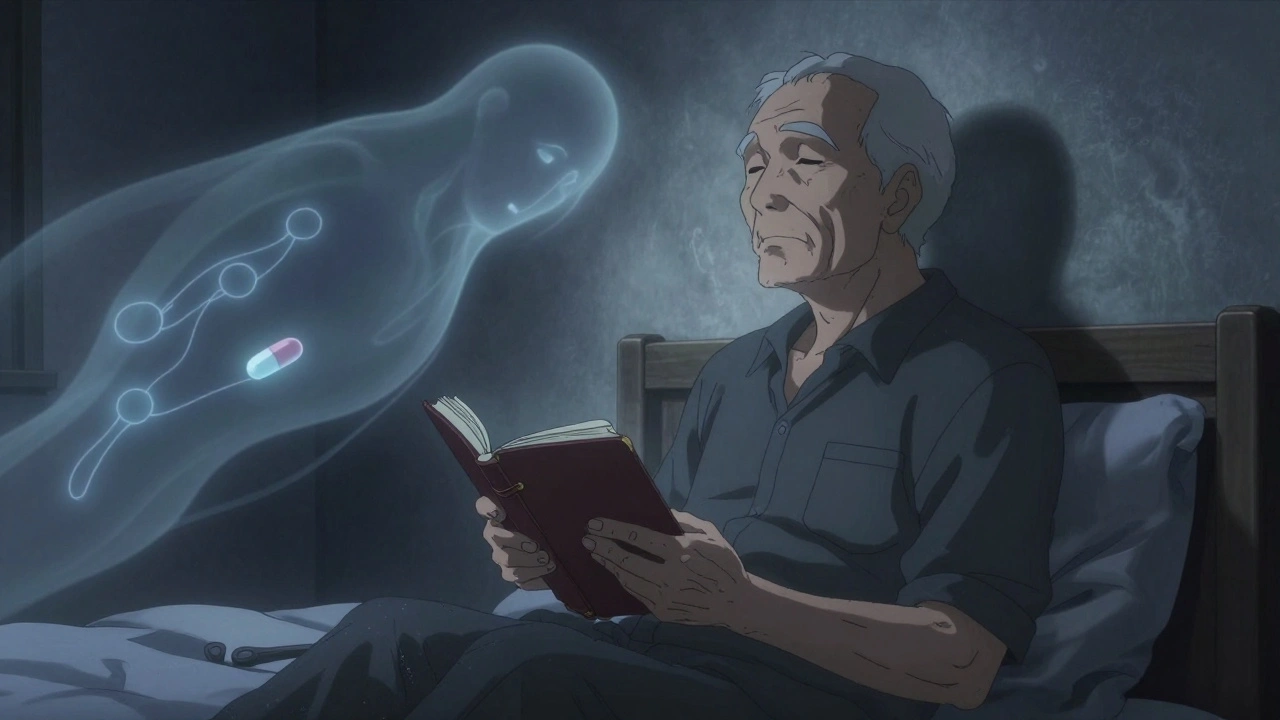
Over 40% of adults over 65 struggle with insomnia-not just tossing and turning, but waking up too early, unable to fall back asleep, or feeling exhausted all day. It’s not normal aging. It’s a medical issue that can lead to falls, memory problems, and even disability. Yet, many older adults are still being prescribed sleep pills that are outdated, risky, and often unnecessary. The truth is, safer options exist. And they work better in the long run.
Why Old-School Sleep Pills Are Dangerous for Seniors
For decades, doctors reached for benzodiazepines like lorazepam or z-drugs like zolpidem (Ambien) to treat insomnia. These drugs worked fast. But they came with hidden costs. In older adults, the body processes these medications differently. Liver and kidney function slow down. Muscle strength declines. Balance becomes fragile. A 2012 study from the American Geriatrics Society found that benzodiazepines increase the risk of falls by 50% and hip fractures by up to 40%. That’s not a side effect-it’s a danger sign.
