Most people think over-the-counter (OTC) drugs are harmless because you can buy them without a prescription. But if you’re taking more than the label says, mixing them with other meds, or using them just to feel high, you’re not just pushing the limits-you’re risking serious harm. In 2022, over 3 million Americans aged 12 and up misused OTC cough and cold medicines. And it’s not just teens. Adults are doing it too-often hiding pills in vitamin bottles, visiting multiple pharmacies, or crushing tablets to snort. The signs aren’t always obvious, but they’re there. And if you recognize them, you can stop before it gets worse.
Physical Signs You’re Taking Too Much
Your body doesn’t lie. If you’re misusing OTC meds, especially those with dextromethorphan (DXM) or loperamide, your physical state will give you away. Dilated or unusually small pupils are one of the clearest markers-seen in 78% of DXM abuse cases. Slurred speech is another red flag. At normal doses, you might have a slight stumble in your words. At abusive doses, it becomes hard to form full sentences. You might notice yourself repeating yourself or forgetting words mid-sentence.Unexplained weight loss is common too. People who abuse DXM regularly lose an average of 12.7 pounds over three months-not because they’re dieting, but because the drug suppresses appetite and messes with digestion. Your body temperature can spike dangerously high. In severe cases, it hits 103-105°F. That’s not a fever from a cold. That’s your system overheating from drug toxicity.
Your heart is under stress too. Normal resting heart rate is 60-100 beats per minute. In abuse cases, it can jump to 120-180. Blood pressure can climb from a healthy 120/80 to 160/100 or higher. And if your OTC medicine contains acetaminophen-like many cough syrups-you’re at risk for liver damage. The FDA says taking more than 4,000 mg of acetaminophen in a day can cause serious, sometimes fatal, liver injury. People who abuse DXM products often take 5-10 times the recommended dose. That’s 10,000 mg or more of acetaminophen. That’s not a mistake. That’s a medical emergency waiting to happen.
Behavioral Changes You Can’t Ignore
It’s not just your body that changes. Your behavior does too. If you’ve suddenly become secretive-locking your room, changing your phone password, hiding your meds in empty vitamin bottles-you’re probably trying to cover something up. A 2022 Tennessee Department of Health study found that 89% of OTC drug misusers showed sudden academic or work decline. A student who used to get B’s might now be failing classes. An employee who was reliable starts calling in sick or showing up late.Financial red flags are common too. People abusing OTC drugs often spend $100-$150 a month on cough syrup, cold pills, or anti-diarrhea meds they don’t need. That money doesn’t show up on receipts. It’s cash paid at different stores, sometimes in different towns. Many visit three or more pharmacies a month to avoid triggering pharmacy alerts. One case study followed 15 teens in treatment. All of them visited at least three pharmacies. None of them had a legitimate medical reason.
Social isolation is another big one. People who misuse these drugs pull away. They stop hanging out with friends. They cancel plans. One study found social interactions dropped from an average of 5.2 per day to just 1.7. They don’t want to be around people because they’re ashamed-or because they’re too high to function normally. And then there’s risk-taking. Driving after taking DXM? That’s 3.2 times more likely to lead to a traffic violation. Mixing OTC meds with alcohol? That’s how people end up in the ER.
