When you pick up a prescription for a generic drug, you’re not getting a lesser version of the medicine. You’re getting the same thing-just at a fraction of the cost. But how does the FDA make sure that a generic pill, patch, or injection works just as well as the brand-name version? The answer isn’t simple, and it’s not just about matching ingredients. It’s about proving, with hard data, that every dose you take is safe, consistent, and effective.
What Makes a Generic Drug ‘The Same’?
The FDA doesn’t just say a generic drug is equivalent. They prove it. Under the Hatch-Waxman Act of 1984, two strict criteria must be met: pharmaceutical equivalence and bioequivalence.
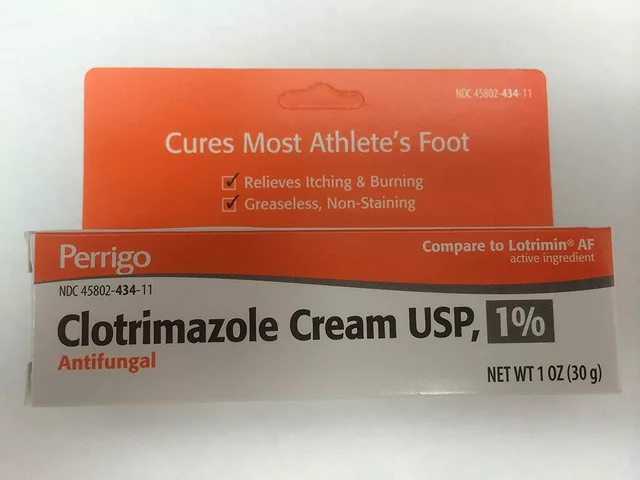
Pharmaceutical equivalence means the generic drug has the same active ingredient, strength, dosage form (pill, liquid, injection), route of administration (oral, topical, etc.), and intended use as the brand-name drug. The label must match too. That’s the baseline. But here’s what most people don’t realize: the inactive ingredients can be different. Color, flavor, fillers, and even the shape of the pill don’t matter-as long as they don’t affect how the drug works. A generic aspirin might be blue instead of white, or oval instead of round. That’s fine.
Bioequivalence is where the real testing happens. It’s not enough for two drugs to have the same ingredients. They must deliver those ingredients into your bloodstream the same way. The FDA requires that the 90% confidence interval for two key measurements-Cmax (peak concentration in the blood) and AUC (total exposure over time)-must fall between 80% and 125% of the brand-name drug’s values. That’s not a guess. It’s a statistically proven range based on studies done in healthy volunteers.
Most generic drugs are tested using single-dose studies in 24 to 36 people. Blood samples are taken over several hours to map how quickly and how much of the drug gets absorbed. If the numbers fall within that 80%-125% window, the FDA approves it. This system has been used for decades and works for over 90% of all generic drugs on the market.
How Are Generic Drugs Made and Tested?
Manufacturing a generic drug isn’t like baking cookies. It’s a precision science. Every step-from sourcing raw materials to packaging the final product-must follow Current Good Manufacturing Practices (cGMP), written into federal law under 21 CFR Parts 210 and 211. These rules apply equally to brand-name and generic manufacturers. There’s no second-tier standard.
Every batch of a generic drug must be tested for identity (is this the right drug?), strength (does it have the right amount of active ingredient?), purity (is it free of toxins or contaminants?), and quality (does it dissolve properly?). These tests aren’t done once. They’re done for every single lot produced. The methods used must be validated, meaning they’ve been proven to give accurate, repeatable results.
Stability testing is another big part of the process. A generic drug must prove it won’t break down or lose effectiveness over time. Manufacturers run accelerated tests-like storing the drug at 40°C and 75% humidity for six months-to predict how it will hold up over its shelf life. Then they do long-term studies at real-world storage conditions for 12 to 24 months. If the drug still meets specs after two years, that’s its labeled expiration date.
The FDA doesn’t trust paperwork alone. They send inspectors to over 3,500 manufacturing sites every year-across the U.S. and around the world. These inspections check everything: equipment cleanliness, worker training, data integrity, even how raw materials are stored. A single violation can delay approval for months. And here’s a fact many don’t know: about half of all generic drugs in the U.S. are made by the same companies that produce the brand-name versions. Often, they’re made in the same factory, on the same lines.
