A vertigo surge at 60 mph is every driver’s nightmare. If you live with Meniere’s, you don’t need scare stories-you need straight answers. Yes, many people keep driving, but you need firm rules, a clear plan, and the confidence to cancel a trip when your body says no. This guide shows you how to judge fitness to drive, handle legal bits like DVLA notifications, and what to do if symptoms hit while you’re behind the wheel.
TL;DR:
- If you have unpredictable, disabling vertigo, don’t drive. Tell the DVLA and your insurer when required. Return to the road only when a clinician confirms your condition is controlled.
- Build a safer-driving plan: pre-drive self-check, trigger control (sleep, salt, hydration), route choices, and an emergency pull-over routine.
- Some meds help attacks but can make you drowsy. If you feel sedated, you’re not fit to drive.
- Use car tech (lane-keep, adaptive cruise), carry a “vertigo kit,” and set hard stop-rules after a flare.
- If symptoms hit while driving: signal, slow, hazards on, pull over, stop, and wait it out. Call for help if needed.
The realities of driving with Meniere’s (risks, triggers, and what you can control)
Meniere’s can hit with sudden vertigo, ear fullness, tinnitus, and fluctuating hearing. The scary part while driving isn’t the ringing-it’s the unpredictable spinning or a “drop attack.” Even milder imbalance can make speed, roundabouts, and fast head turns feel risky. That unpredictability is why driving rules are strict.
You can lower risk by managing what’s under your control. Common triggers include poor sleep, salty meals, dehydration, caffeine or alcohol, stress, bright or flickering light, and rapid head movements. Big swings in barometric pressure can stir symptoms for some people too. If you’re in the UK, think foggy dawn motorways, the A64 glare at sunset, or a sudden downpour-the visual load alone can be tough on a sensitive vestibular system.
Here’s a plain rule: if you feel off-balance before you start the car, you’re not fit to drive. Lightheaded, foggy, or “floaty” counts. Meniere’s isn’t just the classic room-spin. If your head feels wrong, skip the trip.
People often ask about tinnitus and hearing loss. Tinnitus alone doesn’t ban you from driving, and many people with hearing loss drive safely. The problem is when hearing swings distract you or reduce awareness of emergency sirens. Fix that with simple steps: mirror checks every 5-7 seconds, slightly lower music volume, and a clear car cabin (loose items can rattle and spike anxiety).
If you only remember one phrase today, let it be this: Meniere's disease driving demands a plan, not hope. Hope is not a strategy when traffic moves at 70 mph.
DVLA rules, insurance duties, and when to stop (UK-focused, with notes for elsewhere)
In the UK, medical fitness-to-drive rules come from the DVLA. Their guidance on vestibular disorders (updated regularly; check the latest) says you must not drive during sudden disabling vertigo. If these attacks are recurrent or unpredictable, you may need to tell the DVLA. Group 1 licences (cars/motorcycles) are treated differently from Group 2 (lorries/buses), with Group 2 needing stricter control for longer.
- Group 1 (cars/motorcycles): If you get sudden, disabling vertigo, stop driving. If episodes are recurrent/unpredictable, tell the DVLA. You can usually return once a clinician confirms your condition is controlled and you’re free of sudden disabling attacks. The DVLA may ask for reports from your GP/ENT.
- Group 2 (lorries/buses): Standards are tougher. Recurrent disabling vertigo often leads to revocation until you have a longer symptom-free period (commonly around 1 year) and specialist confirmation that the risk of sudden attacks has resolved. Expect a more detailed medical review.
Always tell your insurer about any condition that could affect driving. Failing to disclose can void cover-even if an incident wasn’t your fault. Be blunt with them: “I have Meniere’s; here’s how it’s managed; here’s what my specialist says.” Many insurers just note it and move on; some may ask for confirmation from your GP or ENT.
Healthcare sources worth knowing: NHS advice on Meniere’s (symptoms, triggers, treatments) and the DVLA’s “Assessing fitness to drive” guidance for vestibular disorders. Specialist clinical guidance from the American Academy of Otolaryngology-Head and Neck Surgery (2020 update) and NICE resources inform UK practice. These aren’t law, but they shape decisions.
