Statins, taken by millions for cholesterol, raise liver enzymes in up to 2% of users. That doesn’t always mean damage, but if ALT levels jump more than three times the normal limit, doctors are trained to stop the drug. Symptoms? Fatigue, nausea, dark urine, or yellowing skin. But here’s the problem: 68% of people who develop drug-induced liver injury don’t notice anything until four to eight weeks in. By then, the damage is often advanced. New blood tests for microRNA-122 and keratin-18 fragments can now detect liver cell death three to five days earlier than traditional liver enzyme tests. That’s a game-changer for catching problems before they become life-threatening.Kidney Injury: When Your Filters Fail
Your kidneys don’t just make urine-they filter toxins out of your blood. And many drugs don’t care. Aminoglycoside antibiotics like gentamicin are notorious. Up to half of patients on long-term treatment develop kidney damage. The drug sticks to receptors in the kidney’s tubules, wrecking mitochondria and causing cells to die. NSAIDs like ibuprofen and naproxen are even more insidious. They’re over-the-counter, so people think they’re harmless. But in people over 65, ibuprofen alone is linked to 15% of all acute kidney injury cases. These drugs reduce blood flow to the kidneys, and if you’re dehydrated or already have kidney trouble, that’s enough to trigger failure. Contrast dye used in CT scans causes kidney injury in 2 to 15% of patients-with rates jumping to 50% if you already have poor kidney function. Vancomycin, a powerful antibiotic, is another culprit. When blood levels go above 15 mg/L, the risk of kidney damage rises sharply. For every extra 5 mg/L above that, the risk increases by 30%. And here’s the kicker: 44% of patients with NSAID-related kidney injury don’t feel a thing until a routine blood test shows their creatinine is high. Doctors now use new biomarkers like TIMP-2 and IGFBP7 to spot kidney stress before creatinine rises. These tests can warn of injury within hours, not days. But most hospitals still rely on outdated blood tests. If you’re on long-term NSAIDs, diuretics, or antibiotics, ask for an eGFR check every three months. If your eGFR drops below 60, your meds may need adjusting.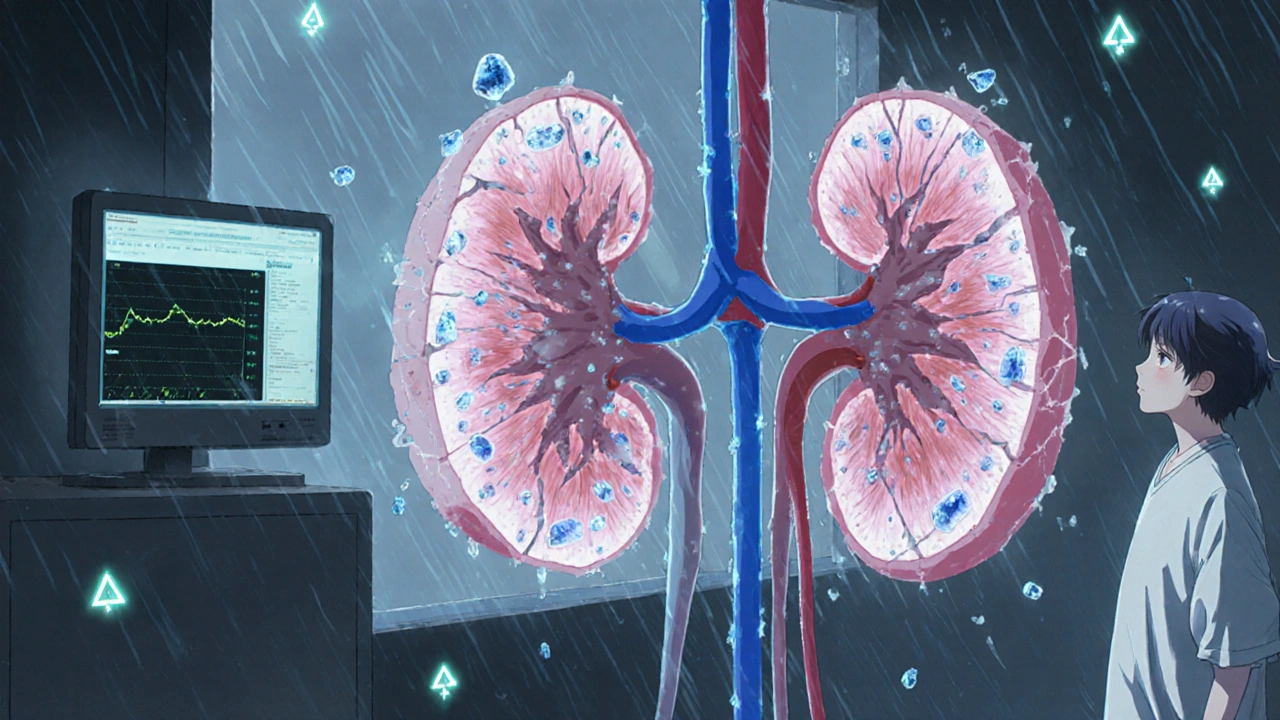
