Perioperative Anticoagulation Timing Calculator
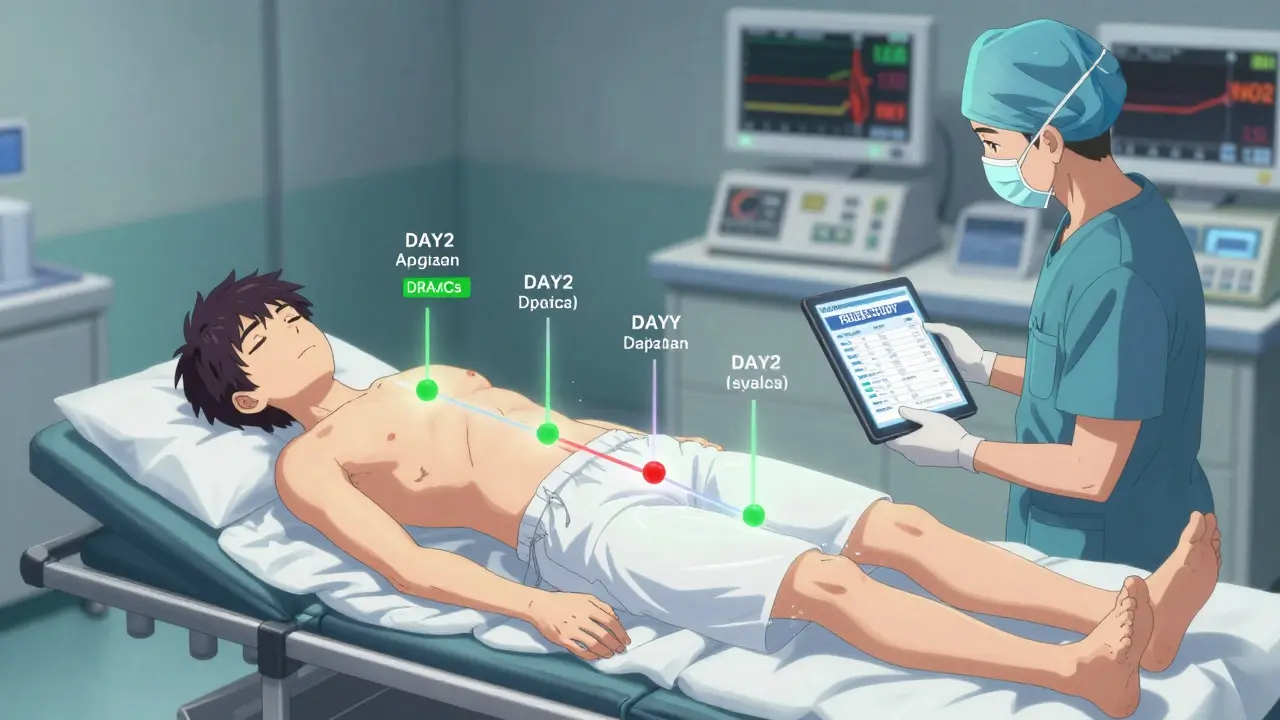
Results
When you're on blood thinners and need surgery, the biggest question isn't just how to do the operation-it's when to stop the medication, and when to start it again. Too early, and you risk a deadly clot. Too late, and you could bleed out on the table. This isn't theoretical. In 2024, the American College of Cardiology reported that 17% to 23% of patients on direct oral anticoagulants (DOACs) had major bleeding during emergency surgeries because their anticoagulation wasn't managed properly. That’s more than one in five people. And it’s preventable.
Why This Isn’t Just About Stopping Pills
People often think managing blood thinners before surgery means simply skipping a dose. It doesn’t. It’s a precision operation. You’re balancing two life-threatening risks: bleeding and clotting. The goal isn’t to make you drug-free-it’s to make you safely drug-free for the shortest time possible. The game changed in 2018 with the PAUSE study. Before that, doctors routinely bridged patients on warfarin with heparin injections while stopping their oral meds. That meant weeks of needles, hospital stays, and higher bleeding risk. The PAUSE study proved that for most people-especially those on DOACs like apixaban, rivaroxaban, or dabigatran-bridging does more harm than good. No benefit. More bleeding. That’s why the 2023 CHEST guidelines now say: suggest against bridging for nearly all patients.DOACs vs. Warfarin: Two Different Rules
Not all blood thinners are the same. And their management isn’t interchangeable. DOACs (like apixaban, rivaroxaban, dabigatran) have short half-lives. That means they leave your system quickly. For most surgeries, you stop them 1 to 4 days before, depending on the drug and your kidney function. For example:- Apixaban, rivaroxaban, edoxaban: Stop 3 days before surgery
- Dabigatran: Stop 4 days before surgery (longer if you have kidney issues)
When You Can Skip Stopping Altogether
You don’t always need to stop. For low-bleeding-risk procedures, you can often keep taking your blood thinner.- Cataract surgery
- Dental fillings or simple extractions
- Skin biopsies
- Endoscopies without biopsy
Neuraxial Anesthesia: The One Exception
If you’re getting an epidural or spinal block, the rules tighten. A spinal hematoma-bleeding around the spinal cord-is rare, but it can cause permanent paralysis. That’s why timing here is non-negotiable. The American Society of Regional Anesthesia (ASRA) says:- Stop factor Xa inhibitors (apixaban, rivaroxaban, edoxaban) at least 3 days before
- Stop dabigatran at least 4 days before
- Wait at least 24 hours after surgery to place the next epidural or spinal catheter
When to Restart After Surgery
Restarting too soon can cause bleeding. Too late, and you risk a stroke or pulmonary embolism. The 2023 CHEST guidelines recommend:- Restart DOACs 24 hours after surgery, but not before
- For minor procedures (hernia repair, cataract): restart at full dose
- For major procedures (hip replacement, brain surgery): start with half dose or prophylactic dose on day 1, then full dose on day 2 or 3
Reversal Agents: The Emergency Backup
Sometimes, surgery is urgent. You can’t wait 3 days. You need to reverse the anticoagulant now. There are two FDA-approved reversal agents:- Idarucizumab (Praxbind): Reverses dabigatran. Works in minutes. Cost: about $3,700 per vial.
