When you're sneezing, itchy, and swollen from allergies, antihistamines feel like a lifeline. But if you also have high blood pressure, a simple question pops up: Are antihistamines safe for me? The answer isn’t yes or no-it’s more like, which one, how much, and are you taking anything else with it?
Not all antihistamines are the same. Some can drop your blood pressure. Others might nudge it up. And a few, especially when mixed with decongestants, can turn a routine allergy pill into a hidden risk. The good news? Most people with high blood pressure can take antihistamines safely-if they pick the right kind and know what to watch for.
First-Generation vs. Second-Generation: The Big Difference
There are two main types of antihistamines, and the difference matters more than you think.
First-generation antihistamines-like diphenhydramine (Benadryl), chlorpheniramine, and hydroxyzine-were developed decades ago. They work fast and knock you out. That’s why they’re in many sleep aids. But they also cross into your brain easily, which is why they cause drowsiness, dry mouth, and blurred vision. More importantly for blood pressure, they block H1 receptors in your blood vessels. That can cause your vessels to relax too much, leading to a drop in blood pressure. In fact, IV diphenhydramine can lower systolic pressure by 8-12 mmHg within minutes. Even oral doses can cause dizziness when standing up, especially in older adults or those already on blood pressure meds.
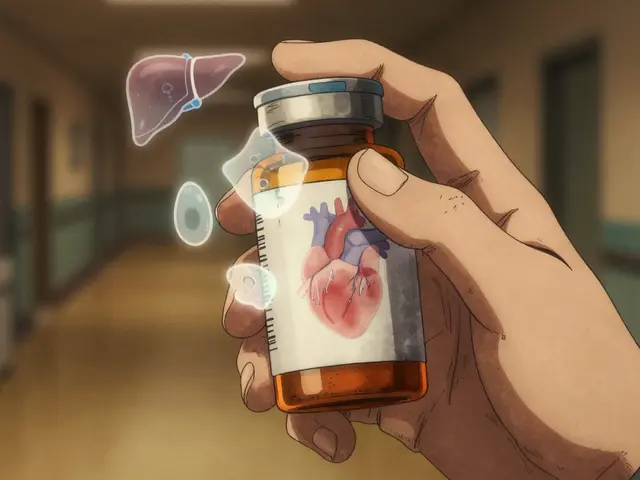
Second-generation antihistamines-like loratadine (Claritin), cetirizine (Zyrtec), and fexofenadine (Allegra)-were designed to avoid the brain. They don’t make you sleepy. And crucially, they don’t mess with your blood pressure the same way. Multiple studies, including FDA reviews up to 2022, show that loratadine has neutral effects in 97% of cases. Cetirizine is equally safe. Fexofenadine, which barely gets processed by the liver, is even cleaner. In clinical trials involving over 4,000 hypertensive patients, 89% reported no change in blood pressure with second-gen antihistamines alone.
Decongestants Are the Real Problem
Here’s where things get tricky. Many allergy pills aren’t just antihistamines-they’re combo packs. Look at the label: Claritin-D, Zyrtec-D, Benadryl Allergy Plus Congestion. That “D” stands for pseudoephedrine or phenylephrine-decongestants.
Decongestants shrink swollen nasal passages by tightening blood vessels. That’s great for a stuffy nose. But they tighten vessels everywhere-including those in your heart and kidneys. That raises blood pressure. GoodRx’s 2023 analysis of 12 clinical trials found that pseudoephedrine can raise systolic pressure by about 1 mmHg on average. Sounds small? In someone with uncontrolled hypertension, that’s enough to push them over the edge. In one survey, 47% of people using decongestant combos reported blood pressure spikes of 5-10 mmHg.
Other combo ingredients add risk too. Ibuprofen in allergy-pain formulas can raise BP by 3-4 mmHg. Acetaminophen, especially at high daily doses (over 4,000 mg), can nudge it up by up to 5 mmHg. So if you’re taking a cold-and-allergy tablet with all three-antihistamine, decongestant, and painkiller-you’re stacking risks.
Who’s at Highest Risk?
