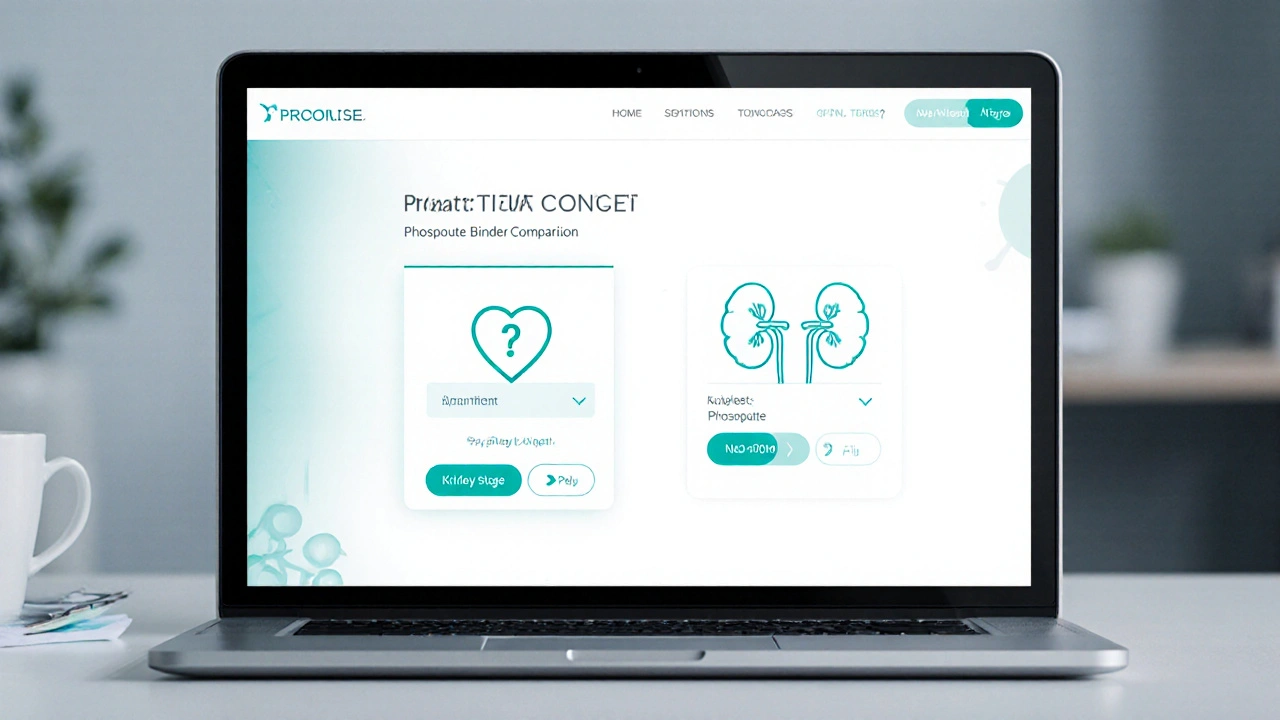
Phosphate Binder Comparison Tool
Compare Phosphate Binders
How to Use This Tool
Select your primary concern and kidney stage to get personalized recommendations about phosphate binders. This tool helps compare key features like effectiveness, side effects, and cost.
When it comes to managing phosphate levels in chronic kidney disease, PhosLo is a popular calcium acetate binder. But the market is crowded - sevelamer, lanthanum carbonate, ferric citrate, and even magnesium hydroxide all claim to be better, cheaper, or safer. This guide breaks down the science, the cost, and the real‑world pros and cons so you can decide which binder fits your lifestyle and medical needs.
Key Takeaways
- PhosLo (calcium acetate) is effective, inexpensive, and easy to take, but it adds extra calcium.
- Sevelamer hydrochloride works without calcium load and may lower LDL, yet it costs 3‑4× more.
- Lanthanum carbonate offers strong phosphate binding with minimal calcium, but pill burden and rare GI issues are concerns.
- Ferric citrate binds phosphate while also treating iron deficiency anemia - a two‑in‑one win for many CKD patients.
- Magnesium hydroxide is cheap and adds magnesium, but it can cause diarrhea and isn’t strong enough for severe hyperphosphatemia.
What Is PhosLo (Calcium Acetate)?
PhosLo is a prescription calcium acetate tablet used as a phosphate binder in patients with chronic kidney disease. Calcium acetate works by releasing calcium ions in the intestines, which then attach to dietary phosphate and form insoluble complexes that are excreted in stool. The result is a drop in serum phosphate without the need for dialysis adjustments.
Because calcium acetate is a Calcium acetate is a calcium salt that binds dietary phosphate in the gut, it also contributes extra calcium to the body - a double‑edged sword. For patients prone to vascular calcification, that added calcium can be risky. For others, it helps meet calcium needs without extra supplements.
Who Needs a Phosphate Binder?
