Travel Pathogen Risk Checker
Check Your Travel Risk
Select your destination to see common enteric infections and recommended precautions.
Travel Risk Assessment
Select a destination to see common enteric infections and prevention measures.
Common Pathogens
Prevention Tips
Picture this: you’re sipping a fresh coconut on a beach in Thailand, when a sudden stomach cramp ruins the vibe. That’s the nightmare of catching an enteric infection while traveling. The good news? With the right knowledge, you can keep your gut happy and explore the world worry‑free.
Understanding Enteric Infections
Enteric infections are illnesses that affect the gastrointestinal tract, primarily the stomach and intestines. They’re caused by a range of bacteria, viruses, and parasites that you can pick up through contaminated food, water, or poor hygiene. The most common symptom set includes diarrhea, abdominal cramps, nausea, and sometimes fever.
Why Travelers Are Prime Targets
Travel disrupts your routine. New cuisines, unfamiliar water sources, and differing sanitation standards expose you to microbes your body isn’t used to. Studies from the CDC show that up to 50% of short‑term travelers experience some form of gastrointestinal upset, often dubbed “traveler’s diarrhea.”
Hotspots and the Usual Suspects
Not all destinations carry the same risk. Here’s a quick glance at the regions most linked to specific pathogens:
- Escherichia coli (ETEC) - prevalent in SouthAsia, Latin America, and Africa; typically spreads via contaminated water.
- Campylobacter jejuni - common in Eastern Europe and parts of the Middle East; often linked to undercooked poultry.
- Salmonella enterica - worldwide, especially where eggs and raw produce are consumed raw.
- Shigella spp. - high‑risk in crowded urban areas with limited sanitation.
- Vibrio cholerae - coastal regions of SouthAsia and parts of the Caribbean; can cause severe watery diarrhea.
- Hepatitis A virus - transmitted via contaminated food; especially a concern in Central America and the Middle East.

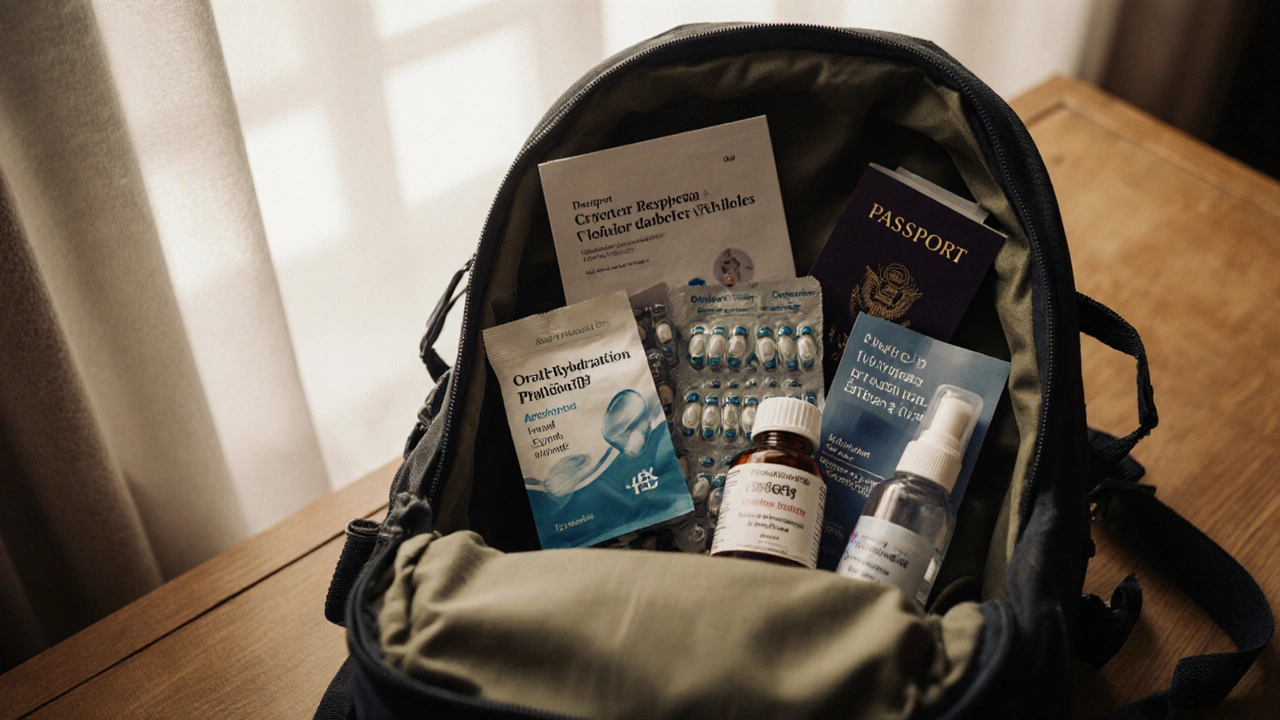
Pre‑Travel Preparation: Vaccines, Clinics, and Probiotics
Before you board the plane, a few steps can drastically lower your risk.
