Ever wonder why your doctor told you to take that pill with food-especially something fatty? It’s not just to avoid an upset stomach. For many modern medications, eating fat isn’t optional-it’s part of how the drug works. This isn’t folklore. It’s science. And it’s changing how thousands of people manage chronic conditions like high cholesterol, organ transplants, and fungal infections.
Why Fat Makes Some Drugs Work Better
Not all drugs play nice with water. About 70% of new medicines being developed today are poorly soluble in water. That’s a huge problem because your body absorbs drugs mostly through your gut, and water is the main carrier. If a drug doesn’t dissolve, it doesn’t get absorbed. It just passes through and gets flushed out. That’s where fatty foods come in. When you eat fat, your body responds naturally. Your gallbladder releases bile. Your pancreas churns out enzymes. Together, they break down fat into tiny droplets and mix them with bile salts. These mixtures-called micelles-act like molecular taxis, picking up poorly soluble drugs and carrying them into your bloodstream. This isn’t theoretical. Take cyclosporine, a drug used after organ transplants to stop rejection. The original version, Sandimmune®, had wildly inconsistent absorption. Patients needed blood tests every few weeks to adjust doses. The newer lipid-based version, Neoral®, uses oil and surfactants to mimic the body’s natural fat-processing system. Studies show it boosts absorption by 20-30%. That means more consistent levels, fewer side effects, and less guesswork for doctors.How Lipid-Based Formulations Are Built
Pharmaceutical companies didn’t just start telling people to eat more butter. They reverse-engineered how the body handles fat and built drugs around it. The most common type is called a SEDDS-Self-Emulsifying Drug Delivery System. These are liquid mixtures packed into soft gel capsules. Inside, you’ll typically find:- 30-60% oil (often medium-chain triglycerides or MCTs from coconut or palm oil)
- 20-50% surfactants (like Tween 80 or Cremophor EL, which help mix oil and water)
- 10-30% cosolvents (like Transcutol HP, which keeps the drug dissolved until it hits the gut)
Real-World Impact: Patients Who Notice the Difference
For patients, the shift from traditional pills to lipid-based versions isn’t just about numbers on a lab report. It’s about daily life. Take fenofibrate, a cholesterol-lowering drug. The old version, Lopid®, had to be taken three times a day with meals. Many patients missed doses because it was too complicated. The lipid-based version, Tricor®, works once daily-even without a high-fat meal. A 2022 study found 87% of patients had fewer stomach issues, and 72% preferred it. One Reddit user wrote: “I used to dread taking my cholesterol meds. Now I just swallow it with coffee and forget about it.” Another example is itraconazole, an antifungal used for stubborn infections. The capsule form needed a full meal with fat to work. Without it, absorption dropped by 40%. The liquid lipid-based version, Sporanox®, works just as well whether you’ve eaten or not. That’s huge for cancer patients or elderly people who can’t eat regularly.
When Fat Doesn’t Help-And Can Hurt