Phosphate binders are prescribed when hyperphosphatemia is a chronic condition characterized by elevated phosphate levels in the blood. In Chronic Kidney Disease (CKD) Stage5, the kidneys can’t excrete phosphate efficiently, leading to bone‑mineral disorders, cardiovascular calcification, and higher mortality.
Typical goals are: serum phosphate<5.5mg/dL, calcium‑phosphate product<55mg²/dL², and maintaining a balanced calcium intake.
Popular Alternatives to PhosLo
Let’s look at the main competitors you’ll see on a nephrologist’s prescription pad.
- Sevelamer hydrochloride is a non‑calcium polymer binder that also lowers LDL cholesterol.
- Lanthanum carbonate is a lanthanide‑based binder with a high binding capacity and low calcium load.
- Ferric citrate is an iron‑based binder that simultaneously treats iron‑deficiency anemia.
- Magnesium hydroxide is an over‑the‑counter antacid that also binds phosphate, adding magnesium to the equation.

Decision Criteria: How to Pick the Right Binder
Every patient’s situation is unique, but these six factors usually drive the choice:
- Phosphate‑binding potency - how much tablet or dose is needed to lower phosphate by 1mg/dL.
- Calcium load - extra calcium can worsen vascular calcification.
- Side‑effect profile - GI upset, constipation, diarrhea, or metabolic disturbances.
- Cost & insurance coverage - out‑of‑pocket expenses matter a lot for chronic therapy.
- Pill burden - number of tablets per day; adherence drops after >3 tablets.
- Additional benefits - e.g., sevelamer’s LDL‑lowering or ferric citrate’s anemia control.
Side‑Effect Snapshot
| Binder | GI Effects | Metabolic Concerns | Special Notes |
|---|---|---|---|
| PhosLo (Calcium Acetate) | Constipation, mild nausea | Hypercalcemia, vascular calcification risk | Inexpensive; easy dosing (usually 2-3 tablets/day) |
| Sevelamer Hydrochloride | Flatulence, abdominal pain | No calcium load; may lower LDL cholesterol | Higher cost; 4-6 tablets/day typical |
| Lanthanum Carbonate | Mild constipation | Very low calcium load; rare liver enzyme elevation | Chewable tablets; pill burden moderate |
| Ferric Citrate | Dark stools, occasional nausea | Iron overload possible; treats anemia | Useful when anemia co‑exists |
| Magnesium Hydroxide | Diarrhea, abdominal cramping | Hypermagnesemia risk in advanced CKD | Cheapest; often OTC |
Cost Comparison (2025 US Prices)
| Binder | Typical Daily Dose | Monthly Cost (USD) | Insurance Coverage* |
|---|---|---|---|
| PhosLo (Calcium Acetate) | 2‑3 tablets | $30‑$45 | Usually covered, generic available |
| Sevelamer Hydrochloride | 4‑6 tablets | $250‑$350 | Partial coverage; prior‑auth common |
| Lanthanum Carbonate | 1‑2 chewable tablets | $180‑$240 | Partial coverage; specialty tier |
| Ferric Citrate | 2‑4 tablets | $150‑$200 | Covered for anemia indication |
| Magnesium Hydroxide | as needed | $5‑$10 | OTC, no insurance needed |
*Coverage varies by plan; always check formularies.
Best‑Fit Scenarios
- PhosLo (Calcium Acetate): Ideal for patients with low baseline calcium, no significant vascular calcification, and tight budgets.
- Sevelamer Hydrochloride: Best for those who need calcium‑free therapy, have high LDL, or have already shown calcification on imaging.
- Lanthanum Carbonate: Suited for patients who want a potent binder with low pill count and are okay with chewable tablets.
- Ferric Citrate: Perfect for CKD patients who also struggle with iron‑deficiency anemia; kills two birds with one pill.
- Magnesium Hydroxide: Good for mild hyperphosphatemia or as an adjunct when cost is the primary concern.
Practical Tips for Switching or Starting a Binder
- Check baseline calcium, phosphorus, and vitaminD levels - these guide dosing.
- Start low and titrate up: most binders need 1‑2weeks to see serum changes.
- Take the binder with meals (or immediately after) to maximize phosphate capture.
- Monitor for GI upset; consider a stool softener if constipation becomes an issue.
- Schedule labs every 1‑2months after a change to catch hyper‑ or hypo‑calcemia quickly.
- Discuss insurance beforehand - some plans require step therapy (start with calcium acetate before approving sevelamer).
Frequently Asked Questions
Can calcium acetate cause heart problems?
Can calcium acetate cause heart problems?
Excess calcium from binders can contribute to vascular calcification, which increases cardiovascular risk. The key is to keep serum calcium within target range and avoid high‑dose calcium acetate if imaging already shows calcification.
Why do I need to take my binder with every meal?
Phosphate binders work by attaching to the phosphate in the food you eat. If you skip the binder, that phosphate passes straight into the bloodstream, undoing the purpose of the medication.
Is sevelamer really better for cholesterol?