If you’re outside the UK: rules vary. In Canada and Australia, you generally must be symptom-free and medically cleared; commercial licences are stricter. In the US, licensing is state-based, but physicians often advise no driving during attacks and for a period after, with documentation in your records. When in doubt, ask your ENT and check your state/provincial licensing website.
Question you may have: “How long after an attack should I wait?” The DVLA focuses on control and absence of sudden disabling episodes, not a fixed number of hours. In practice, many ENTs advise not driving for at least 24 hours after a significant vertigo attack and only when you feel fully recovered. If your treatment plan uses sedating meds (like prochlorperazine or diazepam during an attack), do not drive until you feel sharp-and the medication’s effects have worn off.
Your safer-driving plan (pre-drive checks, on-road tactics, and emergency steps)
Make this a routine you can run half-asleep-even if your cat wakes you before dawn. Consistency is your safety net.
Pre-drive 5-minute check:
- Rate your steadiness from 0-10 (0 = bedbound spin, 10 = solid). If below 8, don’t drive.
- Scan for triggers: sleep less than 6 hours? salty meal last night? skipped breakfast? stress spike? If two or more yes, delay or take another mode.
- Quick head-move test (seated, engine off): turn your head side-to-side briskly 5 times. Any spin or weird lag? Cancel the drive.
- Vision/attention check: can you fixate on a licence plate across the road without strain? Any visual shimmer? Iffy vision means no go.
- Medication check: if you took anything sedating (cyclizine, cinnarizine, prochlorperazine, diazepam), you’re not fit to drive until fully alert.
Route and timing choices:
- Short, familiar routes beat long, complex ones. Avoid peak glare times if light triggers you.
- Pick roads with frequent safe pull-over spots. Motorways are fine if you’re stable and know the next services; otherwise, take A-roads with lay-bys.
- Build a 15-minute buffer so you never feel rushed. Stress fuels symptoms.
In-car setup that helps:
- Seat higher with headrest aligned to the back of your head; a stable head reduces vestibular load.
- Mirrors wide and slightly down; this boosts situational awareness if hearing dips.
- Cabin cool, gentle airflow. Strong scents and warm cabins can worsen nausea.
- Keep a “vertigo kit”: water, ginger sweets, a sick bag, tissues, spare meds (in original packaging), sunglasses, a small card with emergency contacts.
Driving tactics you’ll actually use:
- Keep eyes on the horizon and the car ahead’s number plate. Avoid rapid head turns; use mirrors instead.
- Take bends smooth and steady. Late, gentle braking beats sudden, jerky moves.
- Space cushion: at 60 mph, keep at least 3 seconds behind in dry, 4-5 in rain.
- Use driver aids if you have them: lane-keep assist, adaptive cruise, blind-spot monitoring. They don’t replace you; they reduce load.
Emergency steps if symptoms hit while driving (memorise this):
- Signal immediately. Ease off the accelerator. Switch on hazards.
- Steer smoothly to a safe spot: hard shoulder, lay-by, side street, car park. Don’t fight the spin; keep movements minimal and steady.
- Stop. Handbrake/park. Keep hazards on. If needed, open windows, recline slightly, close eyes, and focus on slow breaths.
- If nausea is severe, use your sick bag; sip water once settled.
- Call for help if you’re alone or symptoms persist. If you’re in a dangerous location or feel faint, call emergency services.
- Do not resume driving until fully stable and alert. If in doubt, don’t move the car. Arrange pickup or roadside assistance.
After any roadside episode, treat it as a data point. What triggered it? What helped? Log it in a notes app. Patterns show up fast when you write them down.

Treatments, tools, and car adaptations that make driving easier
Treatment goals: fewer attacks, milder symptoms, better balance. That’s good for life and good for driving.
What clinicians use (summarised from NHS practice, NICE resources, and AAO-HNS guidance):
- Lifestyle: consistent sleep, lower stress, moderate caffeine/alcohol, hydration, and a reduced-salt diet (often 1.5-2 g sodium/day). Some people notice fewer attacks with salt control; others don’t. It’s low-risk to try.
- Preventive meds: betahistine is commonly prescribed in the UK. A 2022 Cochrane Review found uncertain benefit overall, but many clinicians and patients report fewer or milder episodes. Diuretics are also used in some cases.
