Medication Reconciliation: What It Is and Why It Saves Lives
When you’re taking multiple drugs—whether for high blood pressure, diabetes, or chronic pain—medication reconciliation, the process of comparing a patient’s current medication list with newly prescribed drugs to avoid errors. It’s not just paperwork; it’s a safety net that stops dangerous mix-ups before they happen. This isn’t something that only happens in hospitals. It matters every time you switch doctors, get discharged from the ER, or start seeing a new pharmacist. A simple mistake—like forgetting you take warfarin or not telling your new doctor about your daily aspirin—can lead to a stroke, a bleed, or even death.
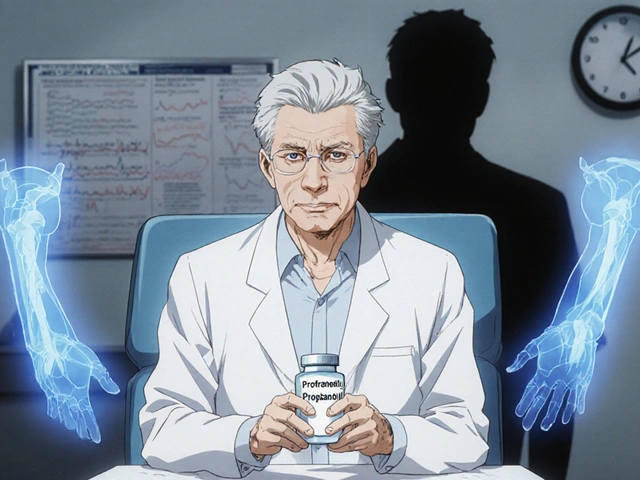
Drug interactions, when two or more medications clash in your body, causing harmful side effects are one of the biggest reasons medication reconciliation exists. Think about someone on blood thinners who starts taking a new painkiller without telling their doctor. Or an elderly patient on five different pills who gets prescribed an antihistamine that raises their blood pressure. These aren’t rare cases. The FDA estimates that over 1.5 million Americans are harmed each year by medication errors, and nearly half of those happen because no one checked the full list. That’s why pharmacy safety, the system of checks and protocols that prevent harmful medication mistakes is built around this simple step: write down everything you take, bring it to every appointment, and ask, "Is this still right for me?"
Medication errors, mistakes in prescribing, dispensing, or taking drugs that lead to harm don’t always come from bad intent. Often, they come from bad communication. A doctor assumes you’re still taking a drug your old doctor stopped. A pharmacist fills a new script without knowing you’re allergic to a dye in a generic version. A caregiver forgets to mention you’ve been skipping pills because they’re too expensive. Medication reconciliation fixes these gaps by forcing everyone involved—patients, nurses, pharmacists, doctors—to look at the full picture. It’s not about trust. It’s about verification.
You don’t need to be a senior or have a complex illness to benefit. Even if you take just two or three meds, a new prescription can throw everything off. That’s why the best time to do medication reconciliation is before you leave the hospital, before you start a new treatment, and every time your meds change. Bring your pills in a bag. Write down the names, doses, and why you take them. Ask your pharmacist to review them. If you’re switching providers, ask for a copy of your current list. Don’t assume someone else is keeping track. Your life depends on it.
Below, you’ll find real stories and expert advice on how medication reconciliation connects to everything from generic drug safety to managing insulin, avoiding allergic reactions to inactive ingredients, and protecting seniors from dangerous combinations. These aren’t theoretical guides. They’re practical tools used by people who’ve been through the system—and lived to tell the story. What you’ll read here isn’t just about pills. It’s about staying alive when the system is stacked against you.
How to Prevent Medication Errors During Care Transitions and Discharge
Medication errors during care transitions are a leading cause of preventable harm. Learn how medication reconciliation, pharmacist involvement, and better communication can stop these errors before they happen.