Tacrolimus-Azole Interaction Calculator
Why This Matters
Azole antifungals can cause dangerous spikes in tacrolimus levels, leading to kidney damage. This calculator helps adjust doses to prevent toxicity while maintaining therapeutic effectiveness.
Recommended Tacrolimus Dose
0.0 mg/day
Risk level
Key Guidelines
Voriconazole / Ketoconazole: Reduce tacrolimus dose by 50-75%
Posaconazole: Reduce dose by 25-50%
Isavuconazole: Reduce dose by 10-20%
Monitoring: Check tacrolimus trough levels daily for first 3-5 days, then twice weekly until stable.
When a transplant patient gets an infection, doctors often reach for an azole antifungal like voriconazole or posaconazole. It makes sense - these drugs work well against fungi, are taken orally, and are widely available. But if that same patient is on tacrolimus, a common immunosuppressant, things can go wrong - fast. Azoles and tacrolimus don’t just coexist; they collide in the body, causing tacrolimus levels to spike dangerously high. This isn’t theoretical. It’s happening in hospitals every week, and it’s leading to acute kidney injury, hospitalizations, and sometimes permanent damage.
Why This Interaction Happens
Tacrolimus is broken down in the liver by an enzyme called CYP3A4. Think of this enzyme as a factory worker that takes the drug apart so it can be cleared from the body. Azole antifungals - ketoconazole, itraconazole, voriconazole, posaconazole - are like sabotage agents. They bind tightly to CYP3A4 and shut it down. When that happens, tacrolimus doesn’t get metabolized. It just keeps building up in the bloodstream. The numbers are startling. Ketoconazole can push tacrolimus levels up by 300% to 500%. Voriconazole? Often 100% to 300%. Even posaconazole, considered milder, can still double tacrolimus concentrations. And because tacrolimus has such a narrow safety window - too little and the body rejects the transplant, too much and the kidneys start to fail - even a small change can be catastrophic. This isn’t just about blood levels. It’s about what happens next. Tacrolimus directly damages the kidneys by constricting blood vessels inside them. This reduces blood flow, causes inflammation, and leads to a rise in creatinine - the classic sign of kidney trouble. In one study, patients on voriconazole saw their creatinine levels double within 48 hours. That’s not a slow decline. That’s a crash.Who’s at Risk