Heart Risks: From Arrhythmias to Heart Failure
Some drugs don’t just affect your heart rhythm-they can permanently weaken it. Doxorubicin, a chemotherapy drug used for breast cancer and lymphoma, causes heart failure in up to 26% of patients who receive more than 450 to 500 mg per square meter of body surface. The damage comes from iron-driven free radicals that attack heart muscle cells. That’s why oncologists track your left ventricular ejection fraction (LVEF) every few months during treatment. If your LVEF drops below 45% or falls more than 15 points from baseline, they stop the drug. Immune checkpoint inhibitors-new cancer drugs like pembrolizumab-are a different kind of threat. They can trigger myocarditis, an inflammation of the heart muscle. It’s rare-only 1% of patients get it-but when they do, 40 to 50% die. Symptoms? Chest pain, shortness of breath, swelling in the legs. And it often hits within the first 90 days of treatment. Antipsychotics like haloperidol and ziprasidone can stretch your heart’s electrical system. They prolong the QT interval on an ECG, which can lead to a deadly arrhythmia called torsades de pointes. Ziprasidone adds an average of 16.4 milliseconds to the QT interval-more than double risperidone’s effect. Fluoroquinolone antibiotics like ciprofloxacin raise the risk of aortic aneurysms by 31% if taken for more than 60 days. That’s because they weaken collagen in blood vessel walls. If you’re on any of these drugs and suddenly feel dizzy, have palpitations, or get out of breath with minimal effort, don’t wait. Get an ECG and an echocardiogram. Early detection saves lives.Neurologic Damage: Memory, Nerves, and Movement
Your brain and nerves are sensitive. Some drugs attack them slowly, over years. Proton pump inhibitors (PPIs)-like omeprazole and pantoprazole-are taken daily by tens of millions for heartburn. But long-term use (over 4.4 years) increases dementia risk by 21%. The mechanism isn’t fully clear, but it may involve changes in brain vitamin B12 levels or increased amyloid buildup. Chemotherapy