Medication Switch Monitoring: What You Need to Track When Changing Drugs
When you switch from one medication to another, your body doesn’t just flip a switch—it reacts. Medication switch monitoring, the process of tracking how your body responds when changing prescriptions. Also known as drug transition management, it’s not optional if you’re on long-term meds like blood thinners, antidepressants, or beta blockers. Skipping this step can lead to rebound symptoms, dangerous interactions, or even hospital visits. Think of it like tuning a car after swapping engines—you don’t just crank the key and hope for the best.
Side effects during switch, the physical and emotional changes that happen when stopping one drug and starting another are real and often misunderstood. Someone switching from Propranolol to another beta blocker might feel dizzy or fatigued not because the new drug is bad, but because their body is adjusting. Same with switching anticoagulants—stopping warfarin and starting a DOAC can cause temporary clotting risks if the overlap isn’t timed right. These aren’t random glitches. They’re predictable patterns, and medication adherence, how consistently you take your drugs during the transition is what keeps you safe. Digital tools like smart pillboxes and reminder apps help, but they’re only as good as the plan behind them.
And then there’s drug interactions, when your new medication clashes with something else you’re taking. It’s not just about the new pill. It’s the NSAID you take for back pain, the antihistamine for allergies, or even that herbal supplement you think is harmless. Antipsychotics paired with QT-prolonging drugs? That’s a cardiac risk. Statins and certain antibiotics? Liver enzymes can spike. These aren’t rare edge cases—they show up in real patient records, and they’re why monitoring isn’t just about the main drug you’re switching. It’s about the whole system.
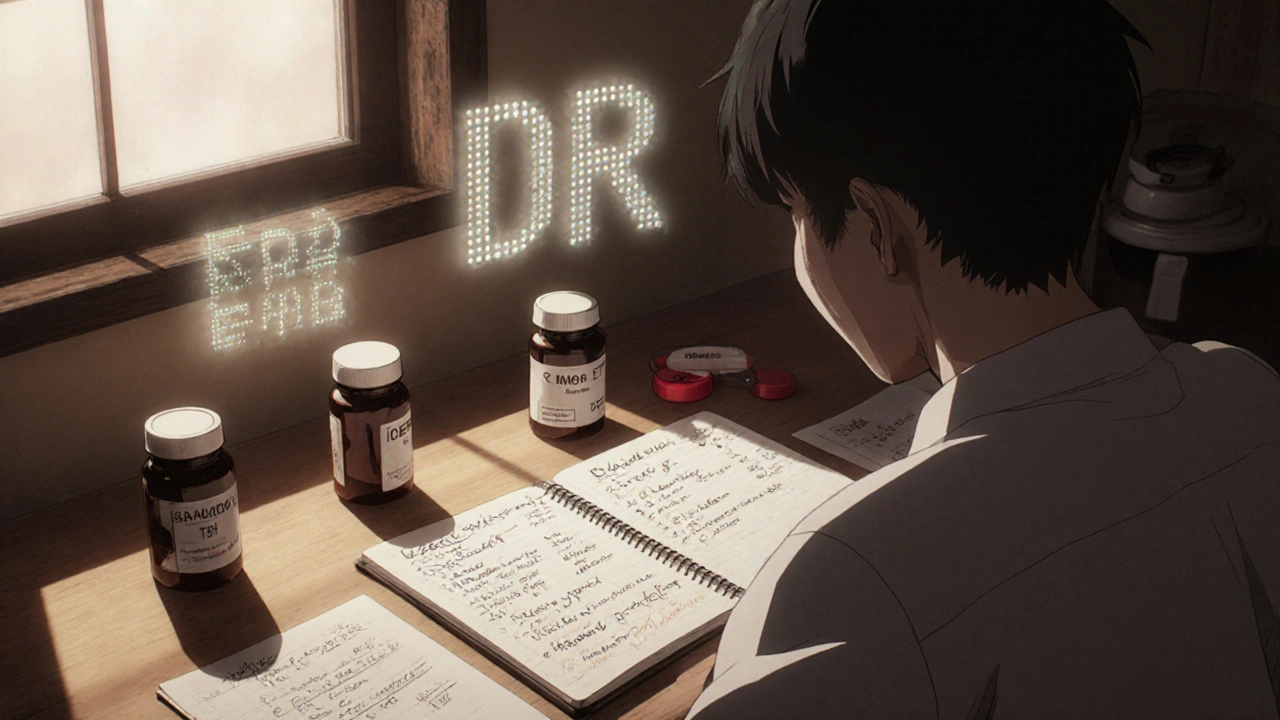
People often think once the doctor says "switch to this," the job’s done. But the real work starts after the prescription is filled. You need to track changes in mood, energy, sleep, digestion, or even skin rashes. Keep a simple log: date, drug, dose, how you felt. Did your blood pressure drop too fast? Did nausea hit right after the switch? Did your anxiety spike before the new med kicked in? These aren’t just symptoms—they’re data points that tell your doctor if the switch is working or if you need to pause, adjust, or go back.
There’s no one-size-fits-all checklist, but the best monitoring plans are simple, personal, and timely. You don’t need fancy tech. You need awareness. And you need to speak up when something feels off. The posts below cover real cases: how seniors manage anticoagulant switches after a fall, how people handle sertraline’s GI side effects during transition, how liver enzymes shift with statin changes, and why some generics require more vigilance than others. These aren’t theoretical guides—they’re lived experiences. What you’ll find here are the tools, red flags, and practical steps that actually help people make the switch safely, without guesswork.
How to Track Medication Effectiveness After a Generic Switch
Learn how to track if your generic medication is working after a switch. Key signs to watch for, when to test labs, what to tell your doctor, and which drugs carry the highest risk.