This interaction hits hardest in solid organ transplant recipients - especially kidney, liver, and lung transplant patients. These patients are on tacrolimus for life. They’re also more likely to get fungal infections because their immune systems are suppressed. Lung transplant patients, for example, have an 85% chance of being prescribed azoles for prophylaxis. That’s nearly everyone. Some patients are at even higher risk. People with a CYP3A5 gene variant that makes them “poor metabolizers” - common in African and Middle Eastern populations - break down tacrolimus even slower. Add an azole on top, and levels skyrocket faster. Older patients, those with pre-existing kidney issues, or those on multiple other medications that also affect CYP3A4 (like certain antibiotics or antivirals) are also more vulnerable. It’s not just about the drug itself. Dosing matters. A patient on 3 mg of tacrolimus twice daily might be fine. But start them on voriconazole, and suddenly that same dose becomes the equivalent of 9 mg or more. No one adjusts for that. And when they don’t, the results are predictable.Real Cases, Real Consequences
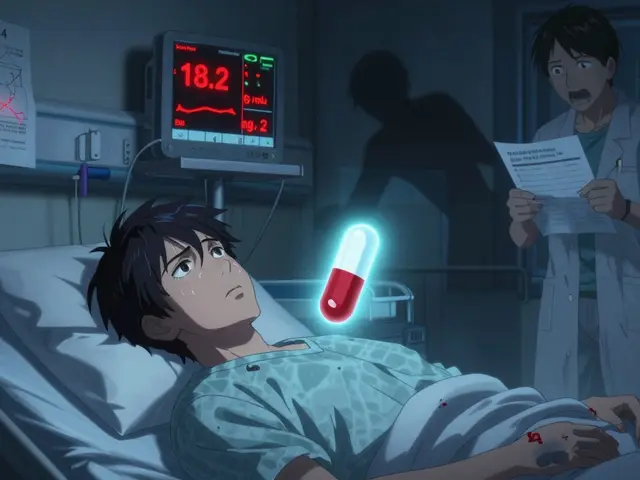
One kidney transplant patient on Reddit described waking up with swollen ankles and feeling exhausted. His last tacrolimus level was 6.5 ng/mL - perfectly normal. Three days after starting voriconazole for a suspected fungal infection, it was 18.2 ng/mL. His creatinine jumped from 1.2 to 2.8 in under 72 hours. He was hospitalized with acute kidney injury. He spent a week on IV fluids and had to switch to a different antifungal. His transplant team had to reduce his tacrolimus dose by 70% and monitor him daily. Transplant pharmacists say this happens weekly. One pharmacist in a 2022 survey said his center had at least one unplanned hospital admission per month because of this interaction. Another said they once had a patient go from stable to needing dialysis in five days. The patient survived, but his kidney function never fully recovered. These aren’t rare outliers. Studies show azole-tacrolimus interactions contribute to 15-20% of all tacrolimus-related kidney damage in transplant centers. That’s one in five cases of kidney injury tied directly to a drug interaction that could have been prevented.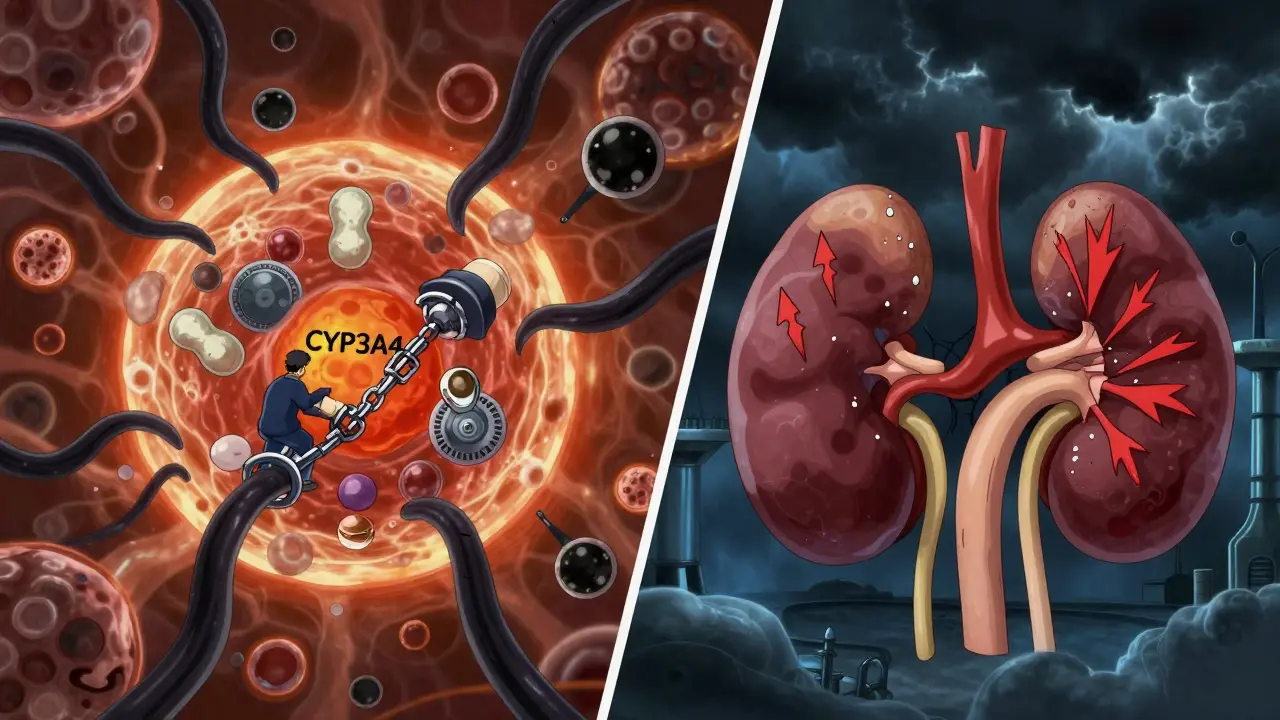
What Works: Managing the Risk
The solution isn’t to avoid azoles. It’s to manage the interaction like a controlled explosion - with strict protocols. When an azole is needed, tacrolimus must be reduced before the azole even starts. For strong inhibitors like ketoconazole or voriconazole, cut the tacrolimus dose by 50-75%. For posaconazole, reduce by 25-50%. For isavuconazole - a newer azole that’s much weaker at inhibiting CYP3A4 - only a 10-20% reduction is needed. Many centers now have standardized order sets built into their electronic health records to make this automatic. Monitoring is non-negotiable. Trough levels should be checked daily