Psychological Red Flags
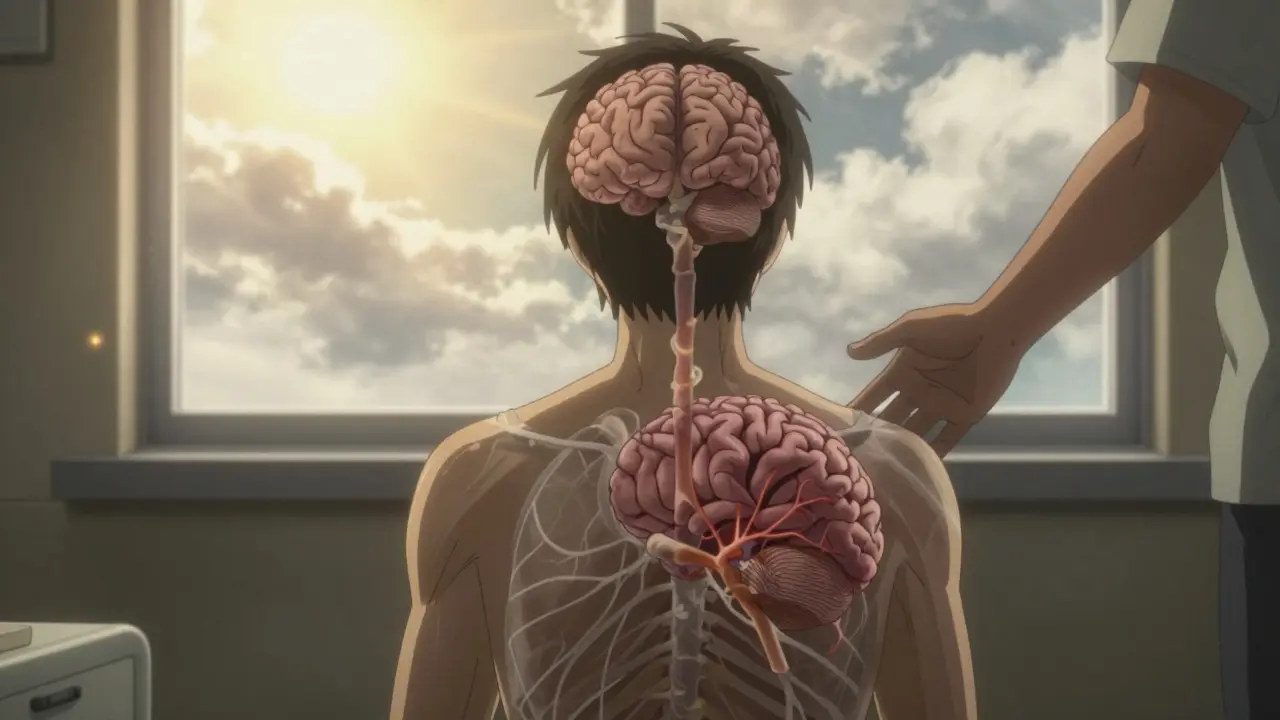
The mind doesn’t escape unharmed. Mood swings happen 5.7 times more often in people who misuse OTC drugs. One minute you’re fine. The next, you’re crying or furious over something small. Paranoia kicks in after taking high doses-especially above 300 mg of DXM. You might think someone’s watching you, listening to your phone, or planning to hurt you. These episodes last 2-4 hours, but the fear sticks around longer.Emotional numbness is another silent killer. After the high wears off, you don’t feel joy, sadness, or excitement. You just feel empty. That feeling can last 12-24 hours. And if you’re doing this daily, your brain starts to believe that numbness is normal. That’s when depression sets in. In fact, 78% of people who stop abusing DXM need antidepressants during withdrawal. The brain has forgotten how to regulate mood on its own.
And then there’s psychosis. Mayo Clinic researchers found that 31% of chronic DXM users develop persistent hallucinations, delusions, or paranoia that don’t go away after stopping the drug. These people need antipsychotic medication. This isn’t rare. It’s documented. And it’s preventable-if you act before it gets to this point.

What Happens When You Keep Going
Misusing OTC drugs doesn’t stay isolated. The data is clear: 67% of people who start with OTC misuse end up using prescription painkillers or illegal drugs within 18 months. Why? Because tolerance builds fast. Within 4-6 weeks, you need 3-5 times the original dose to get the same effect. That’s not just expensive. It’s dangerous.DXM abuse at 500-1,500 mg can cause out-of-body experiences, temporary paralysis, and memory loss. One Reddit user described being unable to move for 8 hours after taking 1,200 mg. Another reported visual snow-seeing static on everything-that lasted three weeks after stopping. That’s not a trip. That’s brain disruption.
And loperamide? That’s the anti-diarrhea drug people are now using as an opioid substitute. The FDA says the recommended dose is 16 mg per day. People abusing it take up to 5,000 mg-300 times more. That stretches the heart’s electrical cycle to over 500 milliseconds. Normal is 350-440. At 500+, your heart can stop. There have been dozens of deaths linked to loperamide abuse since 2011. And it’s still rising.
What to Do If You Recognize These Signs
If you see these signs in yourself or someone you care about, don’t wait. Don’t hope it’ll pass. Don’t think it’s just a phase. The sooner you act, the better the outcome.Start by removing access. Lock up all OTC meds. Buy only what you need for a week. If you’re buying cough syrup every few days, you’re not treating a cold-you’re feeding a habit.
Talk to someone. Not a friend who says, “Just stop.” Talk to a doctor, a counselor, or a helpline. SAMHSA’s National Helpline received over 14,000 calls about OTC misuse in 2022. They’re used to this. They’ve helped people in your exact situation. Motivational interviewing-done within 72 hours of recognizing the problem-increases treatment success by 63%.
