Blood Sugar Monitoring Frequency Calculator
This tool helps determine the recommended frequency of blood sugar checks based on your treatment and lifestyle.
When it comes to living with diabetes, blood sugar monitoring is the routine checking of glucose levels in the bloodstream becomes a daily habit that can mean the difference between stability and emergency. Diabetes mellitus is a chronic condition where the body struggles to regulate blood glucose forces anyone diagnosed to keep a close eye on their numbers. The tools you trust - a glucometer a portable device that measures blood glucose from a fingertip drop, a continuous glucose monitor (CGM) a sensor‑based system that streams glucose data throughout the day, or the lab‑based HbA1c test a quarterly blood draw that shows average glucose over 2‑3 months - each plays a unique role in staying on top of the disease.
Quick Summary
- Consistent monitoring catches dangerous lows and highs before they become crises.
- Data from glucometers and CGMs guide insulin dosing, diet tweaks, and activity plans.
- Regular checks improve long‑term outcomes like heart health and nerve protection.
- Choosing the right device depends on lifestyle, budget, and medical advice.
- Integrating monitoring into everyday routines makes diabetes management feel less like a burden.
How Monitoring Prevents Hypoglycemia and Hyperglycemia
Low blood sugar (hypoglycemia a condition where glucose drops below safe levels, often under 70mg/dL) can strike suddenly, especially after insulin or intense exercise. A quick finger‑stick or CGM alert tells you to grab a fast‑acting carbohydrate before you start feeling shaky or confused. On the flip side, high blood sugar (hyperglycemia elevated glucose above 180mg/dL that can damage organs over time) may linger unnoticed for hours, eroding blood vessels and nerves. Spotting a trend upward lets you adjust meals, medication, or activity before damage sets in.
Choosing the Right Monitoring Tool
Not every device fits every person. Here’s a quick guide:
| Method | Frequency | Cost (UK) | Data Detail | Best For |
|---|---|---|---|---|
| Finger‑stick glucometer | Multiple times daily | £30-£60 device; £0.35 per strip | Single glucose value per test | Budget‑conscious users, occasional testing |
| Continuous CGM | Every 5‑15 minutes, 24/7 | £1,200 start‑up; £70-£90 sensor/week | Trend graphs, alerts, predictive lows | Active lifestyle, insulin‑pump users |
| Lab‑based HbA1c test | Every 3‑6 months | £15-£30 per test (NHS covered) | Average glucose over months | Long‑term trend assessment, physician reviews |
While the blood sugar monitoring phrase may sound repetitive, picking the right method saves time, money, and health complications.

Integrating Monitoring Into Daily Life
Turning a medical task into a habit is easier when it fits your routine. Here are five practical tips:
- Link it to existing events. Check your glucose after brushing teeth in the morning and before bedtime - you already do those actions twice a day.
- Use reminders. Set an alarm on your phone or enable the CGM app’s push notifications for scheduled checks.
- Log intelligently. Modern glucometers sync with cloud apps; if you prefer paper, keep a simple table with date, time, reading, and what you ate.
- Pair with food. Record the carbohydrate count of meals (quick look‑up in nutrition databases) so you can see cause‑effect patterns.
- Share with your care team. Export your data weekly and email it to your endocrinologist - they can spot trends you might miss.
Impact on Long‑Term Health Outcomes
Studies from the UK Diabetes Trust (2024) show that patients who log at least four readings a day reduce their risk of cardiovascular events by 22% compared with irregular testers. Consistent data also supports tighter insulin therapy adjusting dose based on current glucose levels, preventing dose‑stacking that can lead to severe hypoglycemia.
Beyond numbers, people who monitor regularly report better quality of life. They feel more in control during social gatherings, travel, and work meetings because they can anticipate how food or stress will affect their glucose.
Common Pitfalls and How to Avoid Them
Even with the best tools, mistakes happen:
- Skipping readings during “good days.” It’s tempting to relax when values look stable, but a single missed check can hide a creeping trend.