for the first 3-5 days after starting the azole. Then twice a week until levels stabilize. Some centers now use concentration-to-dose ratios (C/D ratios), which account for how much drug the patient is taking versus what’s in their blood. This method has been shown to reduce nephrotoxicity by 22% compared to just checking troughs alone. A 2020 protocol at a major transplant center reduced toxicity events by 60% after they implemented a fixed 75% dose reduction for posaconazole. That’s not luck. That’s science.Alternatives That Don’t Crash Tacrolimus
Sometimes, the best move is to avoid the interaction entirely. Echinocandins - caspofungin, micafungin, anidulafungin - don’t touch CYP3A4. They’re given intravenously, so they’re not ideal for outpatient use, but they’re safe. Lipid-based amphotericin B also has minimal interaction risk, though it carries its own kidney toxicity. That’s a trade-off, but it’s often better than a tacrolimus spike. Isavuconazole is emerging as a promising alternative. It’s an azole, yes - but it’s a weak CYP3A4 inhibitor. Studies show it only increases tacrolimus levels by 30-50%, compared to 100-300% with voriconazole. The problem? Insurance often won’t cover it as first-line. Cost is still a barrier, even when safety is better.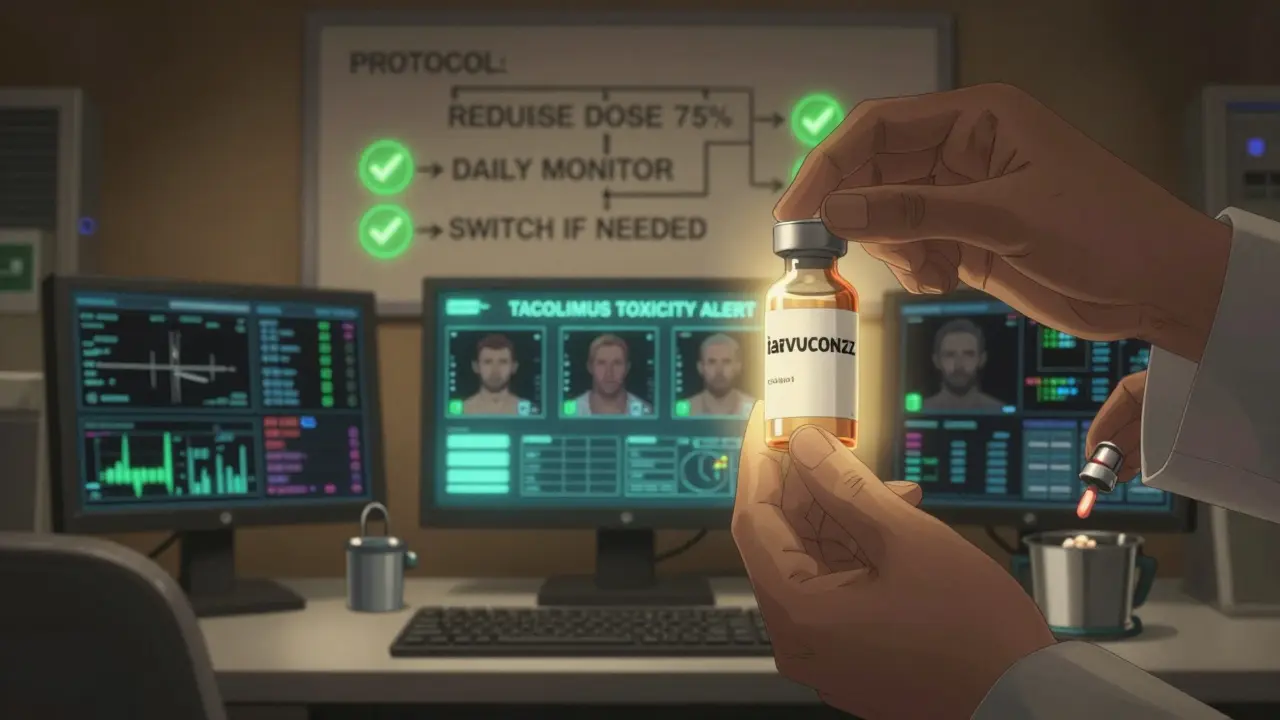
The Bigger Picture
Transplant medicine is getting better. Survival rates are higher than ever - 97% of kidney transplant patients are alive one year after surgery. But living longer means managing more complications. Infections are still the leading cause of death in the first year after transplant. So antifungals aren’t going away. The real problem isn’t the drugs. It’s the lack of consistent protocols. A 2022 survey found that 25-30% of transplant centers still had at least one severe toxicity case per year from this interaction. Why? Because some teams still rely on old habits. Some don’t have alerts in their EHR. Some don’t check levels daily. Some assume “it’s just a little increase.” The FDA approved a new extended-release form of tacrolimus in 2023. It smooths out the peaks and valleys in blood levels, which may reduce kidney damage. And by 2024, guidelines will start factoring in CYP3A5 genetics - meaning some patients might need less dose reduction than others. But until those changes are universal, the safest approach remains simple: reduce tacrolimus before starting the azole. Monitor levels like your life depends on it - because it does. And always ask: Is there a safer alternative?What Patients Should Know
If you’re on tacrolimus and your doctor prescribes an antifungal, ask:- Is this an azole? If yes, how will my tacrolimus dose change?
