Why Drug-Drug Interactions Are a Silent Threat for Older Adults
Imagine taking five or six medications every day - some for blood pressure, others for arthritis, diabetes, and sleep. Now imagine two of those pills quietly cancel each other out, or worse, team up to damage your kidneys or send your heart into chaos. This isn’t fiction. It’s everyday reality for millions of older adults. Drug-drug interactions (DDIs) are one of the most common - and preventable - causes of hospital visits in people over 65. And yet, most patients and even some doctors don’t see it coming until it’s too late.
Older adults are at higher risk because their bodies change with age. The liver slows down. The kidneys don’t filter as well. Fat and muscle balance shifts. These changes mean drugs stick around longer, build up to dangerous levels, or don’t work the way they should. Add in multiple doctors, multiple pharmacies, and over-the-counter supplements nobody tells anyone about - and you’ve got a perfect storm.
One in three seniors takes five or more prescription drugs. That’s polypharmacy. And according to the American Geriatrics Society, nearly 35% of them are on at least one medication that should be avoided or adjusted for their age. These aren’t rare cases. They’re the norm.
The Most Dangerous Interactions in Older Adults
Not all drug interactions are equal. Some cause mild dizziness. Others lead to falls, kidney failure, or heart attacks. The most dangerous ones cluster in two areas: the heart and the brain.
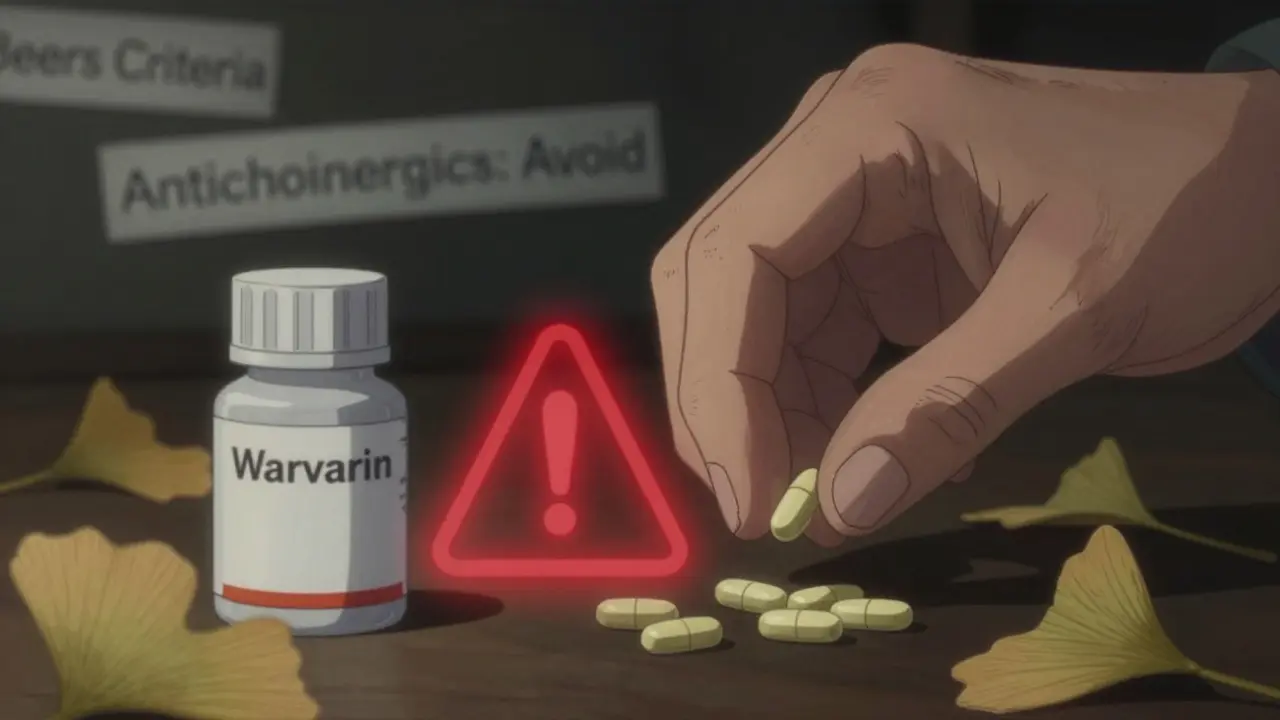
Cardiovascular drugs - like warfarin, beta-blockers, and calcium channel blockers - are involved in nearly 39% of serious DDIs. For example, combining warfarin (a blood thinner) with certain antibiotics like trimethoprim-sulfamethoxazole can spike bleeding risk by over 200%. Even common painkillers like ibuprofen can interfere with blood pressure meds, making them less effective and raising the chance of stroke.
