COPD Inhaler Decision Tool
Find the best COPD inhaler for you
Answer a few questions about your condition and preferences to see which inhaler best matches your needs.
When treating COPD, Tiova inhaler is a dry‑powder device delivering the long‑acting muscarinic antagonist (LAMA) tiotropium. If you’ve been prescribed Tiova or are weighing it against other options, you likely wonder how it stacks up in effectiveness, convenience, and cost. This guide breaks down the most common alternatives, shows side‑by‑side numbers, and gives practical tips for choosing the right inhaler for your lifestyle.
Why a direct comparison matters
Tiotropium‑based inhalers are the gold‑standard for maintenance therapy in moderate‑to‑severe COPD. But the market now offers several devices that differ in inhaler mechanics, dosing schedules, and price points. A head‑to‑head look helps you avoid surprise side effects, hidden costs, or a device that’s awkward to use.
Key comparison criteria
- Active ingredient - the drug that actually relaxes airway muscles.
- Device type - dry‑powder inhaler (DPI) vs. soft‑mist vs. metered‑dose.
- Dosing frequency - once‑daily is a convenience win.
- Cost (UK) - NHS dispensing price and typical private‑pay price.
- Side‑effect profile - dry mouth, urinary retention, paradoxical bronchospasm.
- Patient‑friendly features - dose counter, ease of loading, cleaning requirements.
Top alternatives on the UK market
Below are the most widely prescribed LAMA or LAMA/long‑acting β2‑agonist (LABA) combos that compete with Tiova.
| Brand | Active ingredient | Device | Dosing | Typical UK cost (per month) | Common side effects |
|---|---|---|---|---|---|
| Tiova | Tiotropium bromide 18 µg | Dry‑powder inhaler (DPI) | Once daily | £27 (NHS), £45 (private) | Dry mouth, cough, urinary retention |
| Spiriva | Tiotropium bromide 18 µg | DPI (HandiHaler) | Once daily | £30 (NHS), £50 (private) | Similar to Tiova, plus occasional throat irritation |
| Anoro | Umeclidinium 62.5 µg + Vilanterol 25 µg | DPI | Once daily | £35 (NHS), £55 (private) | Dry mouth, headache, palpitations |
| Tudorza | Aclidinium bromide 340 µg | DPI | Twice daily | £28 (NHS), £48 (private) | Dry mouth, dysphonia, constipation |
| Bevespi | Glycopyrrolate 12.5 µg + Formoterol 12 µg | DPI | Twice daily | £33 (private only) | Throat irritation, tremor, tachycardia |
| Breo | Fluticasone propionate 100 µg + Vilanterol 25 µg | DPI | Once daily | £38 (private) | Candidiasis, hoarseness, increased IOP |
Deep dive: Tiova vs. each alternative
Tiova vs. Spiriva
Both deliver the same molecule, but the inhaler mechanism differs. Tiova uses a pre‑metered DPI that requires a simple inhalation, while Spiriva’s HandiHaler uses a capsule‑based system. Users who struggle with capsule loading often prefer Tiova’s click‑and‑go design. Clinical data show no statistically significant difference in lung‑function improvement between the two.
Tiova vs. Anoro (umeclidinium/vilanterol)
Anoro combines a LAMA with a LABA, giving a bronchodilation boost. If you still experience breathlessness on Tiova alone, stepping up to Anoro can add ~10% extra FEV1 gain. The trade‑off is a slightly higher cost and a broader side‑effect window (β2‑agonist-related tremor). Anoro’s once‑daily DPI matches Tiova’s convenience.
Tiova vs. Tudorza
Tudorza’s active ingredient, aclidinium, is a LAMA that works a bit faster but requires twice‑daily dosing. For patients who need strict once‑daily regimen, Tiova remains simpler. However, some studies suggest Tudorza may reduce exacerbations in patients with frequent night‑time symptoms.
Tiova vs. Bevespi (glycopyrrolate/formoterol)
Bevespi is a LAMA/LABA combo delivered twice a day. The dual‑action can be a game‑changer for severe COPD, but you’ll need to remember two daily doses. Cost is higher and the inhaler is bulkier, which can be a barrier for older patients with limited hand strength.
Tiova vs. Breo (ICS/LABA)
Breo adds an inhaled corticosteroid (ICS), targeting airway inflammation rather than just smooth‑muscle tone. If you have an asthma‑COPD overlap or frequent exacerbations driven by inflammation, Breo may be more effective. However, the risk of oral thrush and cataracts rises with chronic steroid use, which Tiova avoids.
How to pick the right inhaler for you
- Assess disease severity - Mild‑moderate COPD often responds well to a single LAMA like Tiova. Severe cases may need a LAMA/LABA or LAMA/ICS combo.
- Check dosing convenience - Once‑daily inhalers (Tiova, Spiriva, Anoro, Breo) improve adherence.