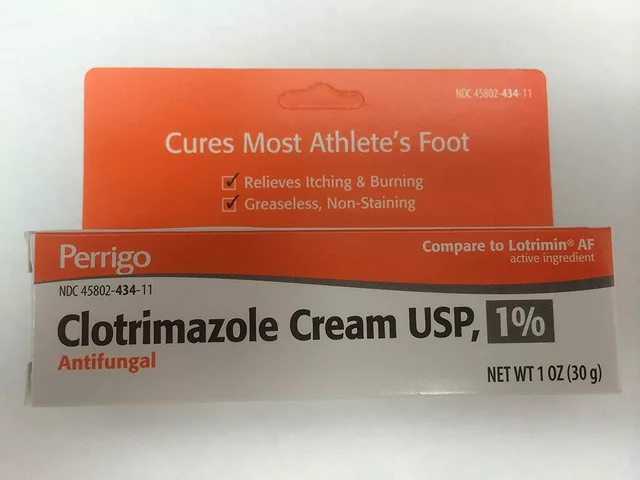
- Acute attack meds: prochlorperazine, cyclizine, or cinnarizine for nausea/vertigo. Diazepam may be used short-term in select cases. These can sedate you-if you feel drowsy or slowed, you’re not fit to drive.
- Rehabilitation: vestibular physiotherapy improves balance and reduces motion sensitivity between attacks. It’s boring homework with big payoff for driving steadiness.
- Procedures: intratympanic steroids can reduce attacks for some. Gentamicin or surgery (like endolymphatic sac decompression or labyrinthectomy) is for severe, refractory disease-these have pros/cons you must discuss with your ENT, especially regarding hearing.
- Hearing support: hearing aids, sound therapy for tinnitus, and simple communication habits in the car (agreeing hand signals, lower radio volume) keep you safer and less stressed.
Car features worth paying for when you can:
- Good LED headlights with auto-dip reduce glare and strain at night.
- Clear head-up display keeps your eyes on the road.
- Adaptive cruise and lane-keep to smooth your workload on dual carriageways.
- Wide-angle mirrors and blind-spot alerts to offset hearing dips.
- Quiet cabins reduce fatigue; test-drive on a windy day to judge stability and noise.
Alternatives when you choose not to drive:
- Public transport with timed options to avoid rush hours.
- Community transport or on-demand ride services for medical appointments.
- Work adjustments: hybrid days, flexible start times, or remote meetings. Employers in the UK have a duty to consider reasonable adjustments.
One small personal note: I map my errands in a loop around York so I’m never more than 10 minutes from a safe pull-over spot. On bright days, a cap and sunglasses live in the cup holder. It’s not dramatic-just practical. Less drama is the goal.
Checklists, decision aids, and FAQs
Quick decision guide before you pick up the keys:
- Last attack: none in the past 24 hours, and you feel fully normal now.
- Sleep: at least 6 hours.
- Hydrated and fed: yes to both; salty binge last night? If yes, reconsider.
- Medication: nothing sedating in your system.
- Head-turn test seated: no spin or lag.
- Plan B: alternative route or transport if you need to stop.
Simple rules of thumb:
- No symptoms = consider driving with your plan in place.
- Minor wobble = delay, recheck in 30-60 minutes, or ride-share.
- Any vertigo, anxiety spike, or fogginess = don’t drive. Your life is worth the taxi fare.
| Scenario | Risk on the road | What to do | Legal/administrative step |
|---|---|---|---|
| Stable for months, no recent attacks | Lower, but not zero | Follow pre-drive check, carry vertigo kit, choose routes with safe pull-overs | Usually no DVLA action if no recurrent disabling episodes |
| Occasional mild imbalance, no spins | Moderate, especially at night or in bad weather | Short daylight trips, avoid peak glare, slow head turns, extra following distance | Inform insurer about diagnosis; DVLA notification if advised by clinician |
| Recent disabling vertigo episode | High | Don’t drive; wait until fully recovered; discuss with your GP/ENT | DVLA notification may be required if episodes are recurrent/unpredictable |
| Using sedating meds (e.g., prochlorperazine) | High-slowed reaction time | No driving until you feel fully alert and off sedating effects | None specific, but document advice in your records |
| Commercial driving (Group 2) | Very high standard | Stop driving with any disabling vertigo; seek specialist clearance | Expect stricter DVLA review; longer symptom-free period usually needed |
Mini‑FAQ
- Can I drive if I only have tinnitus? Yes, if attention and awareness aren’t affected. Keep the cabin quiet and check mirrors often. If tinnitus spikes make you anxious or distract you, delay the trip.