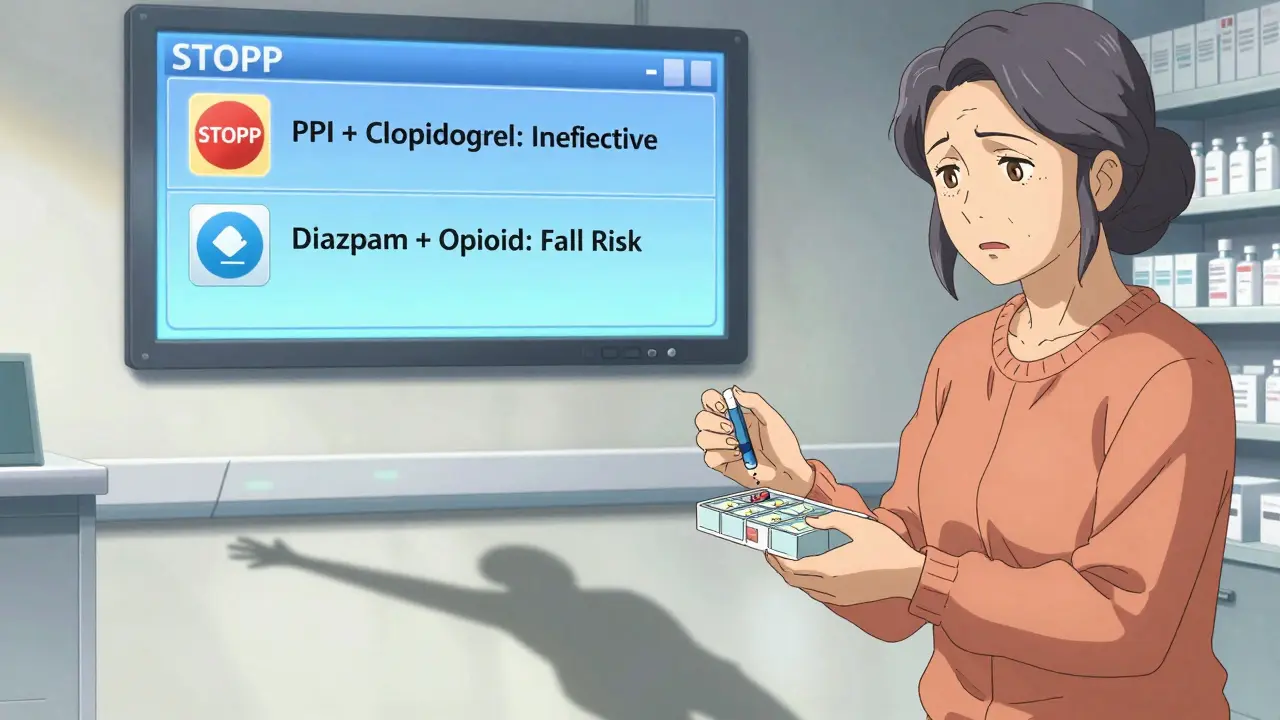
The central nervous system is the second hotspot. Sedatives, antidepressants, and antipsychotics often overlap. Take benzodiazepines like diazepam (Valium) and combine them with opioids or even some sleep aids. The result? Extreme drowsiness, confusion, and a much higher fall risk. In fact, the CDC reports that nearly half of all hip fractures in seniors are linked to sedating medications.
And don’t forget herbal supplements. Ginkgo biloba, garlic pills, and St. John’s wort might seem harmless - but they can thin the blood, interfere with antidepressants, or alter how the liver breaks down other drugs. A 2023 Merck Manual survey found that 68% of older adults never tell their doctor about these supplements. Why? They think they’re “natural,” so they’re safe. They’re wrong.
The Beers Criteria and STOPP: Your Real-World Safety Tools
Doctors don’t guess which drugs are risky. They use evidence-based lists. Two of the most trusted are the Beers Criteria and the STOPP criteria.
The Beers Criteria, updated every two years by the American Geriatrics Society, is a list of 30 drug classes that should generally be avoided in seniors - and 40 others that need dose changes based on kidney function. For example, anticholinergic drugs like diphenhydramine (Benadryl) are on the list because they cause confusion, dry mouth, and urinary retention. Yet, they’re still found in many OTC sleep aids and allergy pills.
STOPP (Screening Tool of Older Persons’ Potentially Inappropriate Prescriptions) is even more detailed. It lists 114 specific drug combinations that are dangerous for older adults. One example: prescribing a proton pump inhibitor (like omeprazole) long-term with clopidogrel. The PPI blocks the enzyme that activates clopidogrel, making the blood thinner useless - and increasing stroke risk.
Studies show hospitals that use STOPP during discharge cut inappropriate prescribing by over 34% and reduce readmissions by 22%. That’s not just a number - it’s fewer ER visits, fewer broken hips, and more time at home.
