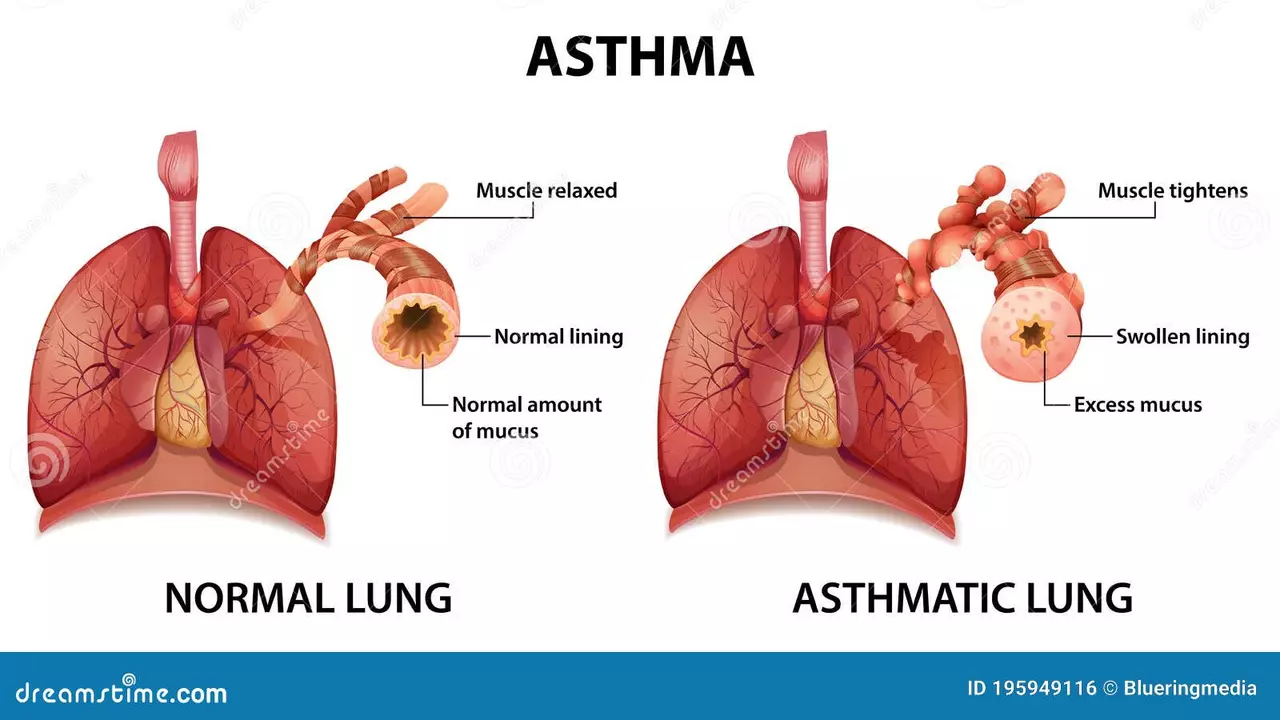
Understanding Lung Inflammation
Before diving into the importance of regular checkups, it's crucial to understand what lung inflammation is. In simple terms, lung inflammation is a condition where your lungs and airways become swollen and filled with fluid or pus. This can lead to a variety of symptoms like coughing, shortness of breath, and chest pain. The most common causes of lung inflammation include infections, such as pneumonia and bronchitis, and chronic diseases like asthma and chronic obstructive pulmonary disease (COPD). The severity of lung inflammation can vary greatly and if left untreated, it can lead to serious complications and even death.
Why Regular Checkups Matter
Regular checkups play a vital role in maintaining good health. These checkups allow your doctor to detect potential health issues before they become severe problems. With lung inflammation, early detection is particularly important. The sooner lung inflammation is identified and treated, the better the outcomes are likely to be. Regular checkups also provide an opportunity for your doctor to provide advice on lifestyle changes that can help prevent lung inflammation, such as quitting smoking or improving your diet.
Early Signs of Lung Inflammation
Knowing the early signs of lung inflammation can help you understand when to seek medical attention. These symptoms often include persistent coughing, difficulty breathing, chest pain, and fatigue. It's important to pay attention to these signs and seek immediate medical attention if you experience any of them. Also, if you're at a higher risk of developing lung inflammation, for example, if you're a smoker or have a family history of lung disease, it's even more important to keep a close eye on your health.
Checkups and Diagnosis
Detecting lung inflammation early often requires a range of tests which are usually conducted during regular checkups. These may include a physical examination, chest X-rays, CT scans, lung function tests, and blood tests. Your doctor will use these tests to assess your lung health and determine whether there's any inflammation. While these tests may seem daunting, they're crucial for early diagnosis and effective treatment of lung inflammation.
Treatment and Management of Lung Inflammation
Once lung inflammation is diagnosed, treatment usually involves managing the symptoms and treating the underlying cause. This may include medication to reduce inflammation, antibiotics to treat infections, or lifestyle changes such as quitting smoking or avoiding allergens. Regular checkups are vital here too, as they allow your doctor to monitor your condition and adjust treatment as necessary. Remember, successful management of lung inflammation often requires a long-term commitment to regular checkups and treatment.