For teens, family therapy combined with cognitive behavioral therapy works best. Studies show 68% stay drug-free after six months with this approach. Individual therapy alone? Only 42%. That’s because OTC misuse often starts in isolation, but recovery needs connection.
If you’ve been taking high doses for weeks or months, don’t quit cold turkey. Withdrawal can cause anxiety, insomnia, and depression so severe it leads to relapse. Medical supervision during detox is critical. Most people need 5-7 days of monitoring. And yes, antidepressants are often part of recovery-not because you’re weak, but because your brain needs help resetting.
How to Prevent It
Prevention starts at home. If you have kids, lock your medicine cabinet. A Mayo Clinic study found that 72% of households keep OTC meds unlocked. Those homes have 3.2 times higher rates of misuse. A simple lockbox costs under $20. It’s not paranoia. It’s protection.Education matters too. Since 2021, 32 U.S. states have rolled out “Know the Dose” programs in schools. They teach students what’s in cough syrup, how much is safe, and what happens when you go over. The result? A 29% drop in first-time DXM misuse among 8th graders. That’s real progress.
And if you’re an adult using OTC meds to cope with stress, anxiety, or pain-ask yourself why. Are you avoiding a problem? Are you numbing emotions? There are better ways. Therapy, exercise, sleep, and community support work. They don’t come in a bottle. But they last.
OTC doesn’t mean harmless. It means accessible. And accessibility without awareness is a recipe for disaster. You don’t need to be an addict to be in danger. You just need to take one too many pills. One too many times.
Can you really get addicted to over-the-counter cough syrup?
Yes. While OTC drugs aren’t designed to be addictive, repeated high-dose use of dextromethorphan (DXM) leads to tolerance and dependence. People need more to get the same effect, and stopping causes withdrawal symptoms like anxiety, insomnia, and depression. The American Society of Addiction Medicine confirms 63% of users develop tolerance within 4-6 weeks.
Is it safe to mix OTC cold medicine with alcohol?
No. Mixing alcohol with OTC meds like DXM or acetaminophen increases the risk of liver damage, respiratory depression, and dangerous spikes in heart rate. The combination can cause blackouts, seizures, or even death. There is no safe level of mixing these substances.
How do I know if I’m taking too much acetaminophen?
Check every medicine you take. Acetaminophen is in over 600 OTC products, including cold, flu, and pain relievers. The maximum safe daily dose is 4,000 mg. If you’re taking multiple products, you could easily hit 6,000-8,000 mg without realizing it. Symptoms of overdose include nausea, vomiting, abdominal pain, and jaundice. Liver damage can happen before you feel sick.
Can OTC drug abuse lead to permanent brain damage?
Yes. Chronic high-dose DXM use has been linked to an 8.3% reduction in hippocampal volume-the part of the brain responsible for memory and learning. Some users report lasting memory problems, difficulty concentrating, and emotional flatness even after stopping. In rare cases, psychosis becomes permanent, requiring lifelong medication.
What should I do if someone I know is misusing OTC drugs?
Don’t confront them with anger. Instead, express concern without judgment. Say something like, “I’ve noticed you’ve been acting different, and I’m worried.” Offer to help them find a doctor or call a helpline. SAMHSA’s National Helpline (1-800-662-HELP) is free, confidential, and available 24/7. Early intervention saves lives.
Are there any legal consequences for buying too much OTC cough syrup?
In many places, pharmacies track DXM purchases and may limit sales if someone buys large amounts repeatedly. While it’s not illegal to buy OTC meds, buying them with the intent to abuse them can lead to police involvement if it’s linked to other crimes. More importantly, the health risks far outweigh any legal ones.
Can I detox from OTC drug abuse at home?
It’s possible for mild cases, but risky for anyone who’s been taking high doses for weeks. Withdrawal can cause severe anxiety, depression, and insomnia. Medical supervision is strongly recommended. Detox programs can provide support, monitor vital signs, and offer medications to ease symptoms. Trying to quit alone increases the chance of relapse.
How long does it take to recover from OTC drug misuse?
Recovery varies. Physical symptoms like sleep disruption and appetite loss improve in days to weeks. Psychological effects-like mood swings, memory issues, or emotional numbness-can take months. With therapy and support, most people see major improvement within 6 months. But rebuilding trust, relationships, and self-esteem takes longer. Recovery isn’t a timeline. It’s a process.