Clinical studies show sevelamer can reduce LDL by 10‑15% compared with calcium‑based binders. If you have high cholesterol on top of CKD, it may be a win‑win.
Can I mix magnesium hydroxide with calcium acetate?
Mixing is generally safe, but the combined antacid effect can cause diarrhea. Talk to your nephrologist before combining; they might prefer a single binder to simplify dosing.
How often should I get labs after changing binders?
Most doctors order serum phosphate, calcium, and PTH every 4‑6weeks after a switch. If you experience symptoms (muscle cramps, bone pain), call sooner.
Choosing the right phosphate binder isn’t a one‑size‑fits‑all decision. By weighing potency, calcium load, side effects, cost, and any extra benefits, you can land on the option that keeps phosphate under control without creating new problems. Talk to your kidney care team, compare the numbers, and pick the binder that matches your health goals and wallet.




Shivaraj Karigoudar October 2, 2025
When we step back and look at the whole ecosystem of phosphate binders, the interplay of calcium load, cost, and patient comorbidities becomes a delicate balancing act. PhosLo, being calcium acetate, provides a solid phosphate binding capacity while simultaneously supplementing calcium, which can be a boon for patients with low dietary calcium intake. However, the added calcium also raises the specter of vascular calcification, especially in long‑term dialysis cohorts where calcium‑phosphate product is already flirting with dangerous thresholds. From a pharmacoeconomic perspective, PhosLo's price tag of $30‑50 per month makes it an attractive first‑line option in resource‑limited settings. Contrast this with sevelamer, whose non‑calcium formulation sidesteps the calcification risk but carries a cost three to four times higher, often exceeding $300 per month. Lanthanum carbonate sits in the middle ground, delivering potent binding with minimal calcium, yet its pill burden can be daunting for elderly patients already juggling multiple medications. Ferric citrate introduces a clever two‑in‑one mechanism, tackling iron‑deficiency anemia while binding phosphate, but its gastrointestinal side‑effects such as constipation limit its universal applicability. Magnesium hydroxide, the cheapest of the lot, adds magnesium to the diet, which may be beneficial for some but its comparatively weak binding power makes it unsuitable for severe hyperphosphatemia. Clinical guidelines generally recommend tailoring the binder choice to the patient’s calcium profile, cardiovascular risk, and financial constraints. In practice, many nephrologists start with PhosLo for its affordability and ease of administration, monitoring serum calcium closely. If calcium rises above target, a switch to a non‑calcium binder like sevelamer or lanthanum is often considered. It is also worth noting that patient adherence is heavily influenced by pill size and frequency; PhosLo’s relatively low pill count can improve compliance. Conversely, sevelamer’s powder formulation, while flexible, may be less appealing to patients who dislike mixing powders into liquids. Another layer of complexity is drug‑drug interaction; calcium acetate can bind certain antibiotics, necessitating timing adjustments. Therefore, a multidisciplinary approach, involving dietitians, pharmacists, and social workers, is essential to navigate these nuances. Ultimately, the ‘right’ binder is the one that aligns clinical efficacy with the patient’s lifestyle, comorbidities, and budget, and regular reassessment is key.
Matt Miller October 15, 2025
Sevelamer's price can be a dealbreaker for many patients.
Fabio Max October 29, 2025
PhosLo's low cost makes it a pragmatic starter, especially when calcium levels are stable. If you need a calcium‑free option, sevelamer or lanthanum are solid backups.
Darrell Wardsteele November 11, 2025
Don't be fooled by the cheap price; extra calcium can mess up your heart vessels. Make sure your doc watches those labs.
Madeline Leech November 24, 2025
Look, the science is clear – too much calcium = risk of calcification. If you can afford it, skip calcium binders. Saving a few bucks now might cost you later.
Barry White Jr December 7, 2025
PhosLo works well costwise. Check calcium levels regularly.
Andrea Rivarola December 21, 2025
From a cultural perspective, many patients in South Asia view calcium supplementation as beneficial, which can bias them toward calcium‑based binders. This sociocultural inclination sometimes overshadows clinical guidelines that warn about hypercalcemia. As a mentor, I try to gently introduce the evidence without dismissing traditional beliefs. Balancing respect for cultural norms with evidence‑based medicine is a subtle art.
Tristan Francis January 3, 2026
Big pharma pushes sevelamer to keep profits high. Calcium binders are the cheaper truth.
Keelan Walker January 16, 2026
Thanks for the deep dive 🙏 you nailed the balance between calcium load and budget 💸 many patients forget how pill burden affects adherence 🤔 the tip about timing antibiotics with calcium is gold 🏆 keep the info coming 😊
Heather Wilkinson January 29, 2026
Happy to help! 🌟 If anyone needs more resources just shout out, I'm here 😊
Henry Kim February 12, 2026
Another point to consider is dietary phosphate intake; reducing processed foods can lessen the binder dose needed. Pairing diet changes with the right binder often yields the best outcomes.
Neha Bharti February 25, 2026
Ferric citrate shines for anemic CKD patients.