- Andexanet alfa (Andexxa): Reverses factor Xa inhibitors (apixaban, rivaroxaban, edoxaban). Works in 10-15 minutes. Cost: about $19,000 per dose.
How Doctors Decide Who’s at Risk
It’s not guesswork. Doctors use two scores:- CHA₂DS₂-VASc: Measures stroke risk in atrial fibrillation. Points for age, heart failure, high blood pressure, diabetes, prior stroke, vascular disease, and female sex. A score of 2 or higher means you’re at risk.
- HAS-BLED: Measures bleeding risk. Points for high blood pressure, liver or kidney disease, stroke, labile INR, elderly, drugs or alcohol use. A score of 3 or higher means you’re more likely to bleed.

What Goes Wrong in Real Hospitals
A 2022 JAMA study of 45 academic hospitals found that 89% followed DOAC discontinuation rules correctly. But only 63% restarted them properly. That’s the gap. Common mistakes:- Restarting DOACs too early-within 12 hours of surgery
- Not checking kidney function before choosing how long to stop dabigatran
- Assuming all patients with mechanical valves need bridging (they don’t, according to 2023 CHEST)
- Using heparin bridge when it’s not needed, leading to unnecessary bleeding
What’s Coming Next
The future is faster, simpler, and safer. Ciraparantag is a new universal reversal agent currently in Phase 3 trials. It works on all anticoagulants-DOACs, heparin, even warfarin-and reverses them in under 10 minutes. If approved in 2026, it could replace idarucizumab and andexanet alfa entirely. Meanwhile, the GARFIELD-AF registry, tracking over 75,000 patients in 35 countries, is giving doctors real-world data on how patients do after surgery. That’s helping refine guidelines beyond clinical trial numbers. The bottom line? The rules are getting smarter. They’re no longer one-size-fits-all. They’re based on your body, your procedure, your risk.What You Should Do
If you’re on a blood thinner and scheduled for surgery:- Don’t stop your meds without talking to your doctor
- Ask: “Is this a high- or low-bleeding-risk procedure?”
- Ask: “Will I need bridging?” (The answer should be no, unless you have a mechanical mitral valve or a recent clot)
- Ask: “What’s my CHA₂DS₂-VASc and HAS-BLED score?”
- Write down when you last took your pill before surgery
- Confirm with your anesthesiologist if you’re getting spinal or epidural anesthesia
Can I keep taking my blood thinner before minor surgery?
Yes, for low-bleeding-risk procedures like cataract surgery, dental fillings, or skin biopsies, you can usually continue your anticoagulant without stopping. The risk of bleeding is very low, and stopping increases your chance of a stroke or clot. Always confirm with your surgeon and anticoagulation team.
Do I need a blood test before surgery if I’m on a DOAC?
No. Routine blood tests to measure DOAC levels aren’t recommended. Guidelines from the American College of Chest Physicians say they don’t improve outcomes and add cost. Timing based on the drug and your kidney function is enough.
What if I need emergency surgery and I’m on a blood thinner?
Emergency reversal agents are available: idarucizumab for dabigatran and andexanet alfa for factor Xa inhibitors. These can reverse the effect in minutes. But they carry their own risks-like blood clots-and are expensive. The priority is stopping the bleeding, then restarting anticoagulation as soon as safely possible.
Why is heparin bridging no longer recommended?
Studies like PAUSE and data from ASH 2022 show that heparin bridging doesn’t reduce clots-but it does increase major bleeding. For most patients, especially those on DOACs, the short time off the pill (3-5 days) carries a lower risk of clot than the added risk from heparin injections.
Can I take aspirin instead of my blood thinner before surgery?
No. Aspirin is not a substitute for anticoagulants like warfarin or DOACs. It doesn’t prevent strokes or clots the same way. Stopping your prescribed anticoagulant and replacing it with aspirin can put you at high risk for stroke or pulmonary embolism. Never switch without medical supervision.
How long should I wait to restart my blood thinner after major surgery?