The NO TEARS Method: A Simple Checklist for Safer Medications
What should you ask your doctor or pharmacist during every visit? Use the NO TEARS framework - it’s practical, easy to remember, and covers everything.
- Need: Is this drug still necessary? Maybe your pain improved, or your blood pressure is stable. You might not need it anymore.
- Optimization: Is the dose right? Older adults often need lower doses. A pill that was fine at 50 might be too strong at 75.
- Trade-offs: Do the benefits outweigh the risks? A drug that helps with depression might make you dizzy. Is it worth it?
- Economics: Can you afford it? Many seniors skip doses because of cost. Talk to your pharmacist about generics or patient assistance programs.
- Administration: Are you taking it right? Are you crushing pills you shouldn’t? Using the wrong inhaler? Misuse is common and dangerous.
- Reduction: Can we stop any of these? Sometimes, the safest choice is to stop a drug - not add another.
- Self-management: Do you understand your whole list? If you can’t explain what each pill does, you’re at risk.
This isn’t a one-time conversation. It’s a habit. Bring your pill bottle - all of them - to every appointment. Even the vitamins.
Why Fragmented Care Makes Things Worse
Most seniors see multiple doctors. One for heart, one for joints, one for memory. Each writes prescriptions. Few talk to each other. Add in different pharmacies - one for prescriptions, another for OTCs - and the system breaks.
Studies show 67% of older adults see three or more doctors a year. That means five different people might prescribe five different drugs - none of them seeing the full picture. A 2023 study in JAMA Internal Medicine found that over half of dangerous DDIs happen during care transitions - like after a hospital stay or moving to a new doctor.
Here’s the fix: designate one provider as your medication captain. Usually, your primary care doctor. Make sure they have access to every prescription - even from specialists. Ask if your pharmacy uses an electronic system that flags interactions. If not, ask for a full medication review every six months.
What You Can Do Right Now
You don’t need to wait for a doctor’s appointment to protect yourself or a loved one. Start today.
- Make a complete list of everything you take - names, doses, why you take them. Include vitamins, supplements, and herbal products.
- Take that list to your pharmacist. Pharmacists are trained to spot DDIs. They can flag problems your doctor might miss.
- Ask: “Is there a safer alternative?” For example, instead of diphenhydramine for sleep, try melatonin or a non-drug approach like better sleep hygiene.
- Never start a new drug without asking: “What happens if I stop this one?” Sometimes, removing a drug is better than adding one.
- Use one pharmacy for all prescriptions. That way, their system can warn you about interactions across all your meds.
And if you’re helping a parent or relative - don’t assume they’re taking things correctly. Watch how they open pill bottles. Do they skip doses? Do they take things at the wrong time? A simple daily pill organizer can make a huge difference.
The Future Is Getting Better - But Slowly
Change is happening, but not fast enough. The FDA now recommends including older adults in clinical trials - but only 18% of new drug applications between 2018 and 2022 included proper geriatric data. That means we’re still guessing how drugs work in seniors.
Hospitals are starting to use AI tools that scan prescriptions in real time and flag risky combinations. Adoption jumped from 22% in 2020 to 47% in 2023. That’s progress. But many clinics still rely on paper lists and memory.
The 2025 update to the Beers Criteria will include more drug-disease interactions and better renal dosing guidance. That’s important. But the real solution isn’t just better lists - it’s better communication, better training, and better patient involvement.
Until then, you have power. You can ask questions. You can bring lists. You can say no to a new pill unless you understand why.
Frequently Asked Questions
What’s the most common drug interaction in elderly patients?
The most common dangerous interaction involves blood thinners like warfarin combined with antibiotics, NSAIDs (like ibuprofen), or even certain herbal supplements like ginkgo. These can cause serious bleeding. Another top concern is combining sedatives (like benzodiazepines) with opioids or sleep aids, which increases fall and confusion risk.
Can over-the-counter medicines cause drug interactions?
Yes - and they’re often the hidden cause. Common OTCs like antihistamines (Benadryl), NSAIDs (Advil, Aleve), and even some antacids can interfere with heart meds, blood pressure drugs, or kidney function. Many seniors don’t realize these count as “medications.” Always tell your doctor about everything you take, even if it’s “just a pill for sleep.”
How often should elderly patients have a medication review?
At least once a year - but every six months is better if they take five or more medications. After any hospital stay, surgery, or new diagnosis, a full review is essential. Don’t wait for symptoms. Prevention beats reaction.
Are there apps or tools that help track drug interactions?
Yes. Apps like Medisafe, MyTherapy, and even the free MyMedSchedule from the FDA let you log all your meds and alert you to potential interactions. Many pharmacies also offer free online medication reviews. Ask your pharmacist - they’re often the best resource.