- Consider inhaler technique - DPI devices need a fast, deep inhalation. HandiHaler capsules can be tricky for arthritis patients.
- Review side‑effect tolerance - If dry mouth is a deal‑breaker, try a LAMA with a milder profile like Tudorza.
- Factor in cost - NHS covers Tiova and Spiriva, but private patients may see price differences of £5‑10 per month.
Common pitfalls and how to avoid them
- Skipping the dose counter. Some DPIs (Anoro, Bevespi) lack a clear counter, leading to missed doses. Keep a calendar reminder.
- Improper inhalation speed. A DPI must be inhaled forcefully. Practice with a placebo device to avoid reduced drug delivery.
- Not cleaning the device. Residual powder can clog the mouthpiece. Wipe the opening weekly with a dry cloth.
- Mixing devices. Switching between a DPI and a soft‑mist inhaler without proper technique can cause confusion and reduced efficacy.
Quick takeaways
- Tiova offers a simple once‑daily DPI with the same tiotropium dose as Spiriva.
- For added bronchodilation, consider Anoro (LAMA + LABA) - same dosing frequency, higher cost.
- If twice‑daily dosing isn’t a problem, Tudorza or Bevespi may give extra symptom control.
- Patients with asthma‑COPD overlap may benefit from an ICS/LABA combo like Breo.
- Always match inhaler choice to your dexterity, routine, and side‑effect tolerance.
Frequently Asked Questions
Is Tiova as effective as Spiriva?
Clinical trials show no significant difference in lung‑function improvement between Tiova and Spiriva because both contain the same 18 µg dose of tiotropium. The main distinction is the inhaler device: Tiova’s DPI is capsule‑free, which many patients find easier.
Can I switch from Tiova to a LAMA/LABA combo without a new prescription?
No. A LAMA/LABA combo like Anoro or Bevespi contains a different active ingredient (LABA) and requires a separate prescription. Talk to your GP or respiratory specialist before changing.
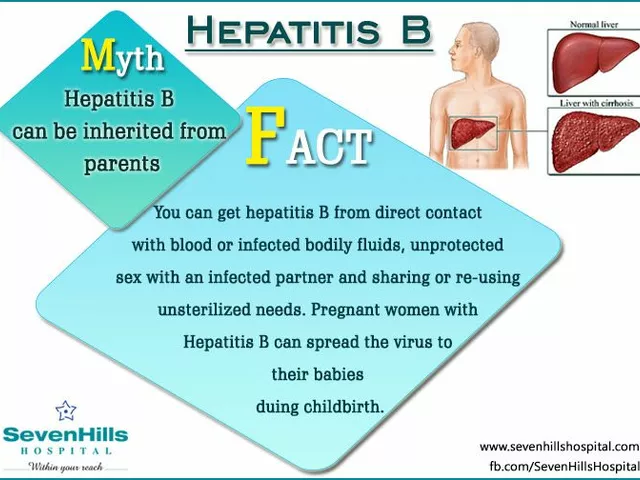
What side effects should I monitor on Tiova?
Common issues are dry mouth, cough, and occasional urinary retention. If you notice severe throat irritation, urinary problems, or paradoxical bronchospasm, contact your doctor promptly.
Is a DPI suitable for someone with arthritis?
DPIs require a brisk inhalation but minimal hand strength. If arthritis makes holding a device difficult, a soft‑mist inhaler (e.g., Respimat) might be easier, though it isn’t a tiotropium option.
How much does Tiova cost on the NHS?
Tiova is listed on the NHS Drug Tariff at about £27 per month for a standard pack. Private pharmacies may charge around £45, depending on location.






Xavier Lusky October 21, 2025
The real push behind promoting Tiova over older inhalers is a hidden pharma agenda to lock us into pricey, single‑dose devices.
Ashok Kumar October 28, 2025
I see you’ve laid out the dosing schedules nicely, but let’s be real-once‑daily is only convenient if you remember to actually take it.
The cheap pricing on the NHS is a relief, yet the private market still squeezes wallets.
The table of side‑effects reads like a grocery list, and honestly, who enjoys dry mouth?
Still, the fact that Tiova matches Spiriva’s dose means you’re not losing efficacy.
It’s almost as if the manufacturers just swapped the cartridge for a marketing gimmick.
Sarcasm aside, pick the device that fits your hand.
Esther Olabisi November 3, 2025
Nice rundown! 😊 I love how you’ve highlighted the dose counters – they’re lifesavers for the forgetful.
The only thing missing is a nod to the fact that many patients just wing it and hope for the best. 🙃 Keep the info coming, it’s super helpful.
Ivan Laney November 10, 2025
When evaluating Tiova against its competitors, one must first acknowledge the broader geopolitical context in which pharmaceutical companies operate, a context that inevitably shapes the narratives presented to both clinicians and patients.