- Visit a Travel Health Clinic at least 4-6 weeks before departure. They’ll tailor vaccine recommendations based on your itinerary.
- Get vaccinated against Hepatitis A (if you haven’t already) and consider typhoid or cholera vaccines for high‑risk zones.
- Ask about a prescription for Azithromycin or fluoroquinolones-these are the go‑to antibiotics for moderate to severe traveler’s diarrhea.
- Pack a supply of Probiotics. A daily dose of Lactobacillus rhamnosus GG has been shown to cut the incidence of travel‑related diarrhea by about 30%.
- Include Oral Rehydration Solution (ORS) packets-these restore electrolytes if you do get sick.
Smart Hygiene on the Ground
Even the best prep can’t replace daily vigilance. Follow these habits:
- Water safety: Drink only bottled water sealed by the manufacturer, or treat tap water with chlorine tablets or a portable UV purifier.
- Food choices: Eat foods that are hot‑cooked and served piping hot. Avoid raw salads, unpeeled fruits, and street‑vendor ice unless you’re sure of the source.
- Hand cleanliness: Use an alcohol‑based hand sanitizer (≥60% ethanol) before meals. If soap and water are available, wash for at least 20 seconds.
- Utensil caution: Prefer disposable cutlery or bring your own set of travel‑size utensils.
If You Get Sick: First‑Aid Steps
Even with precautions, illness can strike. Here’s a quick response plan:
- Assess severity: Mild cramps with 2-3 loose stools usually resolve in 24-48hours. Hydration is the main goal.
- Rehydrate: Mix one ORS packet with 200ml of clean water and sip frequently. Coconut water can be a backup, but it lacks electrolytes.
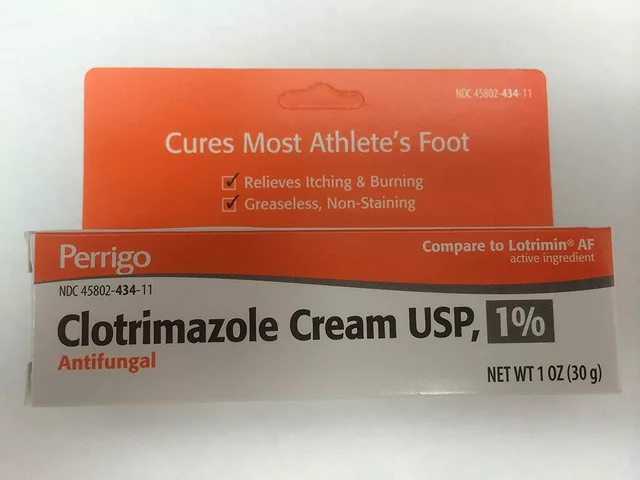
- Consider over‑the‑counter meds: Loperamide can slow motility for mild cases, but avoid it if you have a fever or blood in stools.
- Antibiotic option: If diarrhea persists beyond 48hours, is bloody, or you have a fever >38.5°C, take the prescribed azithromycin (500mg once daily for 3 days) as directed.
