SSRI & Anticoagulant Bleeding Risk Calculator
HAS-BLED Risk Assessment
The HAS-BLED score helps assess your risk of bleeding when taking SSRIs with blood thinners. Answer the questions below to get your personalized risk score.
When you’re taking a blood thinner like warfarin or a DOAC - and also an SSRI for depression or anxiety - you’re not just managing two conditions. You’re managing a hidden risk that many doctors and patients don’t fully understand: bleeding.
Why This Combination Is Riskier Than It Looks
SSRIs - drugs like sertraline, escitalopram, and fluoxetine - work by boosting serotonin in the brain. But serotonin isn’t just a mood chemical. It’s also stored inside platelets, the tiny blood cells that help clots form when you get a cut. When SSRIs block serotonin from re-entering platelets, those platelets lose their ability to stick together properly. This isn’t a side effect - it’s a direct pharmacological action. And when you add that to a blood thinner, the result is a 33% higher chance of major bleeding compared to taking the anticoagulant alone.This isn’t theoretical. A 2024 study of over 42,000 people with atrial fibrillation found that those taking both an SSRI and an anticoagulant had 6 more major bleeding events per 1,000 patients each year than those on anticoagulants alone. That’s not a small number. It’s enough to change how you think about prescribing these drugs together.
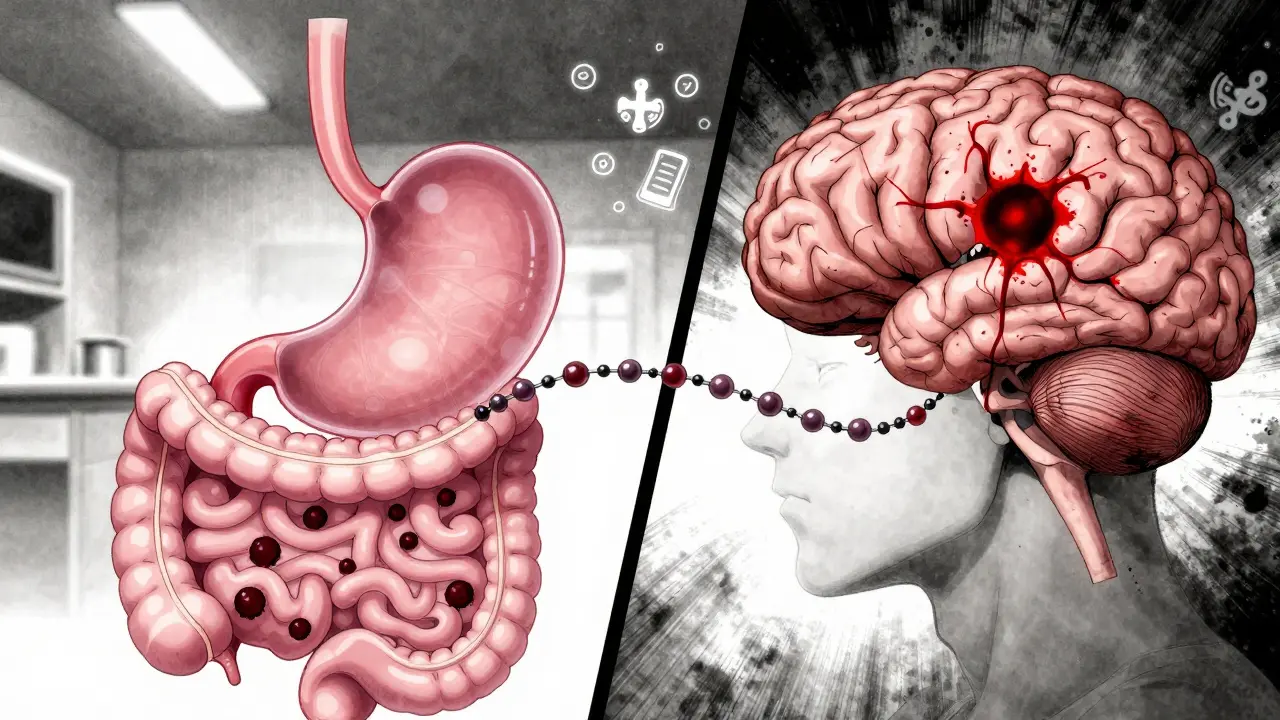
Where the Bleeding Happens - And Why It Matters
Not all bleeding is the same. The most common site? The stomach and intestines. About 58% of major bleeding events in people on this combo are gastrointestinal. That means unexplained fatigue, dark stools, or even just feeling unusually weak could be early signs. Intracranial bleeding - bleeding in the brain - makes up 17% of cases. That’s the scary one. Even a small bleed inside the skull can be life-threatening.And here’s something many don’t realize: the highest risk isn’t after months or years. It’s in the first 30 days. That’s when your body is adjusting to both drugs at once. Platelet function drops sharply during this window. After six months, the risk falls - but it doesn’t disappear. So if you’ve just started an SSRI while on a blood thinner, you need to be extra careful.