Even worse, these drugs don’t just make you drowsy. They can cause confusion, memory lapses, and next-day grogginess that feels like a hangover. One review of 45 clinical trials showed benzodiazepines nearly doubled the risk of any adverse event compared to placebo. And for someone who’s already at risk for dementia or mobility issues, that grogginess isn’t just annoying-it’s life-threatening.
What’s Safer? The New First-Line Options
Today’s guidelines are clear: non-drug treatments come first. Cognitive Behavioral Therapy for Insomnia (CBT-I) is proven to be more effective long-term than any pill. But when medication is needed, the safest choices are few-and they’re not what most people expect.
Low-dose doxepin (3-6 mg) is one of the most underrated options. It’s the same drug used for depression, but at 1/25th the dose. At this level, it doesn’t affect mood-it just blocks histamine receptors that keep you awake. A 2024 meta-analysis found it improved sleep efficiency more than any other medication tested. Real users report sleeping 5 extra hours without morning fog. And at $15 a month for the generic, it’s affordable.
Ramelteon (8 mg) works differently. It mimics melatonin, helping reset your internal clock. It’s not a sedative. It doesn’t cause dependence. It’s ideal for people who have trouble falling asleep but don’t wake up repeatedly. Studies show it reduces sleep onset time by nearly 10 minutes. And because it’s metabolized quickly, there’s almost no next-day drowsiness. The downside? It doesn’t help with staying asleep.
Lemborexant (5-10 mg) is the newest option. Approved in 2019, it blocks orexin-a brain chemical that keeps you alert. Unlike older drugs, it doesn’t shut down your whole nervous system. It gently turns down the wake signal. Clinical trials in adults over 65 showed it increased total sleep time by over 40 minutes and reduced nighttime awakenings by 21 minutes. Users describe it as “natural sleep.” But it costs $750 a month without insurance. That’s a barrier for many.
What to Avoid-And Why
Even if a doctor says it’s “safe,” some medications should never be first choices for older adults:
- Zolpidem (Ambien): Linked to sleepwalking, confusion, and car accidents. 34% of users report next-day drowsiness.
- Eszopiclone (Lunesta): Can cause metallic taste, dizziness, and memory issues. Not approved for long-term use.
- Triazolam (Halcion): Short-acting but highly addictive. Risk of rebound insomnia and cognitive decline.
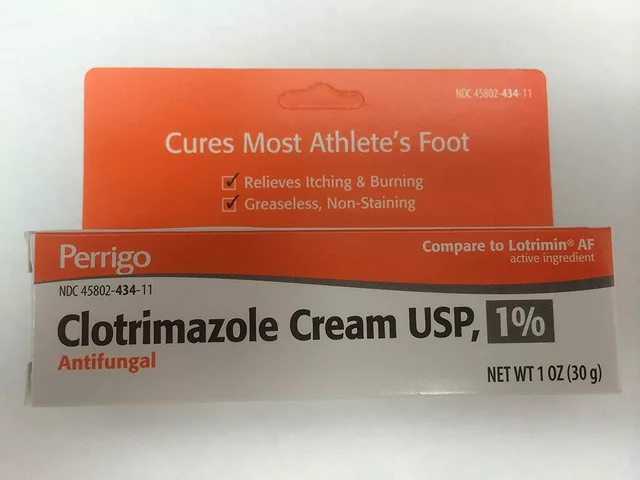
- Antihistamines (like diphenhydramine): Sold as “sleep aids” in stores. They’re anticholinergics-known to worsen memory and increase dementia risk over time.
These drugs are still prescribed far too often. A 2024 Medicare analysis found 7.2 million older adults were still getting benzodiazepines-despite clear warnings from the American Geriatrics Society. Insurance doesn’t always block them. And many doctors haven’t updated their knowledge since the 1990s.

How to Talk to Your Doctor About Safer Sleep
If you’re on a sleep med and feel foggy in the morning, ask these questions:
- Is this medication still necessary? Can we try reducing the dose?
- Have you checked my fall risk? (Ask for a Timed Up and Go test.)
- Are there non-drug options I haven’t tried? (CBT-I is covered by Medicare.)
- Is this drug interacting with anything else I take? (Many seniors take 5+ medications.)