After major surgery like joint replacement or brain surgery, restart your DOAC 1-3 days after surgery, but not before 24 hours. Start with a lower or prophylactic dose if your surgeon advises it, then move to your full dose. This reduces bleeding risk while still protecting against clots.
Is it safe to get an epidural if I’m on apixaban?
Yes, but only if you stopped apixaban at least 3 days before the procedure. The ASRA guidelines require this delay to prevent spinal hematoma. Never proceed with spinal anesthesia unless your doctor confirms the drug has cleared your system based on timing and kidney function.






Cassie Widders January 10, 2026
Been on rivaroxaban for AFib. Had a knee scope last year. Didn't stop my med. Doc said it was fine. No bleed, no clot. Just simple.
Audu ikhlas January 11, 2026
So you're telling me Nigerian doctors who dont even have basic lab equipment are supposed to follow these fancy US guidelines? This is elite medicine for rich people. We dont have idarucizumab here. We have prayer and hope. And that's enough.
Sonal Guha January 11, 2026
DOACs stop 3 days before surgery. No tests needed. Warfarin needs INR under 1.5. Bridging is obsolete. Restart 24h post-op. Simple math. Stop overcomplicating.
laura manning January 11, 2026
It is imperative to note, however, that the PAUSE study, while methodologically robust, was conducted primarily within academic medical centers in high-income nations; extrapolating its findings to community hospitals or resource-limited settings without further validation constitutes a significant clinical overreach. Furthermore, the 2023 CHEST guidelines, while authoritative, are not binding-clinical judgment remains paramount, and individual patient risk stratification must supersede algorithmic adherence.
Jay Powers January 13, 2026
Hey I was on apixaban for a clot and needed gallbladder surgery. My doc didn't even mention bridging. Just told me to skip my pill 3 days out and restart next day. No drama. No needles. I'm alive. That's all that matters. Thanks for the clear info.
Lawrence Jung January 14, 2026
The real tragedy here isn't the bleeding or the clots-it's that we've reduced human life to a checklist. We've forgotten that medicine isn't about following guidelines like a robot. It's about presence. About listening. About holding someone's hand while they're scared. The numbers don't care if you're terrified. But I do.
beth cordell January 14, 2026
As a nurse who’s done 200+ pre-op clears 🤓 I can say: if they’re getting a spinal, 3 days is NON-NEGOTIABLE. I’ve seen the charts. I’ve seen the paralysis. Don’t be the reason someone loses their legs. 💔💉 #StaySafe
jordan shiyangeni January 15, 2026
Let me be perfectly clear: anyone who suggests restarting a DOAC within 24 hours after a major orthopedic procedure is either dangerously naive or actively endangering lives. The PAUSE study had exclusion criteria that omitted 68% of real-world patients-those with renal impairment, those over 80, those on dual antiplatelet therapy. To apply these guidelines universally is not evidence-based-it’s ideological malpractice. And yes, I’ve seen the deaths. And yes, I’ve written the reports. And no, I won’t shut up about it.
Cecelia Alta January 16, 2026
So let me get this straight… you’re telling me my 82-year-old grandma with kidney failure and a mechanical valve is just supposed to skip her dabigatran for 4 days and hope for the best? No bridging? No heparin? Are you kidding me? She’s gonna die on the table and everyone’s gonna shrug and say ‘well the guidelines said so.’
Rinky Tandon January 16, 2026
The HAS-BLED score is clinically insufficient because it fails to account for polypharmacy interactions with DOACs, particularly concomitant NSAID or SSRI use, which significantly amplify bleeding risk. Moreover, the CHA₂DS₂-VASc is outdated in its gender weighting-female sex alone confers 1 point, yet women exhibit higher thrombotic risk post-surgery independent of AFib burden. We need a recalibrated, machine-learning-derived risk algorithm, not 2010-era point systems.
Ben Kono January 18, 2026
My surgeon said I could keep my apixaban for a colonoscopy. I was nervous. But he was right. No bleeding. No clot. Just a clean scope. Don't overthink it. Talk to your team.
Windie Wilson January 20, 2026
Oh wow. So now we're supposed to trust a 19k dollar drug that gives you a 13% chance of a stroke to fix a problem that didn't even need fixing in the first place? What a beautiful capitalist nightmare. Next they'll charge us $50,000 to not die from following the guidelines.
Faith Wright January 21, 2026
I used to be a nurse on the neuro floor. Saw a guy get a spinal hematoma because they gave him an epidural 18 hours after his last apixaban. He’ll never walk again. This isn’t theory. It’s real. And it’s preventable. Please, just listen to the timing rules. One mistake and someone’s life is over.
TiM Vince January 23, 2026
My mom had a pacemaker put in and was on rivaroxaban. They didn't stop it. She went home the same day. No issues. So simple. Why do we make this so hard?
gary ysturiz January 25, 2026
This is exactly the kind of info every patient needs. Clear. Practical. No fluff. If you're on blood thinners and have surgery coming up-print this out. Show it to your doctor. Ask the right questions. You deserve to be safe. You deserve to be heard. Keep sharing this. It saves lives.