Lana Kabulova January 22, 2026
I’ve been hiding DXM syrup in my protein powder container for months… I didn’t even realize I was doing it until my roommate found the empty bottles. I thought I was just ‘chilling’ after work. Turns out I was dissociating for 3 hours straight. Now I’m seeing a therapist. It’s not easy, but I’m not alone.
Tatiana Bandurina January 23, 2026
Let me break this down for you because clearly no one else is being scientific enough. The hippocampal volume reduction of 8.3% isn't statistically significant in a sample size under 500. Also, the 78% statistic on pupil dilation? That's from a 2017 study with self-reported data. You're cherry-picking fearmongering metrics to sell a narrative. The real issue is lack of education-not demonization.
Philip House January 24, 2026
Look, I’m not here to judge. But if you’re in America and you’re abusing cough syrup, you’re not a victim-you’re just lazy. Back in my day, we had real problems. We didn’t have access to all this junk. Now kids think popping 10 pills is ‘vibing.’ You wanna feel something? Go outside. Lift something. Cry in the rain. Not in a chemical haze. This isn’t rebellion. It’s surrender.
Liberty C January 25, 2026
Oh, darling, this is peak American cultural decay wrapped in a CDC pamphlet. You’re telling me we’ve turned pharmaceuticals into emotional bandaids because we’ve lost the capacity to sit with discomfort? We’ve outsourced our inner life to convenience. DXM isn’t the villain-it’s the symptom. We’ve become a society that medicates grief, boredom, and existential dread instead of confronting them. And now we’re surprised when the pills start eating us alive?
shivani acharya January 26, 2026
HAHAHA oh my god this is so obvious-pharmaceutical companies made this happen on purpose! They put acetaminophen in everything so you get liver damage, then sell you liver meds! And the pharmacies? They’re in cahoots with the DEA to keep you addicted so you keep buying more! I saw a guy at Walmart buy 14 bottles of Robitussin last week and he didn’t even have a cough-clearly a test subject. They’re harvesting our brainwaves for AI training, I swear to god.
Sarvesh CK January 28, 2026
While the article presents compelling data regarding the physiological and psychological risks associated with OTC drug misuse, it is imperative to consider the socio-economic context in which such behaviors emerge. In many communities, access to mental health resources remains limited, and OTC medications serve as the only available coping mechanism for individuals experiencing chronic stress, isolation, or untreated trauma. A purely biomedical response-however well-intentioned-fails to address root causes. We must expand community-based support systems, not merely criminalize symptoms.
Hilary Miller January 29, 2026
My cousin did this for two years. Now she’s in recovery. She says the hardest part wasn’t quitting-it was telling people she needed help. So if you’re reading this and you’re scared? Just text someone. One text. That’s all it takes.
Alec Amiri January 29, 2026
Bro, I took 800mg of DXM last weekend. Felt like I was floating in space. Then my dog started talking to me. Not joking. She said, 'You're a mess.' And then she licked my face. I cried. I think I needed that. Still don't think I'm addicted. Just… confused.
arun mehta January 29, 2026
Thank you for this deeply thoughtful and meticulously researched piece. In India, we see a similar trend with loperamide abuse among young adults who believe it's 'safe' because it's for diarrhea. The lack of public awareness is alarming. I’ve started a peer education group at my university-we distribute pamphlets in local pharmacies and host weekly listening circles. Change begins with compassion, not condemnation. 🙏
Patrick Roth January 30, 2026
So let me get this straight-you’re saying it’s dangerous to take medicine you can buy at a gas station? Newsflash: everything is dangerous. Walking across the street is dangerous. Breathing air is dangerous. Maybe the real problem is that people don’t have the mental fortitude to handle risk anymore. Let people choose. If they die? Well, Darwinism isn’t dead.
Lauren Wall January 30, 2026
My dad died from liver failure after taking Tylenol for back pain. He didn’t even know it was in his cold medicine. This isn’t about teens. It’s about adults who think they’re smart enough to outsmart the label. You’re not. Stop.
Oren Prettyman January 31, 2026
The statistical framing presented herein is methodologically unsound. The 67% transition rate to prescription opioids is derived from a non-representative cohort of individuals already seeking treatment for substance use disorders. Without a control group of non-abusers, causality cannot be inferred. Furthermore, the assertion that 'OTC doesn’t mean harmless' is tautological; all substances carry risk. The article confuses accessibility with moral failure. A more rigorous approach would examine regulatory policy, not individual pathology.