Geriatric Insomnia: Causes, Risks, and Real Solutions for Seniors
When older adults struggle to sleep, it’s not just a normal part of aging—it’s geriatric insomnia, a persistent inability to fall or stay asleep in people over 65 that disrupts daily function and increases health risks. Also known as sleep disturbance in the elderly, it’s one of the most common yet overlooked conditions in senior care. Unlike younger people who might toss and turn after a stressful day, seniors with geriatric insomnia often face physical, neurological, and medication-driven barriers that make rest feel out of reach.
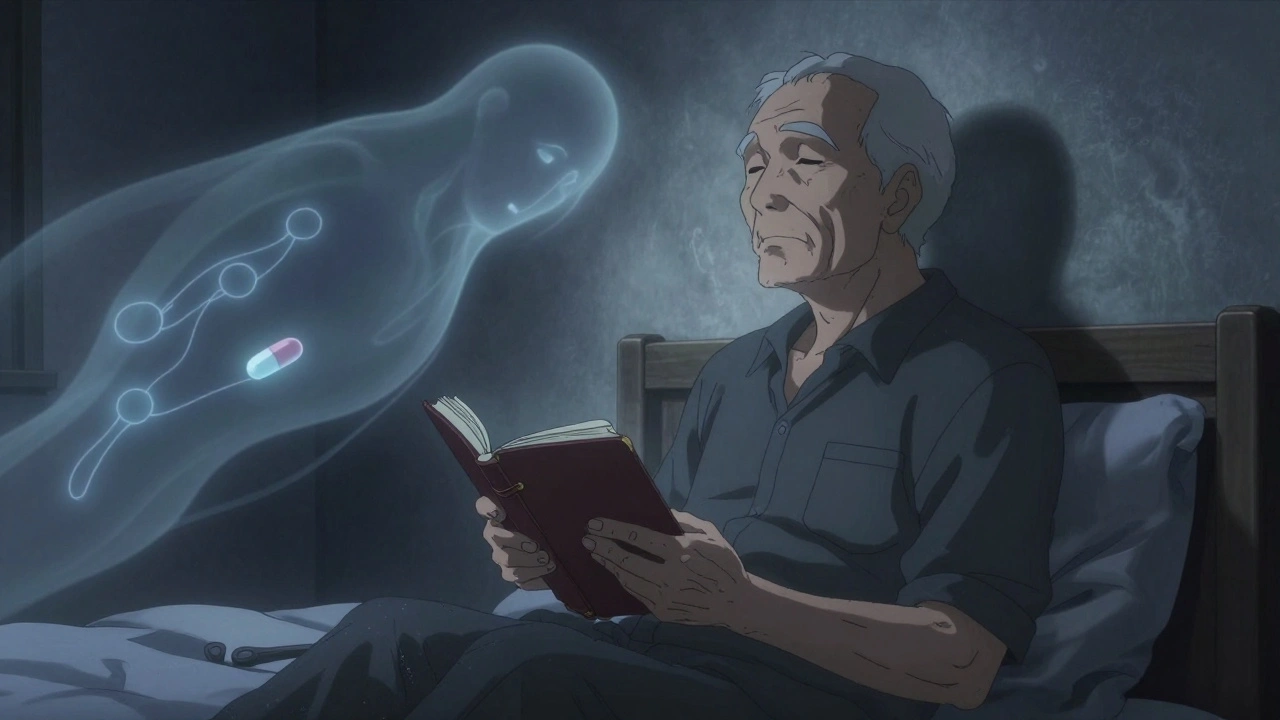
This isn’t just about feeling tired. Poor sleep in older adults links directly to higher risks of falls, memory problems, depression, and even heart disease. Many seniors take medications—like beta blockers, diuretics, or even some antidepressants—that interfere with sleep cycles. Others deal with chronic pain from arthritis, restless legs, or nighttime urination caused by prostate issues. Even something as simple as too much caffeine after noon or skipping daylight exposure can throw off their internal clock. sleep disorders in elderly, a broad category including insomnia, sleep apnea, and circadian rhythm shifts that affect aging populations often overlap, making diagnosis tricky. And because many seniors don’t report their sleep problems, doctors rarely address them unless someone else brings it up.
What makes geriatric insomnia different from regular insomnia? It’s not just the frequency—it’s the consequences. A senior who wakes up three times a night isn’t just cranky—they’re more likely to stumble in the dark, forget to take meds, or lose muscle mass from lack of recovery. And here’s the catch: many over-the-counter sleep aids, like diphenhydramine, are dangerous for older adults. They can cause confusion, dry mouth, urinary retention, and even increase dementia risk over time. That’s why treatment needs to be smarter than just popping a pill. The best approaches focus on sleep hygiene, light exposure, behavioral therapy, and carefully reviewing every medication on the list.
Some seniors find relief with simple changes: moving their bedtime earlier, getting sunlight in the morning, cutting out afternoon naps, or using a white noise machine. Others need help from a sleep specialist who understands how aging changes the brain’s sleep drive. And while insomnia treatment, structured methods to improve sleep quality in people with chronic difficulty falling or staying asleep often includes CBT-I (Cognitive Behavioral Therapy for Insomnia), many clinics still don’t offer it to older patients—despite strong evidence it works better than pills.
What you’ll find in these articles are real stories and science-backed fixes—not guesswork. From how common drugs like statins and antihistamines sabotage sleep, to why skipping a nighttime pill can be safer than taking a sleep aid, this collection cuts through the noise. You’ll see how medication errors during care transitions can worsen sleep, how anticoagulants and blood pressure drugs interact with rest, and why tracking generic switches matters when your body’s already struggling to recharge. These aren’t abstract ideas—they’re daily battles for millions of seniors and their families. And the solutions? They’re simpler than you think, if you know where to look.
Insomnia in Older Adults: Safer Medication Choices for Better Sleep
Older adults with insomnia need safer sleep options than traditional pills. Discover the most effective, low-risk medications like low-dose doxepin and lemborexant-and why benzodiazepines should be avoided.