- Seek professional care: Visit a local clinic or hospital if you develop severe dehydration, vomiting, or symptoms of cholera (rice‑water stools). Carry a card with your emergency contacts and medical insurance details.
Quick Reference: Pathogen‑Symptom‑Treatment Table
| Pathogen | Typical Symptoms | First‑line Treatment |
|---|---|---|
| ETEC (E.coli) | Watery diarrhea, cramps, low‑grade fever | ORS + optional azithromycin if >48h |
| Campylobacter jejuni | Bloody diarrhea, severe cramps, fever | Azithromycin 500mg daily ×3days |
| Salmonella enterica | Diarrhea, fever, vomiting | Supportive care; antibiotics if invasive |
| Shigella spp. | Bloody stools, high fever, tenesmus | Ciprofloxacin 500mg BID ×3days |
| Vibrio cholerae | Profuse watery stools, rapid dehydration | IV fluids + doxycycline 300mg single dose |
| Hepatitis A virus | Jaundice, fatigue, nausea (incubation 2-6weeks) | Supportive care; vaccine for prevention |
Putting It All Together: A Travel Health Checklist
- Schedule a pre‑travel appointment with a Travel Health Clinic (4-6weeks ahead).
- Update routine vaccinations; add HepatitisA, Typhoid, and Cholera if needed.
- Pack ORS packets, a short course of azithromycin, and a daily probiotic.
- Carry a reliable water purification method (UV pen or chlorine tablets).
- Buy a travel‑size hand sanitizer (≥60% alcohol).
- Keep a copy of your medical insurance and emergency contacts.
- Review local health advisories from the World Health Organization and CDC.
Frequently Asked Questions
What is the fastest way to treat traveler’s diarrhea?
Start with oral rehydration solution to replace fluids and electrolytes. If the diarrhea lasts more than 48hours, includes blood, or you have a fever, take the prescribed antibiotic (typically azithromycin) and seek medical care.
Are probiotics worth packing?
Yes. Clinical trials show that daily Lactobacillusrhamnosus GG can reduce the risk of travel‑related diarrhea by roughly one‑third, especially when combined with good hygiene.
Do I need a vaccine for HepatitisA?
If you’re traveling to regions with low sanitation standards-most of Asia, Africa, Central America, and parts of the Middle East-vaccination is strongly recommended. It provides protection for at least 20years.
Can I treat diarrhea with over‑the‑counter meds?
Loperamide can help reduce stool frequency in mild cases, but avoid it if you have a fever or blood in the stool, as it may trap the pathogen inside your intestines.
What should I do if I suspect cholera?
Cholera can cause rapid, life‑threatening dehydration. Start aggressive rehydration with ORS or IV fluids immediately and seek urgent medical care for antibiotic therapy (often doxycycline).







Sarah Aderholdt October 12, 2025
Travel safety starts with the basics: pack a reliable water filter and a few ORS sachets. Keep hand sanitizer handy for every meal stop. Staying aware of local hygiene standards keeps your gut happy.
Phoebe Chico October 13, 2025
Nothing beats a bold adventure, but don’t let those exotic street tacos betray you. Slurp bottled water like it’s the finest wine, and dodge any ice that looks suspiciously homemade. Remember, a single sip of contaminated ice can ruin an entire vacation, so guard your glass like a treasure.
Larry Douglas October 13, 2025
When planning a trip you should first identify the endemic pathogens of the region then acquire appropriate vaccinations afterwards the CDC recommends a pre‑travel consultation at least six weeks prior to departure and any traveler’s diarrhea prophylaxis should be considered for high‑risk areas such as South Asia and sub‑Saharan Africa furthermore oral rehydration salts are essential for managing fluid loss during episodes of diarrhea.
Michael Stevens October 14, 2025
Great reminder about the timing; early preparation really does make a difference. Adding a probiotic to the packing list can also help maintain gut flora during travel.
Ann Campanella October 15, 2025
Honestly this guide feels overly wordy.