Not everyone needs to stress. But some people should be extra careful:
- People with uncontrolled high blood pressure (systolic over 140 mmHg)
- Those on multiple blood pressure medications-antihistamines can interact, especially with beta-blockers or diuretics
- Older adults-they’re more sensitive to drops in blood pressure and dizziness
- People with heart rhythm problems-especially long QT syndrome
- Anyone taking CYP3A4 inhibitors like ketoconazole, erythromycin, or even grapefruit juice-these can spike levels of older antihistamines like fexofenadine or, in rare cases, cetirizine
And while terfenadine and astemizole were pulled from the market in the late 1990s for causing dangerous heart rhythms, they’re still referenced because they show what happens when antihistamines go wrong. Those drugs blocked potassium channels in the heart. Today’s second-gen antihistamines don’t do that-at least not at normal doses.

What Does Monitoring Look Like?
The American Heart Association doesn’t tell everyone to check their blood pressure every time they take an allergy pill. But they do recommend smart steps:
- Before starting: Get your baseline reading. Write it down.
- If you’re on a first-gen antihistamine (like Benadryl): Check your BP 30-60 minutes after the first dose. Watch for dizziness, lightheadedness, or fainting.
- If you’re on a second-gen antihistamine: No routine check needed-unless you feel off. If you have severe heart disease, check after 2-4 hours.
- If you’re using a combo product: Monitor for 2-3 days. Keep a log. If your systolic pressure jumps by 10 mmHg or more, stop and call your doctor.
Home monitors are better than clinic readings. Blood pressure fluctuates. A single reading at the doctor’s office might miss a pattern. Track it at home, same time each day, for three days before and after starting the medication.
Real-World Experiences
People with hypertension share their stories online-and the data matches the science.
On Reddit’s r/Allergy thread from May 2023, 68% of users with high blood pressure said loratadine had no effect. But 22% who used diphenhydramine reported dizziness, often linked to low BP. One user, u/HypertensionWarrior, wrote: “Got IV Benadryl during allergy testing. My systolic dropped 10-12 mmHg in 30 minutes. They made me sit for half an hour before leaving.”
Drugs.com reviews from 2023 show 14% of diphenhydramine users noted “dizziness upon standing.” That’s orthostatic hypotension-a classic sign of blood pressure dropping too fast.
On the flip side, 92% of hypertensive patients in a 2022 American Academy of Allergy survey said they were satisfied with cetirizine. No BP changes. No drowsiness. Just relief.
What Should You Do?
Here’s your simple action plan:
- Read the label. If it says “D,” “Congestion,” or “Sinus,” avoid it unless your doctor says it’s okay.
- Choose second-generation. Loratadine, cetirizine, or fexofenadine are your safest bets.
- Don’t mix. No NSAIDs, no decongestants, no alcohol. Keep it simple.
- Track your BP. Especially in the first few days. Use a validated home monitor.
- Talk to your doctor if you’re on heart meds, have kidney disease, or are over 65.
There’s no need to suffer through allergies just because you have high blood pressure. You just need to pick the right tool-and avoid the traps.
What About Long-Term Use?
Some people take antihistamines daily during pollen season. Others use them year-round for chronic hives or nasal allergies. Is that safe?
Yes-for second-generation antihistamines. The Institute for Clinical and Economic Review found less than 0.01% of users had significant blood pressure changes with long-term use of loratadine or cetirizine. That’s lower than the risk from daily aspirin.
Even better, new research suggests cetirizine might do more than just block histamine. A 2023 study presented at the American Heart Association’s Scientific Sessions showed it reduced endothelial inflammation by 22% in hypertensive patients. That’s a potential bonus-not just safety, but maybe a little heart protection.
Future drugs are even more targeted. Johns Hopkins is testing selective H3 receptor agonists in early trials. These could calm allergic reactions without touching blood pressure at all.
Final Takeaway
Antihistamines don’t have to be off-limits if you have high blood pressure. The problem isn’t the antihistamine-it’s the combo, the old-school version, or the lack of monitoring.
Stick with loratadine, cetirizine, or fexofenadine. Skip the “D.” Watch for dizziness. Check your BP if you’re unsure. And talk to your pharmacist before grabbing anything off the shelf.
Allergies are annoying. But they don’t have to be dangerous.
Can antihistamines raise your blood pressure?