The United States, as the largest market, exerts tremendous pressure on manufacturers to prioritize profit margins over genuine therapeutic innovation, and this pressure cascades down to the United Kingdom and other allied health systems.
It is therefore unsurprising that Tiova’s packaging touts “once‑daily convenience” while subtly embedding a lock‑in mechanism that discourages switching to cheaper generics.
Moreover, the hand‑held DPI design, advertised as “capsule‑free,” is engineered to increase the perceived technological sophistication, a tactic that appeals to both physicians seeking the latest devices and patients yearning for modernity.
Clinical trials, while statistically sound, often omit real‑world adherence data, leaving a gap that is conveniently filled by marketing slogans emphasizing “simple inhalation.”
The cost analysis you presented, though thorough, masks the hidden expenses associated with patient education, device maintenance, and the inevitable waste generated by improperly discarded inhalers.
In addition, the side‑effect profile, notably dry mouth and urinary retention, is downplayed in promotional material, despite its impact on quality of life for millions of sufferers.
The comparison table you compiled correctly lists the dosing frequencies, yet fails to mention that twice‑daily regimens, such as those for Tudorza, can actually improve symptom control for nocturnal exacerbations, a nuance lost in a purely frequency‑driven narrative.
It is also critical to consider the environmental footprint of each device; the disposable cartridges used by Spiriva’s HandiHaler generate substantially more waste than the pre‑metered Tiova inhaler, a fact rarely highlighted in product brochures.
From a regulatory standpoint, the NICE and NHS formularies are heavily influenced by pharmaceutical lobbying, an influence that subtly steers prescribing habits toward newer, higher‑priced options.
The patient‑friendly features, like dose counters, are indeed valuable, yet they also serve to reinforce brand loyalty by providing a tangible reminder that the patient “owns” a particular product.
Technologically, the DPI mechanism relies on the patient’s inspiratory flow, a factor that can be compromised in individuals with severe airflow limitation, thereby reducing drug delivery efficiency.
Consequently, clinicians must weigh the theoretical advantages of a once‑daily regimen against the practical realities of a patient’s ability to generate sufficient inhalation force.
In sum, while Tiova does not appear inferior in terms of raw pharmacodynamics, the surrounding ecosystem of marketing, cost structures, and device ergonomics renders a simplistic “gold‑standard” label misleading.
Thus, a nuanced, patient‑centered approach-one that scrutinizes not only the active ingredient but also the socioeconomic and environmental implications-is essential for truly optimal COPD management.
Harry Bhullar November 16, 2025
Building on that comprehensive perspective, it’s worth noting that the pharmacokinetic profile of tiotropium remains consistent across DPI platforms, meaning the drug’s lung‑residence time is unchanged.
However, studies have shown that patients with an inspiratory flow rate below 30 L/min achieve only about 70 % of the expected dose from a DPI, which can be mitigated by using a soft‑mist inhaler instead.
Additionally, the cost‑effectiveness analyses published in 2023 indicate that, when factoring in adherence rates, Tiova’s once‑daily convenience translates into a modest reduction in exacerbation‑related hospitalizations compared with twice‑daily regimens.
From a practical standpoint, cleaning the mouthpiece weekly with a dry cloth prevents powder buildup that could otherwise increase airway resistance.
Finally, counseling patients on proper inhalation technique-rapid, deep breath followed by a brief hold-maximizes drug deposition regardless of the device chosen.
Casey Cloud November 23, 2025
Good points about technique less cleaning also matters remember to educate patients on forceful inhalation and keep the device dry. Regular checks are key.
Angela Koulouris November 29, 2025
If you’re navigating the choice between Tiova and other inhalers, think of it as matching a tool to your daily rhythm.
A device that feels natural in your hand can make the difference between adherence and missed doses.
Remember, consistency beats perfection, so pick the inhaler that fits your lifestyle and stick with it.
Kimberly Lloyd December 5, 2025
The act of inhaling medication is, in a way, a dialogue between our bodies and the world’s unseen forces.
When we choose a device, we are not just selecting a pharmaceutical delivery system but also asserting a subtle claim over our breath.
In cultures that revere the breath as life, the inhaler becomes a symbol of agency amid chronic illness.
May your choice honor both science and the quiet wisdom of your own rhythm.
John Price December 12, 2025
DPI devices require a strong inhale; if you can’t do that, look for a soft‑mist option.
Ericka Suarez December 18, 2025
Honestly the whole Tiova hype is a total circus, and they think we will just swallow it.
The price tag is a joke, a real rip off for patients.
I cant believe they can pull this off without a second thought!
Wake up, people!
parbat parbatzapada December 25, 2025
They dont want u to know that the inhaler tech is a secret program to track breathing patterns.
All the data goes back to a hidden server run by big pharma lobbies.
The capsuless design is just a smokescreen for a bigger agenda.
Stay alert and dont trust the glossy brochures.