Generic Medication Effectiveness: Do Cheap Drugs Really Work?
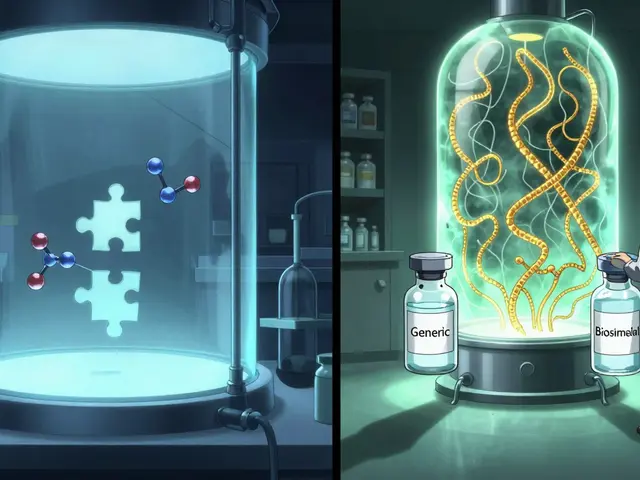
When you pick up a prescription and see it’s a generic medication, a drug that contains the same active ingredient as a brand-name version but is sold under its chemical name. Also known as non-brand drugs, they’re required by the FDA to meet the same standards for strength, purity, and performance as the original. So why do so many people still doubt they work? The truth is, generic drugs aren’t cheaper because they’re weaker—they’re cheaper because companies don’t have to spend millions on advertising or re-proving the drug’s safety. The same active ingredient, same dosage, same way it works in your body. If your doctor prescribes lisinopril and you get the generic version, it’s not a different drug—it’s the exact same one, just without the fancy packaging.
Some people worry about differences in fillers or coatings, but those don’t affect how the drug works. A 2018 study by the FDA analyzed over 1,000 generic drugs and found no meaningful difference in effectiveness compared to brand names. The same goes for common meds like metformin, atorvastatin, or sertraline. You’re not sacrificing results—you’re saving money. And if you’re on a long-term treatment, those savings add up fast. Take brand name drugs, the original version of a medication developed and marketed by the company that invented it. They often cost 10 to 20 times more than generics, even though they contain identical active ingredients. That gap exists because of patents, not performance.
What about those stories you hear—"My generic blood pressure pill didn’t work like the brand"? Sometimes, it’s not the drug. It’s the placebo effect, or maybe you switched from one generic manufacturer to another and noticed a slight difference in pill size or color. That’s normal. But if your condition worsens after switching, talk to your pharmacist or doctor. Rarely, a person might have a sensitivity to an inactive ingredient, but that’s not about effectiveness—it’s about tolerability. And if you’re using digital tools to track your adherence, like smart pillboxes or reminder apps, you’re more likely to notice if something’s off. That’s why medication adherence, how consistently a patient takes their prescribed drugs matters just as much as the drug itself. A cheap pill only helps if you take it.
There’s also a whole layer of legal and economic factors behind why generics exist. The Hatch-Waxman Act, a U.S. law that balances patent protection for innovators with faster access to affordable generics created the pathway for generic drugs to enter the market without repeating expensive clinical trials. That’s why you can now buy generic versions of drugs that used to cost hundreds a month. Companies like Teva, Mylan, and Sandoz compete to make these drugs as cheap as possible—and that competition keeps prices low.
So when you’re choosing between a brand and a generic, ask yourself: Am I paying for better results—or just better marketing? The science says no difference. The data says generics work just as well. And if you’re managing chronic conditions like high blood pressure, diabetes, or depression, sticking with a consistent, affordable option can make a bigger difference than switching to an expensive brand. The real question isn’t whether generics work—it’s why you’d ever pay more unless you have to.
Below, you’ll find real-world comparisons, cost breakdowns, and patient stories that show exactly how generic medications stack up against the brand names—no hype, no fluff, just what works and what doesn’t.
How to Track Medication Effectiveness After a Generic Switch
Learn how to track if your generic medication is working after a switch. Key signs to watch for, when to test labs, what to tell your doctor, and which drugs carry the highest risk.