The ANDA Process: How a Generic Gets Approved
Getting a generic drug approved isn’t quick, but it’s streamlined. Companies submit an Abbreviated New Drug Application (ANDA). Unlike brand-name drugs, which need full clinical trials, generics rely on the FDA’s existing data on the brand-name drug. That’s why it’s called ‘abbreviated.’
An ANDA must include:
- Proof of pharmaceutical equivalence
- Bioequivalence study results
- Manufacturing details and facility information
- Stability data
- Labeling that matches the brand-name drug
The FDA’s Office of Generic Drugs reviews each application. As of 2023, the standard review goal is 10 months for a complete application. But if the data is incomplete or unclear, the FDA issues a ‘complete response letter,’ and the clock resets. In fiscal year 2022, the FDA approved 892 original ANDAs and issued 478 complete response letters. That means nearly half of applications needed more work before approval.
Since 2012, the Generic Drug User Fee Amendments (GDUFA) have helped speed things up. Companies pay fees to fund FDA reviews, and in return, the agency commits to clear timelines. GDUFA III, renewed in 2022, added more focus on complex generics and created the Pre-ANDA program, where manufacturers can meet with FDA scientists early to avoid costly mistakes. In 2022 alone, there were 1,243 Pre-ANDA meetings.
Complex Generics: When the Rules Get Harder
Not all drugs are as simple as a pill you swallow. Think inhalers, injectables, creams, gels, or patches. These are called complex generic drugs. For them, showing bioequivalence isn’t enough. You can’t just measure blood levels-you need to prove the drug behaves the same way in the body at a physical level.
For example, an inhaler must deliver the same particle size, spray pattern, and lung deposition as the brand-name version. A topical cream must penetrate the skin at the same rate. These aren’t just chemical tests-they’re engineering challenges.
The FDA has created over 2,143 product-specific guidances for these complex products. Each one outlines exactly what data is needed. In 2023 alone, they released 27 new guidances. Some of these require advanced testing like in vitro dissolution, structural analysis, or even clinical endpoint studies-where patients are tracked for actual health outcomes, not just blood levels.
Dr. Charles Ganley, former head of the FDA’s Office of Generic Drugs, pointed out in 2019 that these products are harder to prove equivalent. And the FDA agrees. They’ve allocated $15.7 million from 2023-2027 specifically to research better testing methods for complex generics. They’ve held 18 public workshops with over 1,200 experts to tackle these problems.
Do Generics Really Work the Same?
The data says yes. In 2022, a Consumer Reports survey of 1,200 U.S. adults found 89% were satisfied with generic drugs, and 62% chose them specifically to save money. The American Medical Association, the American Academy of Family Physicians, and the FDA all agree: FDA-approved generics are safe and effective.
But there are exceptions. Some drugs have a narrow therapeutic index-meaning the difference between a helpful dose and a harmful one is very small. Levothyroxine, used for thyroid conditions, is one of them. A 2021 study in JAMA Internal Medicine found that 12.3% of patients switched between different generic versions experienced thyroid hormone fluctuations that required dose adjustments.
Similarly, some patients report issues with blood thinners like warfarin or seizure medications like phenytoin. On Reddit’s r/pharmacy, 17% of 1,427 respondents said they noticed differences when switching generics, mostly with these types of drugs. These aren’t common, but they’re real. That’s why pharmacists often recommend sticking with the same generic manufacturer if you’re on one of these drugs.
The FDA acknowledges this. They monitor adverse events and require manufacturers to report any unexpected issues. And while most people won’t notice a difference, if you’re on a narrow-therapeutic-index drug, talk to your doctor. Consistency matters.
Why This Matters: Cost, Access, and Trust
Generic drugs saved the U.S. healthcare system $37 billion in 2022. They make up over 90% of prescriptions filled but only about 23% of total drug spending. That’s the power of competition. Without generics, many people couldn’t afford their meds.
The FDA’s system isn’t perfect, but it’s built on science, not guesswork. Every approved generic drug has been tested, inspected, and verified. The agency doesn’t approve generics because they’re cheap. They approve them because they’ve proven they’re the same.
When you take a generic drug, you’re not taking a risk. You’re taking a scientifically validated medicine that’s been held to the same standard as the brand-name version. The only difference? The price tag.
Are generic drugs as safe as brand-name drugs?
Yes. Generic drugs must meet the same FDA standards for safety, strength, quality, and purity as brand-name drugs. The active ingredient is identical, and manufacturing facilities are inspected to the same level. The FDA has stated that approved generics have the same high quality as their brand-name counterparts.