drugs like cisplatin and oxaliplatin cause nerve damage in up to 70% of patients. Cisplatin leads to permanent numbness and tingling in fingers and toes. Oxaliplatin is worse-it triggers acute, freezing pain during infusion. Patients describe it like “screwing a lightbulb with bare hands in a freezer.” Phenytoin, an old-school seizure drug, can cause cerebellar atrophy in 15 to 40% of long-term users. That means loss of balance, slurred speech, and shaky hands. The damage shows up on MRI scans and doesn’t always reverse, even after stopping the drug. Immune checkpoint inhibitors also hit the nervous system. They can cause Guillain-Barré syndrome, myasthenia gravis, and encephalitis. These are rare-under 1% of patients-but they’re deadly if not caught fast. Symptoms? Weakness that spreads upward, double vision, trouble swallowing, or sudden confusion. If you’re on long-term PPIs or chemo, ask your doctor about cognitive testing or nerve conduction studies. Don’t assume memory lapses are just aging. They might be medication-induced.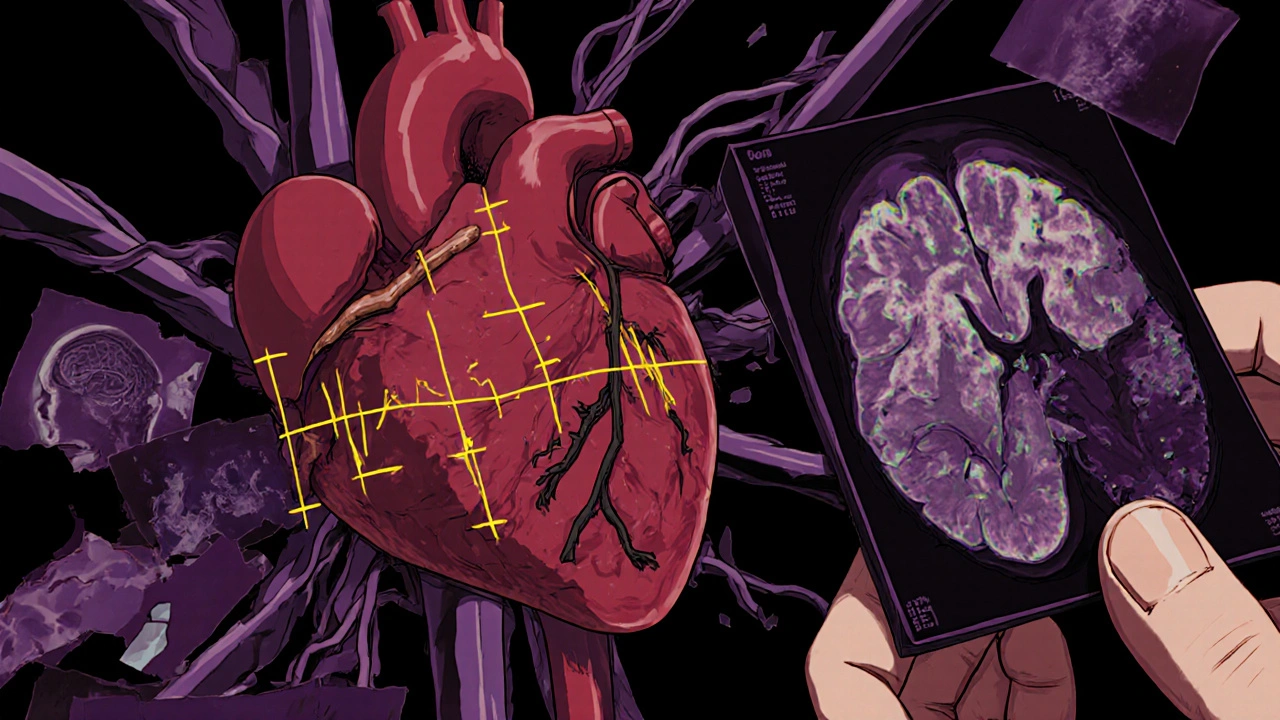
How to Protect Yourself
You can’t avoid all risks-but you can reduce them. Here’s how:- Know your meds. Ask your pharmacist: “Which organs does this drug affect?”
- Track symptoms. Fatigue, dark urine, swelling, numbness, chest pain-don’t ignore them.
- Get baseline tests. Before starting a new drug, ask for liver enzymes, kidney function (eGFR), ECG, and possibly a neurologic exam.
- Don’t assume OTC is safe. NSAIDs, PPIs, and even herbal supplements can harm your organs.
- Ask about alternatives. Is there a drug with less organ toxicity? For example, some statins are less likely to cause liver issues than others.
- Use monitoring. If you’re on high-risk drugs, schedule regular blood tests every 3 to 6 months.







Shana Labed October 30, 2025
This is the kind of post that should be mandatory reading for every adult on the planet. I didn't realize how many OTC drugs are basically slow-motion poison for my organs. I've been taking ibuprofen like candy for my migraines-time to talk to my doc about alternatives. Also, microRNA-122? That’s wild. We’re living in the future, y’all.