What should I do if I think a medication is causing side effects?
Don’t stop it suddenly - especially blood pressure, heart, or psychiatric meds. Write down the symptom, when it started, and what you were taking. Bring this to your doctor or pharmacist. Often, the fix is a dose change or switching to a safer drug - not quitting altogether.
Final Thought: You’re Not Just a Patient - You’re the Manager
Medications aren’t magic bullets. They’re tools. And like any tool, they can be dangerous if used wrong. In older adults, the margin for error is small. But the power to prevent harm isn’t just in doctors’ hands - it’s in yours. Know your meds. Ask questions. Bring the list. Say no when something doesn’t feel right. That’s how you stay safe, independent, and in control - long after the prescriptions are written.





Lindsey Kidd December 24, 2025
I love this post!! 🙌 My grandma takes 7 meds and a handful of supplements, and I finally got her to use a pill organizer after reading this. She said she felt like a superhero when she could explain each one to her doctor. 🌟 #MedicationMatters
Austin LeBlanc December 25, 2025
This is why I hate how doctors just prescribe like it’s a buffet. My uncle ended up in the ER because his ‘natural’ turmeric supplement messed with his blood thinner. Nobody asked about it. Nobody. And now he’s got a $40k bill and a new diagnosis. This isn’t healthcare - it’s Russian roulette.
niharika hardikar December 26, 2025
The clinical implications of polypharmacy in geriatric populations remain grossly under-addressed within contemporary primary care frameworks. The Beers Criteria, while empirically validated, are frequently overlooked due to cognitive load and systemic fragmentation in ambulatory settings. Furthermore, the absence of standardized pharmacogenomic screening exacerbates iatrogenic risk profiles among elderly cohorts with multimorbidity. A multidisciplinary, algorithm-driven medication reconciliation protocol is imperative.
Rachel Cericola December 26, 2025
Let me tell you something - this isn’t just about pills. It’s about dignity. I’ve seen too many seniors become walking side effect lists because someone didn’t take the time to ask, 'Is this still helping?' One of my clients was on three sedatives and a benzodiazepine because her sleep was ‘bad.’ We stopped them all. She started walking her dog again. She started cooking. She started laughing. The meds weren’t helping - they were stealing her life. And the worst part? No one ever asked her if she wanted to keep taking them. You don’t need a PhD to ask, 'What’s the point?' You just need to care enough to listen.
Blow Job December 27, 2025
This is exactly why I started helping my mom manage her meds. I didn’t know anything about pharmacology, but I knew she was confused. So I made a spreadsheet. I took her to the pharmacist. I wrote down every pill, every herb, every ‘just a little’ thing she took. Turns out, she was taking two different versions of the same blood pressure med. She almost had a stroke. Now she has a color-coded chart and a sticker that says 'Ask before you add.' Simple. Life-saving.
Christine Détraz December 28, 2025
I really appreciate how practical this is. I used to think my dad’s forgetfulness was just aging - turns out he was mixing up his pills and taking double doses. Now we use the Medisafe app together. He says it feels like having a little robot assistant. And honestly? It’s brought us closer. We talk about his health more now. It’s not just about safety - it’s about connection.
John Pearce CP December 29, 2025
The erosion of medical standards in the United States is alarming. The normalization of polypharmacy, coupled with the unchecked proliferation of unregulated supplements, represents a systemic failure of both clinical oversight and patient education. The Beers Criteria are not suggestions - they are evidence-based mandates. That they are routinely ignored reflects a culture of complacency, not compassion. Until physicians are held accountable for prescribing errors in geriatric populations, this crisis will persist.
EMMANUEL EMEKAOGBOR December 29, 2025
In Nigeria, we face the opposite problem - many elderly patients cannot afford even one medication, let alone five. But when they do get prescriptions, they often combine them with traditional herbs without telling anyone. I’ve seen cases where patients on warfarin take bitter leaf tea for 'cleaning' and end up bleeding internally. The challenge isn’t just DDIs - it’s access, education, and trust. Maybe we need community health workers trained to ask: 'What else are you taking?' - not just 'What are you taking?'
CHETAN MANDLECHA December 29, 2025
I’m a pharmacist in Delhi. We don’t have AI flags or fancy apps. But we do have handwritten lists, patients bringing bags of pills, and a lot of patience. I once spent 45 minutes with a 78-year-old woman who was taking 11 meds - including 3 different antacids, 2 sleep aids, and a herbal tonic her daughter bought from a street vendor. We cut it down to 4. She cried. Not from sadness - from relief. She hadn’t slept properly in 3 years. Turns out, one of the sleep aids was making her dizzy. She just thought it was old age. We fixed it. No tech needed. Just listening.