Why do generic drugs look different from brand-name drugs?
U.S. law requires that generic drugs look different from brand-name drugs to avoid trademark infringement. That means color, shape, size, and flavor can vary. But these changes don’t affect how the drug works. Only the active ingredient matters for effectiveness.
Can I switch between different generic versions of the same drug?
For most drugs, yes. The FDA ensures all approved generics are bioequivalent. But for drugs with a narrow therapeutic index-like levothyroxine, warfarin, or phenytoin-switching between different generic manufacturers can sometimes cause small changes in blood levels. If you’re on one of these drugs, talk to your doctor or pharmacist before switching.
How does the FDA test bioequivalence?
The FDA uses pharmacokinetic studies in healthy volunteers. Blood samples are taken over time after taking the drug to measure how much enters the bloodstream (AUC) and how fast it peaks (Cmax). The generic’s values must fall within 80% to 125% of the brand-name drug’s values. This range is based on decades of scientific evidence and statistical analysis.
Are all generic drugs made in the U.S.?
No. The FDA inspects manufacturing facilities worldwide. Over half of generic drugs sold in the U.S. are made overseas, primarily in India and China. But every facility-whether in the U.S., India, or elsewhere-must meet the same cGMP standards. The FDA conducts thousands of inspections each year to ensure compliance.




Chiruvella Pardha Krishna February 15, 2026
The FDA’s bioequivalence threshold of 80%-125% isn’t just a number-it’s a philosophical compromise between perfection and practicality. We demand absolute consistency in medicine, yet accept a 25% variance in absorption. Is that trust? Or just the quiet surrender of a system that knows better than to ask for miracles?
Every pill you swallow is a statistical artifact, not a sacrament. And yet, millions take it without question. There’s poetry in that. Or maybe just exhaustion.
Joe Grushkin February 16, 2026
Let’s be real-the FDA doesn’t ‘prove’ anything. They approve based on industry-submitted data. The whole system’s a handshake deal with pharma. And don’t get me started on the 50% of generics made by the same companies as brand names. It’s not competition. It’s branding with a cheaper label.
Virginia Kimball February 18, 2026
I love how this post breaks it all down without the fluff. Seriously, people panic about generics looking different or costing less-but they’re doing the exact same job. My dad’s been on generic metoprolol for 12 years and still runs marathons. If it works, it works. No need to overthink it.
Also-shoutout to the FDA inspectors trudging through factories in India and China. Those folks are the real MVPs.
Betty Kirby February 19, 2026
Chiruvella Pardha Krishna just called a regulatory framework ‘poetry.’ That’s not deep. That’s pretentious. Bioequivalence isn’t philosophy-it’s math. And the 80-125% range? It’s not a compromise. It’s a scientifically validated tolerance based on decades of pharmacokinetic data. Stop romanticizing bureaucracy.
Josiah Demara February 20, 2026
Virginia Kimball is adorable. You think your dad’s on metoprolol and that’s proof? What about the 12.3% of levothyroxine patients who had hormone swings after switching generics? JAMA Internal Medicine didn’t make that up. And no, ‘it works’ isn’t a scientific argument-it’s anecdotal noise wrapped in optimism.
The FDA’s system works for 90% of drugs. The other 10%? The ones that kill people when you switch them? You’re lucky you haven’t been one of them.
Kaye Alcaraz February 22, 2026
Thank you for the detailed breakdown. The rigor behind cGMP, stability testing, and global inspections is not something to take lightly. This is public health infrastructure at its most meticulous. When we dismiss generics as ‘cheap alternatives,’ we undermine the entire scientific and regulatory architecture that keeps us safe.
Every lot tested. Every facility inspected. Every bioequivalence curve validated. This is not luck. This is discipline.
Charlotte Dacre February 24, 2026
So let me get this straight: we trust a pill made in a factory in Hyderabad with the same active ingredient as the brand name… but we’re terrified it’ll be ‘different’ because it’s blue instead of white? Classic. The real drug here is placebo.
Esha Pathak February 26, 2026
There’s something beautiful about how a tiny pill, made on the other side of the world, carries the weight of a life. We don’t see the inspectors. We don’t read the stability reports. We just swallow it. And somehow, it works. Maybe science isn’t cold after all. Maybe it’s quiet. And faithful.
❤️