Not all drugs benefit from fat. In fact, some work worse with it. Drugs like bisphosphonates (used for osteoporosis) need an empty stomach and acidic conditions to dissolve. Eat fat, and your stomach empties slower. Your pH rises. The drug doesn’t dissolve. It just sits there. Taking these with food or fatty meals can make them useless. And then there’s the issue of variability. Not everyone digests fat the same way. People with Crohn’s disease, cystic fibrosis, or gallbladder removal often have reduced bile production. For them, even lipid-based drugs might not work as expected. One study found bioavailability dropped by up to 50% in these groups. Even healthy people vary. A high-fat meal with avocado, nuts, and olive oil triggers a stronger response than a greasy burger. The type, amount, and timing of fat matter. That’s why some lipid-based drugs still carry food-effect warnings-even if they’re better than the old versions.Cost, Access, and the Hidden Trade-Off
Lipid-based formulations aren’t cheap. Because they require complex chemistry, special capsules, and precise manufacturing, they cost 25-35% more to produce. That cost gets passed on. Sporanox oral solution can cost around $1,200 for a 30-day supply. The generic capsule? About $300. That’s a 4x difference. Insurance doesn’t always cover the pricier version unless the patient has failed the cheaper one first. For many, that gap is too wide. A patient might know the lipid version works better-but can’t afford it. Or their pharmacy doesn’t stock it. So they stick with the old pill, even if it means eating fat at the wrong time or dealing with stomach pain.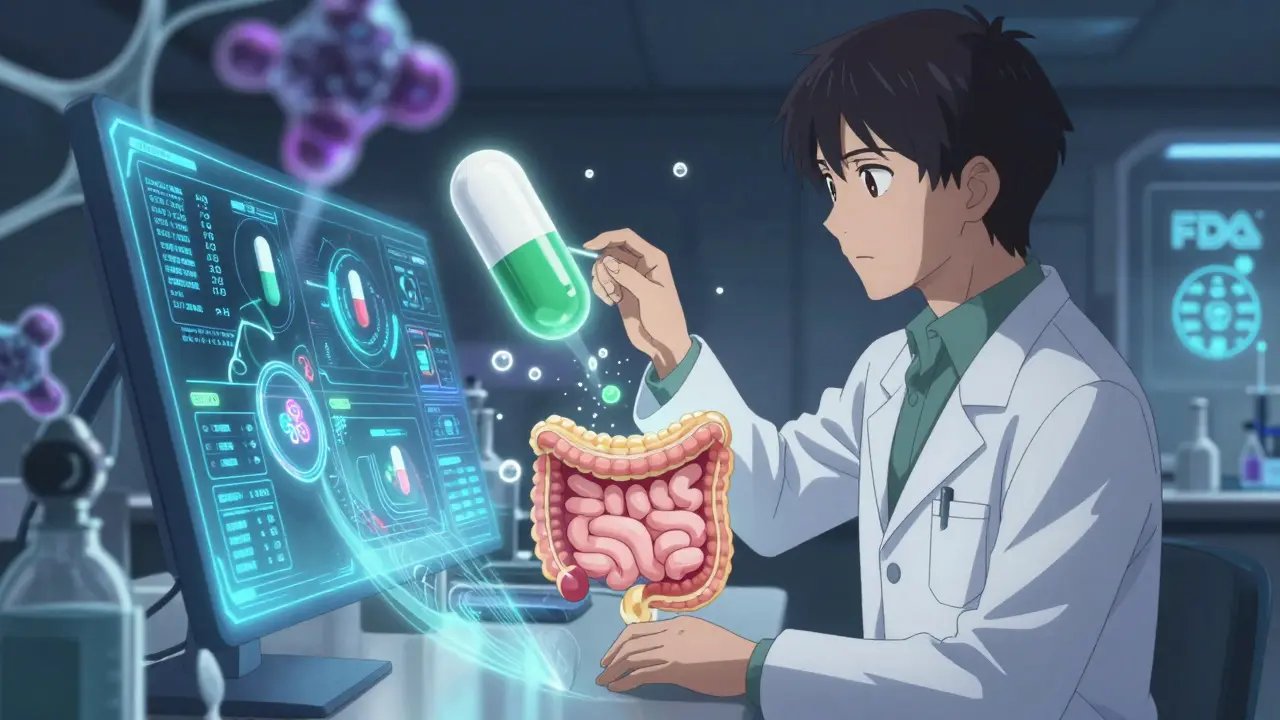
What’s Next? Smarter Pills and Personalized Dosing
The field isn’t standing still. Researchers are building “smart” lipid capsules that respond to your gut environment in real time. MIT scientists recently tested a prototype that changes how it releases the drug based on pH levels and enzyme activity. If your digestion is slow, it waits. If it’s fast, it releases early. This could eliminate food-effect warnings entirely. Another breakthrough is Matinas BioPharma’s LNC platform. Their lipid-based version of amphotericin B-a powerful but toxic antifungal-boosted bioavailability to 92%, compared to just 30% with the old form. That means lower doses, fewer kidney side effects, and better outcomes for patients with life-threatening infections. The FDA and EMA now require detailed testing of how these drugs behave with food. That’s good. It means companies can’t just slap “lipid-based” on a label and call it a day. They have to prove it works.What You Should Do
If you’re on a medication that might be affected by food:- Check the label. Does it say “take with food” or “take on an empty stomach”?
- Ask your pharmacist: Is this a lipid-based formulation? If so, does it still need fat to work?
- If you have a digestive condition (IBD, gallbladder removal, etc.), tell your doctor. Your dosing might need adjustment.
- Don’t assume all fats are equal. MCTs (coconut oil, MCT oil) are more effective than saturated fats from fried foods.
- Don’t skip doses because you didn’t eat fat. If your drug is lipid-based and you forgot to eat, take it anyway. It’s better than nothing.
The Bigger Picture
Fatty foods and lipid-based medications aren’t a gimmick. They’re a smart adaptation of biology. For decades, we tried to force drugs to dissolve in water. Now we’re learning to work with the body’s natural systems. This shift is why more than 40 lipid-based drugs have been approved by the FDA since 2000. It’s why the market is growing at 8.2% a year. And it’s why, in the next decade, we’ll likely see more drugs designed to match how you eat-not force you to change how you live. It’s not magic. It’s medicine that finally understands food isn’t just fuel-it’s part of the delivery system.Do all lipid-based medications need to be taken with fatty food?