Desiree Tan October 16, 2025
Pack that antibiotic kit, don’t gamble with your health. A short course of azithromycin can be a lifesaver if you’re caught off guard. Also, make a habit of washing your hands after every bathroom visit – it’s non‑negotiable. Your itinerary will be smoother if you treat prevention like a daily ritual.
Andrea Dunn October 16, 2025
Well, maybe the “authorities” don’t want you to know about the cheap water filters they hide in plain sight 😏. Just saying, stay vigilant.
Erin Johnson October 17, 2025
Oh, look at you, thinking you can outsmart microbes with a tiny bottle of water. The reality is that most travelers underestimate the cunning adaptability of enteric pathogens. First, understand that bacteria like ETEC thrive in even the most pristine-looking streams, turning a refreshing sip into a nightmare. Second, the very act of ignoring hand hygiene is akin to inviting a burglar into your home. Third, those colorful street food stalls often serve dishes that sit at room temperature for hours, providing a breeding ground for Shigella. Fourth, relying solely on “look‑good” bottled water can backfire when the seal is compromised. Fifth, dehydration isn’t just a mild inconvenience; it can precipitate renal failure if ignored. Sixth, the heroics of “just a little Loperamide” are misplaced when blood stains the toilet bowl. Seventh, antibiotics are not a free‑for‑all indulgence; misuse fuels resistance faster than you can say “travel.” Eighth, oral rehydration solutions are science‑backed but often tossed aside for sugary sports drinks that worsen electrolyte imbalance. Ninth, your immune system isn’t a superhero; it needs support through proper nutrition, sleep, and stress management. Tenth, vaccines like Hepatitis A are not optional extras; they are essential armor for dangerous regions. Eleventh, a portable UV purifier may look like a gadget, but it can literally save your life when you’re stranded without clean water. Twelfth, the “just drink coconut water” myth neglects the fact that many coconuts are harvested after the prime freshness window, harboring hidden bacteria. Thirteenth, don’t forget that the “hospital” in some remote locales might lack IV fluids, making early ORS use critical. Fourteenth, always carry a written list of your medical allergies and a copy of your insurance card – bureaucracy can be deadly. Fifteenth, when you finally make it home, a post‑travel stool test can catch lingering infections before they cause chronic issues. Finally, remember that the best travel story is the one where you return home healthy, with memories intact, and not a tale of gut turmoil.
Rica J October 18, 2025
Yo lol mind the typo but seriously, a cheap water filter can be a game‑changer. I once used a cheap one in Thailand and survived. Pack a spare just in case the first one fails.
Linda Stephenson October 18, 2025
I love how the guide breaks down each region, makes planning less overwhelming. The tip about avoiding raw salads really hits home for me because I’m always skeptical of street vendors. Also, carrying hand sanitizer feels like a tiny shield against unseen germs.
Catherine Mihaljevic October 19, 2025
Sure but the guide overstates risk for Europe it’s not that bad.
Justyne Walsh October 20, 2025
Right, Europe’s food safety standards are generally high, but complacency can still lead to surprise bouts of diarrhea. A little caution never hurts, even in the “clean” corners of the continent.
Callum Smyth October 20, 2025
Absolutely, a simple bottle of purified water can make all the difference. 😊 Stay safe and enjoy the flavors of the world!
Jason Ring October 21, 2025
True, and don’t forget to double‑check the seal before you buy. It’s a tiny step that saves huge trouble.
Kyle Salisbury October 22, 2025
Cultural immersion is rewarding, but respecting local hygiene practices is essential.
Angie Robinson October 22, 2025
Honestly, most travelers ignore the basic advice and suffer avoidable illness.
Emmons Kimery October 23, 2025
Exactly, following the basics can prevent the majority of cases. 👍🏽
Mimi Saki October 24, 2025
Sending you good vibes for a healthy adventure! 🌟
Subramaniam Sankaranarayanan October 25, 2025
From a clinical perspective, the prophylactic use of antibiotics should be guided by local resistance patterns. Overprescription can undermine treatment efficacy worldwide. Therefore, consult up‑to‑date regional data before self‑medicating.