Not All Blood Thinners Are the Same
Warfarin has been around for decades. It’s cheap, but it’s finicky. It needs frequent blood tests (INR checks), and it interacts with many foods and drugs. DOACs - like apixaban, rivaroxaban, and dabigatran - are newer. They’re more predictable. And when it comes to combining them with SSRIs, they may be slightly safer.The 2024 study showed that warfarin plus an SSRI raised bleeding risk by 28%. DOACs plus SSRIs raised it by 22%. The difference wasn’t statistically significant, but it’s a trend worth noting. If you’re starting an SSRI and have a choice between warfarin and a DOAC, the DOAC is often the better option - especially if you’re older, have kidney issues, or have had bleeding before.
Not All SSRIs Are Equal - But Not for the Reason You Think
You might assume that stronger SSRIs - like paroxetine, which blocks serotonin reuptake more powerfully - would cause more bleeding. You’d be wrong. The same 2024 study found no difference in bleeding risk between paroxetine and escitalopram, even though one is much more potent at blocking serotonin uptake. That’s surprising. It suggests the effect isn’t about how strong the drug is, but that it’s there at all.That means switching from one SSRI to another won’t fix the problem. If you’re on an SSRI and a blood thinner, the risk is there regardless of which SSRI you’re taking. The only way to reduce it is to either stop the SSRI - or find a different antidepressant.
What Antidepressants Are Safer?
Not all antidepressants mess with platelets. Mirtazapine and bupropion don’t affect serotonin in platelets the same way SSRIs do. Studies show they carry little to no added bleeding risk when combined with anticoagulants. That’s why guidelines now say: if you’re at high risk for bleeding - say, you’re over 75, have a history of ulcers, or your HAS-BLED score is 3 or higher - consider switching to one of these instead.But here’s the catch: SSRIs are still the first-line treatment for moderate to severe depression. Why? Because they work. And for many people, the benefits outweigh the risks. The goal isn’t to avoid SSRIs entirely. It’s to know when they’re the right choice - and when they’re not.
How Doctors Monitor for Trouble
If you’re on both drugs, your doctor should be checking for signs of bleeding. That means:- Baselining your blood count and checking for hidden blood in your stool (fecal occult blood test)
- For warfarin users: checking your INR twice a week during the first month
- Monthly follow-ups for the first three months
And you need to know the warning signs: unusual bruising, nosebleeds that won’t stop, pink or red urine, vomiting blood or material that looks like coffee grounds, sudden severe headache, or confusion. If any of these happen, get help immediately.

Why This Interaction Is So Common - And So Undermanaged
Depression and anxiety are everywhere. So are atrial fibrillation and the need for blood thinners. About 22% of people with AFib also have depression. That’s a huge overlap. And yet, a 2022 audit found that 68% of dangerous SSRI-anticoagulant combinations happen in primary care - not in specialty clinics. Why? Because it’s easy to miss. A patient comes in for high blood pressure. They’re prescribed warfarin. Then they mention they’ve been feeling down. The doctor writes a prescription for sertraline. No one connects the dots.This isn’t just a medical issue. It’s a system issue. Many electronic health records don’t flag this interaction automatically. Many doctors don’t think about platelet effects when prescribing antidepressants. And patients? They rarely ask.
What’s Changing - And What’s Coming
The FDA updated its guidance in January 2025 to specifically warn about this interaction. New medication guides now say: “Consider non-SSRI antidepressants in patients with additional bleeding risk factors.” That’s a big step.Researchers are also working on smarter tools. The National Institutes of Health is funding a trial called PRECISION-AF, which will follow 5,000 patients on anticoagulants who are either started on an SSRI or a non-SSRI antidepressant. Results are expected in late 2026. Meanwhile, the American College of Cardiology is pushing for clinical decision support tools that combine your bleeding risk score (HAS-BLED) with your depression severity to help doctors pick the safest antidepressant.
One thing’s clear: we’re moving away from a one-size-fits-all approach. This isn’t about avoiding SSRIs. It’s about matching the right drug to the right patient.
What You Should Do
If you’re on a blood thinner and thinking about starting an SSRI - or if you’re already on both - here’s what to do:- Ask your doctor: “Is this combination right for me, given my bleeding risk?”