Also, if you’re on PPIs longer than a year, you’re basically playing Russian roulette with your brain. Stop. Just stop.
California Daughter October 30, 2025
Wait-so you’re saying… NSAIDs… are dangerous? And… acetaminophen? That’s… like… the only thing I take? And… I thought… it was safe? So… what am I supposed to do? Cry? And… also… who approved this? I mean… really…?
Vishwajeet Gade October 31, 2025
USA always exaggerate. In India, we take 10 paracetamol daily and still run marathons. Your liver? Weak. Your medicine? Overregulated. You think your body can't handle a little toxicity? Ha! We have real problems-no clean water, no doctors. You worry about ALT levels? Pathetic.
Also, PPIs cause dementia? Lol. My grandma takes omeprazole since 2005 and still beats me at chess. Your science is trash.
Casey Crowell November 1, 2025
Bro. I just got my first ECG after starting ziprasidone and my QT was 480ms. I panicked. Went to the ER. They said ‘yeah, that’s high, but we’ve seen worse.’
Then I found out my doc didn’t even know about the new TIMP-2 biomarkers for kidneys. I had to Google it and show him. 🤦♂️
Point is: if you’re on meds longer than 3 months, you’re your own best advocate. Don’t wait for a crisis. Ask for the tests. Use emojis if you have to. 🩺💔🧠
Shanna Talley November 2, 2025
This post gave me chills. I used to think meds were just pills. Now I see them as tiny architects of my body’s future.
It’s not about fear. It’s about awareness. If you’re taking something daily for years, you owe it to yourself to know how it’s changing you.
Ask questions. Get tested. Listen to your body. You’re not being paranoid-you’re being wise.
And if you’re a doctor reading this? Please, stop treating patients like numbers.
We’re humans. With organs. And stories.
Samuel Wood November 3, 2025
Let’s be honest-this article reads like a pharmaceutical fearmongering manifesto masquerading as medical advice. The data is cherry-picked, the tone is alarmist, and the ‘solutions’ are laughably simplistic. You think asking your pharmacist about ‘organ toxicity’ is going to save you? Please. The FDA doesn’t even regulate supplements. Your ‘baseline tests’ are meaningless without context.
Also, organ-on-chip tech? Cute. But it’s still in labs. Meanwhile, real patients are being denied care because of cost. Your ‘game-changing’ biomarkers? Unaffordable. This isn’t science-it’s performative outrage.
Jacqueline Anwar November 4, 2025
It is deeply concerning that the public is being led to believe that the mere presence of a pharmaceutical agent in the bloodstream constitutes an imminent threat to vital organ systems. The author’s rhetoric is alarmist, statistically selective, and emotionally manipulative. The fact that 56,000 ER visits occur annually due to acetaminophen does not imply systemic failure-it implies behavioral failure.
Furthermore, to suggest that patients should routinely request microRNA-122 assays is not only impractical, it is medically irresponsible. We do not screen for every theoretical risk. We weigh benefit against harm-and in most cases, the benefit remains overwhelmingly favorable.
This article does not inform. It incites.
Ganesh Kamble November 5, 2025
LOL so now we're scared of every drug ever made? I take metformin, lisinopril, and aspirin daily. My liver enzymes? Normal. My kidneys? Fine. My heart? Beats like a drum.
Next you'll say coffee kills your pancreas. Or breathing kills your lungs.
Also, 'ask your pharmacist'? What, like they know more than your MD? Please. This is just fear porn wrapped in fancy jargon.
Jenni Waugh November 5, 2025
Oh, so now we’re supposed to be terrified of every pill in our cabinet? Let me guess-the next article is going to tell us that sunlight causes skin cancer and water causes kidney stones?
And you think a 21% increase in dementia risk from PPIs is a crisis? That’s like saying eating chocolate increases your risk of winning the lottery. It’s statistically there-but it’s not a reason to stop living.
Also, ‘don’t assume memory lapses are aging’? Honey, I’m 68. My memory is gone. I don’t need a drug to blame. I need a nap.
And yes, I’m being sarcastic. Because this post is a masterpiece of overblown anxiety.