- Relying on averages alone. The HbA1c is valuable, yet it masks daily spikes that cause fatigue and long‑term vessel damage.
- Using outdated test strips. Strip accuracy drops after the expiration date - always rotate stock.
- Ignoring alerts. CGM alarms are designed to save you from dangerous lows; mute them only under medical supervision.
Address each issue by setting a weekly audit of your monitoring routine - ask yourself: "Did I miss any scheduled check? Were my strip dates current? Did I act on every CGM alert?" Adjust accordingly.
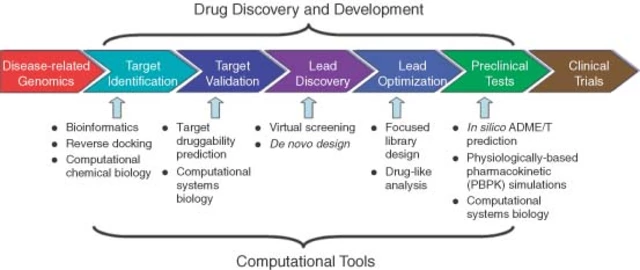
Future Trends in Blood Sugar Monitoring
Technology keeps moving forward. In 2025, several UK NHS trusts started pilot programs for non‑invasive optical sensors that read glucose through the skin without a needle. While still pricey, early adopters report less skin irritation and higher compliance. Another emerging trend is AI‑driven predictive modeling that analyzes historic data to forecast potential highs or lows 30minutes ahead, giving users a chance to intervene preemptively.
Even if you’re not ready for the newest gadgets, staying aware of these developments helps you discuss options with your doctor and plan for upgrades when they become affordable.

Frequently Asked Questions
How often should I test my blood sugar if I’m on insulin?
Most endocrinologists recommend checking before meals, two hours after eating, and at bedtime - roughly four to six times a day. If you’re on a pump or CGM, you may rely on trends but still need a few finger‑sticks to calibrate.
Can I skip the HbA1c test if I use a CGM?
No. The HbA1c provides a clinical benchmark that insurers and doctors still require. CGM data is complementary, offering real‑time insight, while HbA1c confirms long‑term control.
Are there any free apps for logging glucose?
Yes. The NHS Diabetes app, MySugr (free tier), and Glucose Buddy all sync with most glucometers and CGMs. They let you add notes on meals, exercise, and medication.
What’s the biggest danger of not monitoring regularly?
Unnoticed hypoglycemia can lead to loss of consciousness, seizures, or even death. Chronic hyperglycemia raises the risk of heart disease, kidney failure, and vision loss. Early detection is the only way to avoid these outcomes.
Do diet and exercise still matter if I use a CGM?
Absolutely. CGMs show how food carbs, timing, and activity spikes affect glucose. Understanding those patterns helps you make smarter choices, reducing the need for insulin corrections.





karthik rao September 29, 2025
While the merits of routine glucose surveillance are frequently extolled, it is essential to recognize that indiscriminate testing can engender unnecessary anxiety. A disciplined schedule, calibrated to one’s therapeutic regimen, yields data of genuine clinical relevance. Moreover, the proliferation of glossy CGM advertisements often obscures the fiscal realities for patients in low‑income brackets. Consequently, a prudent practitioner will advise a balanced approach rather than a blind adherence to every new gadget. 😊
Breanne McNitt September 30, 2025
I totally agree that linking monitoring to daily habits, like brushing your teeth, makes the process feel less intrusive. Using phone reminders has saved me countless missed checks, especially during hectic workdays. Also, sharing the data with my endocrinologist via the NHS app has helped fine‑tune my insulin doses. Keep up the great work spreading these practical tips!