- What about hearing loss in one ear? Plenty of drivers manage fine. Adjust mirrors, reduce cabin noise, and pay extra attention at junctions. A hearing aid can help with situational awareness.
- Do blue‑light glasses help? If you’re light-sensitive, good sunglasses or a cap can help during the day. At night, avoid overly tinted lenses that cut visibility.
- Are motion sickness bands or ginger useful? Some people find wrist acupressure or ginger helpful for nausea. Harmless to try; don’t rely on them during a true spin.
- Is weather a trigger? Fast pressure drops can stir symptoms in some. If a storm is inbound and you’re borderline, postpone the drive.
- How do I document fitness to drive? Keep a simple symptom log; bring it to your GP/ENT. If the DVLA requests reports, your clinicians will send them.
- What if I’m a bus/lorry driver? Stop driving with any disabling vertigo. Talk to occupational health and your ENT. Expect a stricter return‑to‑work threshold and longer symptom‑free period.
- Can I get a Blue Badge? Not usually for Meniere’s alone, unless mobility is substantially and long‑term affected. Check your council’s criteria.
- Will my insurer raise premiums? Not always. Being proactive-disclosure, a treatment plan, and clinician letters-often helps.
Credible sources behind these tips: DVLA “Assessing fitness to drive” (vestibular disorders), NHS pages on Meniere’s, AAO-HNS 2020 clinical practice guideline, and research reviews such as Cochrane 2022 on betahistine.
Next steps and troubleshooting for different situations
If you were just diagnosed:
- Read your clinic’s written plan. Ask what to take during an attack-and how those meds affect driving.
- Set up a symptom diary: date, duration, triggers, meds taken, and recovery time.
- Tell your insurer you’ve been diagnosed. Keep the note polite and factual.
- Book a vestibular physio if offered. Early rehab pays off later.
- For two weeks, keep trips short and in daylight. Build confidence gradually.
If you’re having frequent attacks:
- Stop driving until you and your clinician agree control is back.
- Review treatment: salt intake, hydration, sleep, stress, and medication doses. Ask about preventive options or adjustments.
- Check for other triggers: new meds, migraines, caffeine changes, new screens or lighting at work.
- Consider a work/commute plan: flexible hours, ride-shares, or remote days. Put it in writing with your manager.
- If episodes are unpredictable and disabling, prepare to notify the DVLA (Group 1) and expect a longer pause if you’re Group 2.
If symptoms strike in the car park before you set off:
- Keys out, seat back, breathe, water. Take your rescue med if prescribed and safe.
- Text your contact that you’re delayed. If symptoms linger, lock up and take a ride home.
If you care for someone with Meniere’s:
- Agree a code word that means “I need to pull over now.”
- Keep their vertigo kit in the passenger door.
- Learn the emergency steps. Be calm and practical; your tone matters.
If you’re ready to return after a rough patch:
- Rehearse low-stress drives first: quiet streets, short loops, then build.
- Drive with a trusted passenger for the first few trips.
- Keep your diary. If you get through 4-6 weeks symptom-light, expand gradually.
Final thought: Driving with Meniere’s isn’t an all-or-nothing verdict. It’s a series of small, smart choices that add up to safe miles. When you choose not to drive, that’s not a failure-it’s expert risk management by the person who knows your body best: you.






Rushikesh Mhetre September 5, 2025
Hey folks, this guide hits the nail on the head – a quick pre‑drive check can save you a huge headache later! Grab a cup of water, rate your steadiness and if you’re below an eight, just park it. Stay safe out there 😊
Sharath Babu Srinivas September 5, 2025
Great summary, but a tiny tweak: use “rate your steadiness from 0‑10” instead of “Rate your steadiness from 0‑10”. The rest looks spot‑on! 👍👍
Halid A. September 5, 2025
I appreciate the thoroughness of the checklist. It provides a clear framework for clinicians to discuss fitness to drive with patients. Maintaining a symptom diary aligns well with evidence‑based practice, and the inclusion of emergency steps is commendable.