Prevention is Better Than Cure
Lastly, it's important to remember the adage that prevention is better than cure. While regular checkups are vital for early detection and treatment of lung inflammation, adopting a healthy lifestyle can help prevent this condition in the first place. This includes quitting smoking, eating a balanced diet, exercising regularly, and avoiding exposure to harmful substances. Regular checkups are also a key part of prevention, as they allow your doctor to provide advice on how to reduce your risk of lung inflammation.





sharon rider July 16, 2023
I think many people overlook how subtle lung inflammation can be until it escalates. A quiet cough or occasional shortness of breath might be dismissed as a cold, but those are often early warnings. Regular checkups catch these signs before they turn into chronic issues. It also gives doctors a chance to discuss lifestyle tweaks that can protect lung health. Keeping an eye on your breathing patterns is a simple act of self‑respect.
swapnil gedam July 16, 2023
Adding to that, routine spirometry can reveal declines in lung capacity that you wouldn't notice day‑to‑day. Even a slight dip in FEV1 may hint at inflammation brewing beneath the surface. The nice thing about regular visits is that doctors can schedule follow‑ups tailored to your risk factors. If you smoke, those appointments become crucial checkpoints. And for those with a family history, early imaging can be lifesaving.
Michael Vincenzi July 16, 2023
Regular check‑ups are more than just a box to tick; they’re a proactive shield against the silent creep of lung inflammation. When you sit down with a clinician, they’ll start with a straightforward physical exam, listening for any atypical breath sounds that could signal trouble. From there, a chest X‑ray offers a quick visual snapshot, while a CT scan can dig deeper, revealing subtle tissue changes that plain films might miss.
Beyond imaging, pulmonary function tests measure how well air moves in and out of your lungs, giving quantifiable data on any obstruction or restriction. Blood work can highlight elevated inflammatory markers, which, combined with your symptom history, paints a clearer picture. If those tests flag anything, early intervention becomes possible-whether that’s a short course of steroids, targeted antibiotics, or simply a change in daily habits.
Speaking of habits, quitting smoking is arguably the single most effective prevention strategy. Even reducing exposure to secondhand smoke or indoor pollutants can make a measurable difference over months. A balanced diet rich in antioxidants supports the body's natural anti‑inflammatory pathways, and regular aerobic exercise improves overall respiratory efficiency.
What’s often overlooked is how follow‑up appointments allow doctors to fine‑tune treatment plans. Medications may need adjusting based on how you respond, side‑effects, or emerging research. Continuous monitoring also keeps you accountable, reinforcing those healthy lifestyle choices you made at the outset.
Lastly, the psychological benefit of knowing you’re on top of your health shouldn’t be understated. Confidence in your care plan reduces anxiety, which itself can exacerbate breathing difficulties. So, whether you’re a 20‑year‑old occasional smoker or a 60‑year‑old with a history of COPD, make those regular check‑ups a non‑negotiable part of your routine. Your lungs will thank you, and you’ll likely avoid the costly, invasive treatments that come with late‑stage disease.
Courage Nguluvhe July 16, 2023
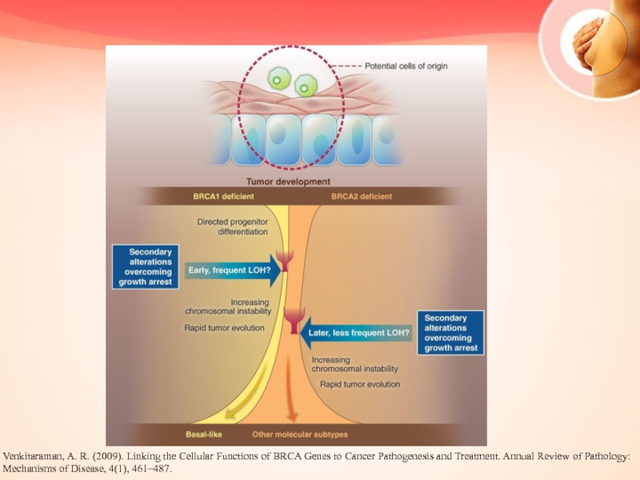
From a clinical standpoint, the integration of high‑resolution computed tomography (HRCT) into routine screening protocols dramatically elevates diagnostic fidelity. HRCT can delineate interstitial patterns, ground‑glass opacities, and bronchial wall thickening with sub‑millimeter precision, which are hallmarks of early inflammatory processes. Coupled with bronchoalveolar lavage cytology, clinicians obtain both anatomic and cellular insights, fostering targeted therapeutic regimens.
Moreover, incorporating biomarkers such as serum IL‑6 and CRP into the assessment algorithm provides a quantitative gauge of systemic inflammation. Elevated levels, even in asymptomatic patients, can preemptively flag subclinical pulmonary involvement. This multimodal approach, while resource‑intensive, curtails progression to irreversible fibrotic remodeling.
Oliver Bishop July 17, 2023
Our country’s health system makes these check‑ups easy, so just get them done.
Alissa DeRouchie July 17, 2023
Honestly, everyone acts like regular checkups are optional, but they’re not- they’re the only way to catch the invisible damage before it ruins everything. It’s weird how we ignore something that’s literally breathing for us every second, yet we skip doctors because it feels like a chore. It’s drama, but also reality.
Emma Howard July 17, 2023
Exactly! Let’s turn that ‘chore’ into a habit- set a reminder, celebrate after each visit, and watch your lungs thrive! 🎉