- Find out your HAS-BLED score. It’s a simple checklist: high blood pressure, kidney/liver disease, stroke history, labile INR, elderly, drugs/alcohol use. If you score 3 or higher, ask about alternatives like mirtazapine or bupropion.
- Don’t stop your meds suddenly. Depression can worsen if you quit an SSRI too fast. Work with your doctor to adjust safely.
- Know the signs of bleeding. If something feels off, don’t wait.
This isn’t about fear. It’s about awareness. You can manage both your heart and your mood - but you need to do it with your eyes open.







Mark Able December 19, 2025
I’ve been on warfarin for AFib and sertraline for anxiety for 3 years. No issues. My doctor never mentioned this risk. Guess I got lucky. But now I’m paranoid every time I get a nosebleed. Thanks for the scare, OP.
Dorine Anthony December 20, 2025
My grandma was on citalopram and apixaban. She started bruising like a grape and had black stools. Took three ER trips before anyone connected the dots. This needs to be screamed from the rooftops.
William Storrs December 20, 2025
You’re not alone. I was in the same boat - SSRIs and rivaroxaban. My cardiologist was clueless until I brought up the study. Now I’m on mirtazapine and my anxiety’s still under control. No more scary bruises. You can switch. It’s not a life sentence. Talk to your doc. Seriously. Do it today.
James Stearns December 21, 2025
It is, of course, an egregious oversight on the part of the medical establishment that such a well-documented pharmacodynamic interaction remains under-recognized in primary care settings. One might argue that the current paradigm of prescriptive medicine is fundamentally ill-equipped to manage polypharmacy in an aging population with comorbid psychiatric and cardiovascular conditions. The data is unequivocal. The failure to act is not merely negligent - it is a systemic dereliction of duty.
Nina Stacey December 22, 2025
so i started escitalopram last month and my dad is on eliquis and he just had a weird episode where he felt dizzy and his gums bled a little and i was like oh no no no but then i thought maybe its just stress or i dont know maybe he ate something weird and now im just sitting here wondering if i should tell him to stop his med or what like i dont even know what to do anymore
Dominic Suyo December 23, 2025
Of course the FDA waits until 2025 to slap a warning on it. Meanwhile, 42k people got a free bleeding lesson. Classic. Pharma’s playing chess while patients are stuck in tic-tac-toe. And don’t even get me started on how docs still think SSRIs are ‘safe’ because they’re ‘not opioids.’
Kevin Motta Top December 25, 2025
My therapist and cardiologist didn’t talk. I had to be the bridge. Now I carry a card in my wallet: ‘On anticoagulant + SSRI. Watch for GI bleeding.’ Simple. Life-saving.
Alisa Silvia Bila December 26, 2025
It’s wild how we treat mental health like it’s separate from physical health. You wouldn’t ignore a heart condition to treat a headache - so why treat depression like it’s just in your head? This post makes me want to scream at every doctor I’ve ever seen.
William Liu December 27, 2025
I switched from sertraline to bupropion last year after reading this exact study. No more bleeding episodes. My depression didn’t get worse. In fact, I feel more like myself. If you’re on both, don’t wait for a crisis. Ask for alternatives. You deserve to feel safe and stable.
Aadil Munshi December 28, 2025
Interesting how people think SSRIs are the only option. Have you ever considered that maybe your depression isn’t serotonin deficiency but a spiritual imbalance? Or maybe it’s the glyphosate in your food? The system is designed to keep you medicated, not healed. Bupropion is just another chemical cage. The real answer is sunlight, fasting, and rejecting pharmaceutical capitalism.
Frank Drewery December 30, 2025
I’m a nurse and I’ve seen this too many times. Elderly patient on warfarin, starts fluoxetine for ‘low mood’ after losing a spouse. Two weeks later, they’re in the ER with a GI bleed. No one asked about meds. No one checked. We need better communication. Not just between doctors - between patients and their care teams.
jessica . December 30, 2025
Big Pharma is pushing SSRIs to make you dependent so they can sell you more drugs. The bleeding risk? A cover-up. They don’t want you to know that depression is caused by vaccines and 5G towers. You think your doctor cares? He’s on their payroll. Switch to herbal tea and stop trusting the system.
Ryan van Leent December 31, 2025
Why are we even still using SSRIs? This is why America’s healthcare is a dumpster fire. You take one pill for your heart and another for your mind and boom you’re bleeding out because nobody thought to check if they’d kill you. My cousin died from this. No one even apologized. Just a $12,000 bill and a shrug.