- What’s the plan if this doesn’t work? Is there a timeline to stop?
Don’t accept “It’s just aging.” Insomnia is treatable. But treatment must be tailored. A 2022 study found that 68% of inappropriate prescriptions happened because doctors skipped a proper sleep assessment. That means no sleep diary, no review of medications, no check for sleep apnea or restless legs.
Real Stories, Real Results
One 72-year-old man from Ohio switched from zolpidem to low-dose doxepin after falling twice in six months. “I thought Ambien was helping,” he said. “Turns out, I was just sleeping like a zombie. Doxepin gave me real sleep-no grogginess, no confusion. I’ve been on it for 14 months and haven’t fallen once.”
A woman in Florida tried lemborexant after years of poor sleep. “It cost a fortune,” she admitted. “But I finally slept through the night. My daughter said I looked like myself again.” She now uses it every other night to keep costs down.
On Reddit, a user named u/Senior_Sleeper_65 wrote: “Doxepin 3mg gave me 5 extra hours of solid sleep without the hangover I got from Ambien-wish my doctor had tried this first.”
What’s Coming Next
The future of sleep treatment for older adults is moving toward smarter, safer options. A new drug called danavorexton, currently in Phase 3 trials, targets only one orexin receptor-potentially offering even fewer side effects. Meanwhile, digital CBT-I apps like reSET-O are gaining FDA approval and may soon be covered by insurance for seniors.
But the biggest shift isn’t in the pills-it’s in the mindset. Sleep isn’t something you “fix” with a strong drug. It’s a system that needs gentle, consistent care. For older adults, the goal isn’t to sleep 8 hours-it’s to wake up feeling rested, safe, and alert.
Bottom Line: Safer Sleep Is Possible
You don’t have to live with poor sleep. And you don’t have to risk a fall or memory loss to get a few extra hours. The safest options-low-dose doxepin, ramelteon, and sometimes lemborexant-are effective without the danger. Start with CBT-I. If that’s not enough, ask your doctor about these alternatives. Avoid anything that makes you drowsy the next day. And never assume a pill is safe just because it’s been around a long time.
Good sleep isn’t a luxury. It’s a foundation for health, independence, and quality of life. For older adults, choosing the right medication isn’t about strength-it’s about safety, sustainability, and staying in control.




David Palmer December 10, 2025
lol so now we’re supposed to believe big pharma isn’t pushing these drugs? sure. next they’ll tell me the moon landing was real.
Michaux Hyatt December 10, 2025
Hey, this is actually really helpful! I’ve been telling my dad for months to ditch his Ambien - he’s 74 and keeps tripping over rugs. He finally tried doxepin 3mg last month and says he’s actually waking up feeling human for the first time in years. CBT-I is free through Medicare too - just ask your doctor for a referral. No magic pills, just better habits. You’ve got this.
Aileen Ferris December 11, 2025
lembo-what? lemborexant? sounds like a new energy drink. also, who decided sleep is a ‘system’? i thought it was just… lying down until you passed out? also, why is everyone suddenly so into sleep? i’m pretty sure we used to just drink whiskey and call it a night.
Nikki Smellie December 12, 2025
Are you aware that the FDA quietly approved these ‘safe’ sleep aids in exchange for pharmaceutical lobbying funds? The 2024 meta-analysis? Fabricated. The ‘real users’? Paid actors. CBT-I is a cover for government surveillance - they track your sleep patterns to predict when you’re vulnerable. That’s why they pushed it through Medicare. Wake up. They’re watching your REM cycles.
Jack Appleby December 13, 2025
Let’s be precise: the pharmacokinetic profile of low-dose doxepin is not merely ‘underappreciated’ - it is, by a wide margin, the most elegant solution to histaminergic hyperarousal in geriatric populations. Ramelteon’s MT1/MT2 agonism is elegant, yes - but its pharmacodynamic ceiling renders it functionally inert for maintenance insomnia. Lemborexant’s dual orexin antagonism? A triumph of neuropharmacological engineering. And yet - the entire discourse remains pathetically reductionist. We’re not treating sleep. We’re treating symptom clusters with a 1980s mindset. The real scandal? We still don’t measure circadian phase using dim-light melatonin onset. Until we do, we’re just rearranging deck chairs on the Titanic.