Most antihistamines alone don’t raise blood pressure. Second-generation ones like loratadine, cetirizine, and fexofenadine are neutral. But combination products with decongestants like pseudoephedrine can raise systolic pressure by 5-10 mmHg. Always check the label for “-D” or “congestion” on the name.
Is Benadryl safe if I have high blood pressure?
Benadryl (diphenhydramine) is a first-generation antihistamine and can lower blood pressure, especially when taken in higher doses or given intravenously. It may cause dizziness or lightheadedness when standing. For people with high blood pressure, it’s not the first choice. Safer alternatives like loratadine or cetirizine are preferred.
Which antihistamine is best for high blood pressure?
Loratadine (Claritin), cetirizine (Zyrtec), and fexofenadine (Allegra) are the safest options for people with high blood pressure. They don’t cross the blood-brain barrier, don’t cause drowsiness, and have minimal effect on blood pressure. Avoid products with decongestants like pseudoephedrine.
Can I take antihistamines with my blood pressure meds?
Second-generation antihistamines like loratadine and cetirizine generally don’t interfere with blood pressure medications. But always check with your doctor or pharmacist, especially if you’re taking drugs like ketoconazole, erythromycin, or grapefruit juice, which can affect how your body processes some antihistamines. First-gen antihistamines like Benadryl may interact more and cause dizziness when combined with diuretics or beta-blockers.
Do I need to check my blood pressure every time I take an antihistamine?
No-not if you’re using a second-generation antihistamine and have stable blood pressure. But if you’re starting a new one, especially a first-gen like Benadryl, or using a combo product with a decongestant, check your blood pressure 30-60 minutes after the first dose. If you feel dizzy or your readings change by more than 10 mmHg, stop and call your doctor.







Akash Chopda November 25, 2025
Big Pharma hides the truth about antihistamines and BP they want you to stay sick so you keep buying pills the D in Claritin-D is a trap
Nikki C November 27, 2025
I used to take Benadryl for everything until I passed out in the grocery store
Now I stick to Zyrtec and I swear it changed my life
No dizziness no brain fog just quiet sinuses and I can actually drive
Alex Dubrovin November 28, 2025
This is the kind of info you wish you had before you ruined your BP trying to get through pollen season
Thanks for laying it out like this
Natashia Luu November 28, 2025
It is unconscionable that over-the-counter medications contain ingredients capable of inducing hypertensive crises without mandatory warning labels
Regulatory agencies are complicit in public endangerment
Andy Louis-Charles November 29, 2025
Loratadine is the GOAT 🏆
Been on it for 5 years with hypertension
Zero issues
Also avoids the 3pm nap that Benadryl gives you
Adam Hainsfurther November 30, 2025
I appreciate how you broke down the difference between first and second gen
I didn’t realize how much the brain penetration mattered
Now I know why I felt like a zombie after Benadryl
Rachael Gallagher December 2, 2025
Americans are so lazy they’ll take a pill with 3 drugs in it just to avoid reading the label
Of course your BP spikes
steven patiño palacio December 3, 2025
It is critical to distinguish between antihistamine monotherapy and combination products
Second-generation antihistamines demonstrate negligible cardiovascular effects in clinical populations with hypertension
Decongestants remain the primary concern
Neoma Geoghegan December 5, 2025
Cetirizine > everything
My BP stayed stable during allergy season
Also no drowsiness = I can still function
akhilesh jha December 7, 2025
I tried fexofenadine last year
It worked
But I felt like something was missing
Like my body wasn’t fighting back
Maybe I’m just addicted to the crash
Jeff Hicken December 7, 2025
this post is too long i read like 3 lines then got bored
just say what pill to take
Douglas cardoza December 8, 2025
I used to take Claritin-D every spring
Then my BP jumped to 160/95
Switched to plain Claritin and now I’m back to 120/75
Simple fix
stephanie Hill December 10, 2025
They don’t want you to know that the FDA approved these combo pills because Big Pharma pays them
Benadryl is basically poison with a smiley face on the bottle
Sam Jepsen December 11, 2025
If you have high BP and allergies you owe it to yourself to talk to a pharmacist
They’re not just people who hand out pills
They’re your secret weapon
Yvonne Franklin December 12, 2025
Cetirizine saved me
My doc said no Benadryl
I listened
Best decision ever