Brandon Burt September 5, 2025
Let's unpack the whole situation, because there’s a lot to consider, and it’s easy to miss a crucial point; first, the unpredictability of vertigo attacks fundamentally challenges any static risk assessment, and that means drivers need a dynamic, real‑time self‑evaluation before each journey. Second, the DVLA’s requirement for medical reporting is not merely bureaucratic red tape, it’s a safety net that protects other road users, and neglecting it can lead to legal and insurance repercussions. Third, medication side‑effects, especially drowsiness, can be insidious; even a mild sedative effect can impair reaction time, so a simple “feel alert?” question may be insufficient. Fourth, the pre‑drive checklist you described is solid, yet it could benefit from a weighted scoring system, for example assigning higher points to balance tests than to hydration status, because balance is the primary driver of safety. Fifth, environmental triggers such as glare or fog should be logged alongside personal factors; a pattern may emerge showing that certain weather conditions correlate with attacks. Sixth, technology aids like lane‑keep assist are great, but they are not a substitute for human vigilance, and over‑reliance can foster complacency. Seventh, the emergency pull‑over protocol is excellent, yet it could be expanded to include a quick phone‑call script to roadside assistance, because seconds count. Eighth, insurance companies often require disclosure, but many offer lower premiums for documented safety measures, which can be an incentive for drivers to stay proactive. Ninth, the suggestion to keep a “vertigo kit” is practical; adding a small flashlight and a portable charger ensures you’re not stranded without communication. Tenth, for commercial drivers, the symptom‑free period of roughly one year is not arbitrary; it reflects the higher risk profile of larger vehicles and the potential for greater harm. Eleventh, vestibular physiotherapy, though sometimes overlooked, yields measurable improvements in balance confidence, and should be part of the long‑term management plan. Twelfth, dietary modifications, particularly sodium reduction, have variable evidence, but they are low‑risk and worth trialing, especially if attacks cluster after salty meals. Thirteenth, mental health support is essential; anxiety can both trigger and exacerbate vertigo, creating a feedback loop that should be broken with counseling or CBT. Fourteenth, employers can play a role by allowing flexible start times, which reduces the pressure to drive in suboptimal conditions. Finally, the key takeaway is that driving with Meniere’s is a nuanced decision that blends medical guidance, personal self‑assessment, and practical adaptations, and embracing this holistic approach maximizes safety for everyone on the road.
Gloria Reyes Najera September 6, 2025
Honestly this stuff is just overblown, US drivers know how to handle any dizziness anyway and we dont need all this UK bureaucracy nonsense
Gauri Omar September 6, 2025
Listen, if you think you can just ignore the spinning and keep tearing down the motorway, you’re courting disaster! The world doesn’t stop for your dizziness, and every snap of a head could fling you into a nightmare. Get a plan, or get out of the driver’s seat before you end up wrecking everything!
Willy garcia September 6, 2025
Sounds solid stay safe and keep that diary handy
zaza oglu September 6, 2025
Wow!!! This checklist is a masterpiece!!! It not only empowers drivers but also paints a vivid roadmap to safety!!! Keep shining this beacon of practicality, and remember, every cautious mile is a victory!!! 🌟🚗
Vaibhav Sai September 6, 2025
I love how you broke down each step with such clarity-it feels like a friendly chat over coffee, yet packed with actionable tips. The pre‑drive rating system is especially handy; I’ll definitely start using the 0‑10 scale before my morning commute. Also, the suggestion to keep a “vertigo kit” in the passenger door is genius, because I always forget my meds otherwise. Thanks for the thorough guide!
Lindy Swanson September 6, 2025
Not gonna lie, I think people are getting way too worried about a little spin. Honestly, a quick stop for a breather usually does the trick, no need for all that paperwork.
Amit Kumar September 6, 2025
Great tips, thanks! 🚗👍
Crystal Heim September 6, 2025
While well‑intentioned, this guide overlooks the fact that many drivers simply cannot meet these strict standards.
Sruthi V Nair September 7, 2025
At the end of the day the road is a mirror of our inner balance; driving with Meniere’s invites us to reflect on control, acceptance, and the rhythm of our own body.