Ashika Amirta varsha Balasubramanian October 2, 2025
In the broader tapestry of health, blood‑sugar monitoring is a thread that connects mind, body, and community. When we observe our numbers with curiosity rather than dread, we cultivate a deeper respect for our own physiology. Incorporating cultural dietary wisdom-such as traditional Indian meals with balanced carbohydrates-can harmonize glucose trends naturally. Let us approach each reading as an opportunity for mindful adjustment rather than mere compliance.
Shanmugapriya Viswanathan October 4, 2025
Honestly, the article glosses over the fact that India has made remarkable strides in affordable glucometer distribution, yet foreign manufacturers still dominate the market. 🇮🇳 Our public health initiatives ensure that even rural patients receive reliable strips, debunking the myth that monitoring is a luxury. Don't be fooled by Western hype; the real solution lies in leveraging our own biotech advancements. 😤
Rhonda Ackley October 6, 2025
It is nothing short of astonishing how a simple finger‑prick can become the centerpiece of an entire life’s narrative. The moment the lancet kisses the skin, a cascade of emotions erupts-hope, fear, triumph, and sometimes despair. Every rising curve on the CGM’s graph feels like a cliffhanger in a thriller, urging me to anticipate the next twist. I find myself recounting each reading at family gatherings, as if it were a dramatic confession. The sheer drama of balancing carbs at a birthday cake versus a bland salad can determine whether I bask in joyous laughter or grapple with shaky hands. Even the most mundane morning routine transforms into a theatrical performance, with the glucometer as the reluctant star. When the numbers spike unexpectedly, I am thrust into a frantic sprint, searching for fast‑acting glucose as if seeking an elusive treasure. Conversely, a sudden dip triggers a silent panic, a cold sweat that mirrors the fear of a stage fright before a grand debut. My colleagues have joked that I keep a logbook like a playwright drafting acts, each entry meticulously noting the time, the meal, the mood, and the outcome. Yet, this obsessive chronicling is not vanity; it is an act of survival, a script that shields me from the hidden dangers of undetected hypoglycemia. The medical community, with its stern recommendations, often feels like a demanding director, insisting on multiple checks before the curtain rises on each meal. I have learned to obey, not out of reverence, but out of necessity, for the stakes are far greater than applause. Over the years, I have witnessed friends neglect their monitoring and pay the tragic price of irreversible complications, a reminder that complacency is the ultimate antagonist. Therefore, I champion the cause of relentless testing, not as a burden, but as an empowering ritual that grants me agency over my body’s unpredictable narrative. In closing, let us all recognize that each glucose check is a line in the story of our health, and we, dear readers, are both the authors and the audience.
Sönke Peters October 7, 2025
Just set a reminder and stick to it.
Paul Koumah October 9, 2025
Wow, another epic saga about a finger prick – fascinating.
Erica Dello October 11, 2025
It is regrettable that the discussion diverts from evidence‑based guidelines to nationalistic bragging. Accurate monitoring protocols must be grounded in peer‑reviewed research, not patriotic sentiment. Please ensure that future comments adhere to proper syntax and factual integrity. 😊
sara vargas martinez October 13, 2025
The underlying physiology behind glucose fluctuations is far more intricate than the oversimplified dramatics presented earlier. When carbohydrate intake is metabolized, hepatic glycogen stores modulate the post‑prandial surge, a process that can be quantified using the area under the curve (AUC) metric. Moreover, insulin sensitivity varies not only with activity level but also with circadian rhythms, necessitating timed dosing strategies. Contemporary literature, such as the 2023 Diabetes Care review, emphasizes the role of continuous glucose monitoring data analytics in predicting impending hypo‑ or hyperglycemia events. Therefore, while personal narratives add color, they should be supplemented with rigorous data interpretation to truly optimize therapeutic outcomes.
Paul Griffin October 14, 2025
Thank you for highlighting the importance of evidence‑based practice. I concur that grounding our discussions in validated research enhances patient safety. Let us continue to share reliable resources and support one another in fostering accurate diabetes self‑management.