- Will my levels be checked daily at first?
- What are the signs of kidney trouble - swelling, less urine, fatigue, nausea?
- Is there a non-azole option that’s just as effective?
Bottom Line
Azoles and tacrolimus are a dangerous combo. Not because the drugs are bad. But because we’ve known about this interaction for nearly 30 years - and we still don’t handle it well enough. The science is clear. The protocols exist. The data shows we can prevent most of these cases. The only thing missing is consistent execution. This isn’t about one patient. It’s about every transplant recipient who’s been put at risk because a simple step - reducing a dose, checking a level - was skipped. The tools are here. The knowledge is here. Now it’s time to use them.Can azoles and tacrolimus be used together safely?
Yes, but only with strict precautions. Tacrolimus dose must be reduced by 50-75% before starting strong azoles like voriconazole or ketoconazole. Blood levels need to be checked daily for the first 3-5 days, then 2-3 times weekly until stable. Isavuconazole is a safer azole option, causing smaller increases in tacrolimus levels. Never start an azole without adjusting the tacrolimus dose first.
How quickly do tacrolimus levels rise after starting an azole?
Levels can spike within 24-48 hours. In some cases, patients have seen their tacrolimus levels double or triple in just two days. This is why daily monitoring is required immediately after starting an azole - waiting longer risks kidney damage before you even realize there’s a problem.
What are the signs of tacrolimus-induced kidney damage?
Early signs include decreased urine output, swelling in the legs or ankles, unexplained fatigue, nausea, and a rising creatinine level on blood tests. Creatinine rising by 50% or more from baseline is a red flag. If you’re on tacrolimus and notice any of these, contact your transplant team immediately - don’t wait.
Why not just stop tacrolimus if the azole is needed?
Stopping tacrolimus risks organ rejection. The immune system can attack the transplanted organ within days. That’s far more dangerous than elevated tacrolimus levels - which can be managed. The goal isn’t to stop the drug, but to lower the dose enough to prevent toxicity while still preventing rejection.
Are there antifungals that don’t interact with tacrolimus?
Yes. Echinocandins (caspofungin, micafungin, anidulafungin) and lipid-based amphotericin B have minimal CYP3A4 inhibition and are safer choices. Isavuconazole, a newer triazole, also causes much smaller increases in tacrolimus levels compared to voriconazole or itraconazole. However, echinocandins require IV administration, and amphotericin B can still harm the kidneys on its own.
Can genetic testing help predict this interaction?
Yes. People with the CYP3A5*1 allele (expressers) metabolize tacrolimus faster and may need higher doses. Those without it (non-expressers) are more sensitive to interactions. About 50-60% of African descent and 10-15% of Caucasians are expressers. By 2024, transplant guidelines will include CYP3A5 testing to personalize dose adjustments - making interactions easier to predict and manage.





Usha Sundar December 22, 2025
This is why I stopped trusting hospital protocols. My cousin got put on voriconazole, no dose adjustment, and ended up in ICU. They didn't even check his levels for three days. It's not a surprise-it's negligence dressed as routine.
And now he's on lifelong dialysis because no one bothered to read the damn drug interaction sheet.