No. While many lipid-based formulations were originally designed to work better with food, newer versions are engineered to be consistent regardless of what you eat. For example, Tricor® (fenofibrate) and Neoral® (cyclosporine) work reliably even without a high-fat meal. Always check your prescription label or ask your pharmacist-some still require food, but many don’t.
Can I use coconut oil or MCT oil to help my medication absorb better?
It’s not recommended. While MCTs are used in pharmaceutical formulations, consuming them on their own won’t reliably replicate the exact conditions needed for drug absorption. The surfactants, cosolvents, and precise ratios in these drugs are carefully balanced. Taking oil alone may not help-and could even interfere. Stick to the instructions on your prescription.
Why do some drugs work better with fat but others don’t?
It depends on the drug’s chemical properties. Drugs that are poorly water-soluble but highly permeable (BCS Class II) benefit most from fat. Think cholesterol meds, antifungals, and immunosuppressants. Drugs that need an acidic environment (like bisphosphonates) or are already water-soluble (BCS Class I) don’t gain anything-and may even absorb worse with fat.
Are lipid-based medications safer than regular pills?
They can be. Because they improve absorption, lower doses are often needed, which reduces side effects. For example, patients on lipid-based cyclosporine report fewer kidney and stomach issues than those on older versions. But they’re not risk-free. Some people have allergic reactions to surfactants like Cremophor EL. Always report unusual symptoms to your doctor.
Why are lipid-based drugs so expensive?
They’re harder to make. The ingredients are more costly, the capsules require special packaging to stay stable, and manufacturing requires advanced lab equipment and expertise. Production costs are 25-35% higher than regular tablets. Until generic versions become available, the price stays high. Some insurance plans require you to try cheaper options first before covering the lipid version.
Can I switch from a regular pill to a lipid-based version on my own?
No. Even if a lipid-based version exists, switching without medical supervision can be dangerous. Dosage isn’t always directly equivalent. Your body may absorb the drug faster or slower, which can lead to under- or overdosing. Always consult your doctor or pharmacist before changing how you take your medication.







Sally Denham-Vaughan January 1, 2026
Wow, I had no idea fat was basically a drug taxi. My grandma always made me eat butter with my medicine and I thought she was just being old-school. Turns out she was a genius. Now I just take my cyclosporine with avocado toast and feel like a biohacker.
Bill Medley January 3, 2026
Scientifically valid. Food-effect studies are mandatory for BCS Class II compounds.
Ann Romine January 4, 2026
In some cultures, taking medicine with fatty foods is traditional-like in West Africa, where palm oil is used with herbal remedies. It’s fascinating how modern science is catching up to ancestral wisdom.
Phoebe McKenzie January 5, 2026
Big Pharma doesn't want you to know this-but they’re forcing you to eat greasy food so they can charge you $1,200 for a pill that should cost $30. They don’t care if you’re broke, sick, or just hate cooking. They want your money. And your gallbladder.
gerard najera January 6, 2026
Evolution designed digestion to handle nutrients, not synthetic molecules. We’re just retrofitting drugs into an ancient system.
Stephen Gikuma January 6, 2026
They’re using coconut oil and surfactants? That’s not medicine-that’s a chemtrail recipe. Who approved this? The WHO? The UN? I bet the WHO’s got a secret lipid agenda.
Bobby Collins January 7, 2026
They’re putting Tween 80 in my meds?? That’s the same stuff in vaccines!! This is all connected. They’re testing bio-weapon delivery systems through cholesterol pills. I’m done.
Layla Anna January 8, 2026
so like... if i take my itraconazole with a little olive oil instead of a whole meal... would that work??? i just dont wanna eat a burger at 7am 😅
Heather Josey January 8, 2026
This is an excellent and well-researched overview. I appreciate the emphasis on patient safety and the distinction between lipid-based formulations and dietary fat. Always consult your provider before altering administration protocols.
Donna Peplinskie January 8, 2026
Oh my gosh, I just realized I’ve been taking my fenofibrate with toast and jam for years… and now I’m wondering if it’s even working?? I mean, like, I’ve never had a stomach issue, but what if it’s just… not doing its job?? 😳
Olukayode Oguntulu January 9, 2026
One must interrogate the epistemological underpinnings of lipid-based delivery systems. The hegemony of Western pharmacology imposes a reductionist paradigm-reducing complex biological entanglements to mere micellar solubilization. The body, as a rhizomatic network, resists such instrumentalization. MCTs are not vehicles; they are metaphors for neoliberal biopower.
Matthew Hekmatniaz January 10, 2026
My cousin with Crohn’s told me her lipid-based drug stopped working after her gallbladder came out. She had to switch back to the old version and just eat fat at every meal. It’s not just about the pill-it’s about your whole body’s story.