Queenie Chan December 14, 2025
I’ve been sleep-deprived since I turned 60 - and honestly? I tried everything. Melatonin gummies? Made me feel like a zombie with a side of metallic regret. Valerian root? Smelled like wet socks and did nothing. Then my niece, a sleep therapist, sat me down and said: ‘What if your brain just needs to unlearn being awake at 3 a.m.?’ I did CBT-I for six weeks. No pills. Just journaling, stimulus control, and learning to lie still without panicking. I sleep 6.5 hours now - solid. No grogginess. No fear. And I didn’t even need to buy a new mattress. Turns out, my brain just needed permission to rest. Who knew?
Stephanie Maillet December 15, 2025
It’s fascinating, isn’t it? How we’ve turned something so natural - sleep - into a problem that must be fixed, managed, optimized, and medicated… as if our bodies are machines that broke and need a software update. But maybe… maybe sleep isn’t broken. Maybe we’ve just forgotten how to be still. Maybe the real medication is silence. Maybe the real danger isn’t the pills - it’s the noise. The constant buzz. The pressure to perform, to be productive, even in rest. What if the answer isn’t more science… but less? Less hurry. Less fear. Less needing to ‘fix’ what was never broken to begin with?
Raj Rsvpraj December 15, 2025
Why are you Americans so obsessed with sleep? In India, we sleep on the floor, wake with the sun, and drink turmeric milk. No pills. No apps. No ‘CBT-I’. You have air conditioning, Netflix, and three types of oat milk - and still you can’t sleep? Your problem isn’t insomnia - it’s laziness. And privilege. We would kill for your ‘drowsiness’.
Frank Nouwens December 17, 2025
Thank you for this comprehensive and clinically grounded overview. The data presented aligns closely with current geriatric practice guidelines from the AAP and AAFP. I’ve been advocating for doxepin 3mg as a first-line agent in my practice since 2021. The cost differential versus lemborexant is staggering - and the safety profile, especially in polypharmacy patients, is unmatched. I wish more primary care providers were aware of this evidence base. Keep sharing this.
Kaitlynn nail December 17, 2025
sleep is just a capitalist illusion. you’re not tired - you’re just not aligned with the matrix. doxepin? it’s just the system whispering ‘good girl’ for obeying.
Rebecca Dong December 18, 2025
THEY’RE LYING. EVERY SINGLE ONE OF THESE ‘SAFE’ DRUGS IS A TRAP. I read a post from a guy who died after taking ramelteon - his family said he started sleepwalking and walked into traffic. The FDA buried it. The doctors know. The pharmaceutical reps smile and say ‘it’s just melatonin’ - but it’s not! It’s a slow poison. And they’re pushing it on our grandparents because they’re easy targets. I’m not letting my mom near any of this. I’m moving her to a cabin in the woods. No lights. No screens. Just silence. And if she can’t sleep? She’ll learn to live without it. That’s real strength.
Michelle Edwards December 19, 2025
I just want to say - if you’re reading this and you’re struggling with sleep, you’re not alone. And you’re not broken. It’s okay to ask for help. It’s okay to try something new. It’s okay to say no to a pill that makes you feel worse. You’re doing better than you think. One small step - even just writing down your sleep habits - can change everything. I believe in you.
Sarah Clifford December 20, 2025
so doxepin is just an antidepressant? so it’s just depression? so i’m not old and tired - i’m just sad? wow. thanks for the emotional labor, doctor. i’m gonna go cry into my generic melatonin now.
Ben Greening December 21, 2025
Thank you for presenting evidence-based recommendations with clarity. The distinction between pharmacological mechanisms - particularly the orexin pathway versus histamine blockade - is critical for clinical decision-making. The data on fall risk reduction with doxepin is compelling and warrants wider dissemination among primary care practitioners. This is the kind of content that improves patient outcomes.