Christine Détraz December 23, 2025
I work in transplant pharmacy and I see this every single week. The worst part? It’s not the doctors who forget-it’s the system. EHR alerts are buried under 17 other warnings. Nurses don’t have time to double-check. Pharmacists are stretched too thin.
But when we do intervene? Lives change. I had a liver transplant patient last month whose creatinine dropped 40% in 72 hours after we cut tacrolimus before starting isavuconazole. It’s not magic. It’s just basic pharmacology.
Why aren’t we doing this everywhere?
John Pearce CP December 24, 2025
Let me be perfectly clear: this is a direct consequence of liberal medical training. In my time at Johns Hopkins, we were drilled on CYP450 interactions from day one. Now? Students memorize flashcards and rely on apps that don’t even flag azole-tacrolimus as "critical"-just "moderate."
It’s not just incompetence. It’s ideological. We’ve replaced rigor with convenience. And now patients are paying the price with failing kidneys.
Until we restore discipline to medical education, this will keep happening. And it will keep being called an "unfortunate interaction" instead of what it is: preventable malpractice.
CHETAN MANDLECHA December 25, 2025
Bro, I’m a med student in Mumbai and we got this exact case in our pharmacology lecture last month. Professor said, "If you give an azole to someone on tacrolimus without adjusting, you’re not a doctor-you’re a hazard."
And honestly? It’s wild how many places still don’t have protocols. We had a guy in our hospital ward last year-same story. Swelling, no urine, creatinine at 4.2. They didn’t even know what voriconazole did to tacrolimus.
Someone needs to make a viral TikTok about this. Like, "Don’t let your transplant die because of a fungal infection."
Ajay Sangani December 26, 2025
It’s funny how we call this a "drug interaction" like it’s some cosmic accident. But it’s not. It’s a human failure. We’ve known about CYP3A4 inhibition since the 90s. We’ve got the data. We’ve got the tools. We’ve got the guidelines.
So why do we keep pretending we don’t?
Maybe because admitting we keep making the same mistake means we have to change. And change is hard. Especially when it means admitting that the system we trust is broken.
But what’s harder? Living with a failing kidney… or living with the guilt of knowing you could’ve stopped it?
Gray Dedoiko December 28, 2025
My sister’s a kidney transplant recipient and she’s been on tacrolimus for 8 years. She just got prescribed posaconazole for a sinus infection last month. I made sure she asked her team about dose adjustment-she did, and they cut it by 40% and checked levels daily. She’s fine now.
But I know so many people who didn’t have someone to advocate for them. This post? It’s a lifeline. Thank you for writing it.
People need to know: if you’re on tacrolimus, don’t take any new med without asking about interactions. Even OTC stuff. Even garlic supplements. Seriously.
Aurora Daisy December 28, 2025
Oh, so now we’re blaming the doctors because they didn’t read a 20-page pharmacology paper before prescribing? How about we blame the FDA for approving azoles without mandatory interaction alerts? Or the EHR companies for burying critical warnings under "low priority"?
Let’s not pretend this is about individual negligence. It’s about a broken system that treats patients like data points until they crash.
And yes, I’m British. We’ve had this figured out since 2015. But hey, at least you’re catching up. Slowly. With a cane.
Paula Villete December 30, 2025
Just had a 68-year-old patient on tacrolimus start isavuconazole. Dose reduced by 20%, levels checked daily. Creatinine stayed stable. No dialysis. No ICU.
It’s not hard. It’s not expensive. It’s not even that time-consuming.
So why does it feel like we’re reinventing the wheel every time?
Maybe because we’re more comfortable with heroics than with consistency.
Also-typo: "concentration-to-dose rations" should be "ratios". But the point still stands. You’re right. This is fixable. We just need to stop pretending it’s not.
Georgia Brach December 31, 2025
Let’s be honest: this post is performative. You’re not trying to help patients-you’re trying to make yourself look like a hero who "finally" exposed this "hidden" danger. It’s been in every transplant textbook since 2002.
And your "alternatives" section? Echinocandins are IV-only, expensive, and still carry renal risk. Lipid amphotericin? More nephrotoxic than tacrolimus in some cases. Isavuconazole? Still an azole. Still inhibits CYP3A4. Just less.
There is no magic bullet. There’s only vigilance. And if you’re not checking levels daily, you’re not doing your job.
Stop pretending this is a systemic failure. It’s a failure of execution. And execution requires discipline, not blog posts.