When someone stops drinking after years of heavy alcohol use, their body doesn’t just feel shaky or anxious-it’s going through a major internal overhaul. The liver, which has been working overtime to process alcohol, suddenly has to shift from damage control to repair mode. But this transition isn’t simple. In fact, the very act of quitting can put extra stress on an already strained liver. Many people think stopping alcohol is the end of the problem. It’s not. It’s the beginning of a critical phase where the right support can mean the difference between recovery and further harm.
What Happens to Your Liver When You Quit Drinking?
Your liver breaks down about 90% of the alcohol you consume. It turns ethanol into acetaldehyde, a toxic byproduct, then into acetate, which your body can use for energy. But when you drink heavily over time, this system gets overwhelmed. Fat builds up, inflammation sets in, and scar tissue starts replacing healthy cells. This is called alcohol-related liver disease, and it includes fatty liver, alcoholic hepatitis, and cirrhosis.
When you stop drinking, your liver doesn’t magically heal overnight. In the first 24 to 72 hours, your body goes into withdrawal. Blood flow to the liver changes. Metabolism shifts. And here’s the catch: even though you’re no longer consuming alcohol, your liver can actually experience more stress during this time. A 2002 study found that liver enzymes like AST and ALT often spike in the first week after quitting-not because of new damage from alcohol, but because the liver is struggling to adapt.
That’s why simply saying “I’m done” isn’t enough. You need a plan that protects your liver while your body adjusts.
Why Medical Supervision Isn’t Optional
Trying to quit alcohol alone, especially after long-term heavy use, can be dangerous. About 5% of people with severe alcohol withdrawal develop delirium tremens-a life-threatening condition with confusion, seizures, and rapid heartbeat. Without medical help, the risk of death rises sharply.
But it’s not just about avoiding seizures. Your liver needs protection too. Medically supervised detox reduces complications by 30% compared to home attempts, according to a 2022 meta-analysis. In a hospital or clinic, doctors can monitor your liver enzymes, blood pressure, and hydration levels. They can give you the right medications at the right time.
Benzodiazepines like chlordiazepoxide are the gold standard for managing withdrawal symptoms. They calm the nervous system and prevent seizures. One study showed they’re 85% effective at stopping seizures, compared to just 40% with symptom-triggered approaches alone. But it’s not just about drugs. Medical teams also check for signs of advanced liver disease-like low albumin levels (below 3.5 g/dL) or a prolonged INR (above 1.5)-which signal you’re at risk of liver failure.
If you’re not in a clinic, you’re not getting this level of oversight. And that’s risky.
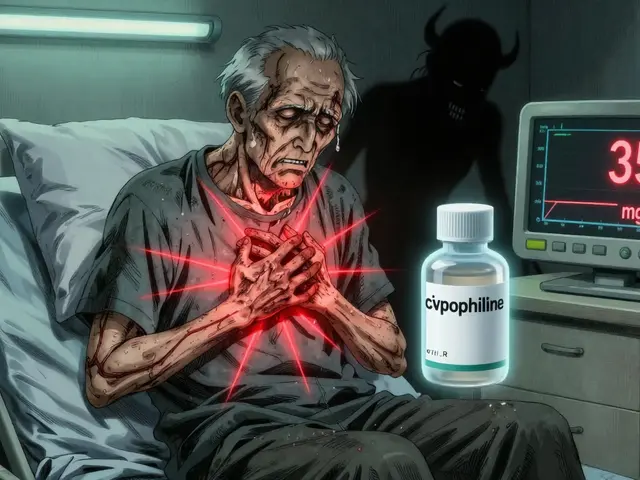
The Hidden Danger: Paracetamol and Other Toxins
One of the most overlooked dangers during alcohol withdrawal is taking common painkillers like paracetamol (acetaminophen). Even a small dose-just 1 to 2 grams a day-can cause a massive spike in liver enzymes in someone recovering from alcohol dependence. Why? Because your liver’s detox pathways are still scrambled. It can’t process the drug properly, and toxic byproducts build up.
A 2002 study documented a case where a person taking only 1.5 grams of paracetamol daily during withdrawal had the highest liver enzyme rise of anyone in the group. That’s not an outlier. It’s a pattern. The liver is more vulnerable during withdrawal than at any other time-even more than when you’re actively drinking.
That means no Tylenol. No cold meds with hidden paracetamol. No over-the-counter pain relievers unless your doctor says it’s safe. Even herbal supplements like kava or comfrey can be harmful. Stick to what your medical team approves.
Nutrition: The Secret Weapon for Liver Recovery
Your liver needs fuel to repair itself. But heavy drinkers are often malnourished. Alcohol blocks nutrient absorption. It depletes vitamins, especially thiamine (B1), which is critical for brain and liver function.
Without thiamine, you risk Wernicke-Korsakoff syndrome-a severe brain disorder that can cause memory loss, confusion, and even permanent damage. That’s why hospitals give 500mg of IV thiamine daily for 3 to 5 days during detox. Oral supplements won’t cut it if you’re severely deficient.
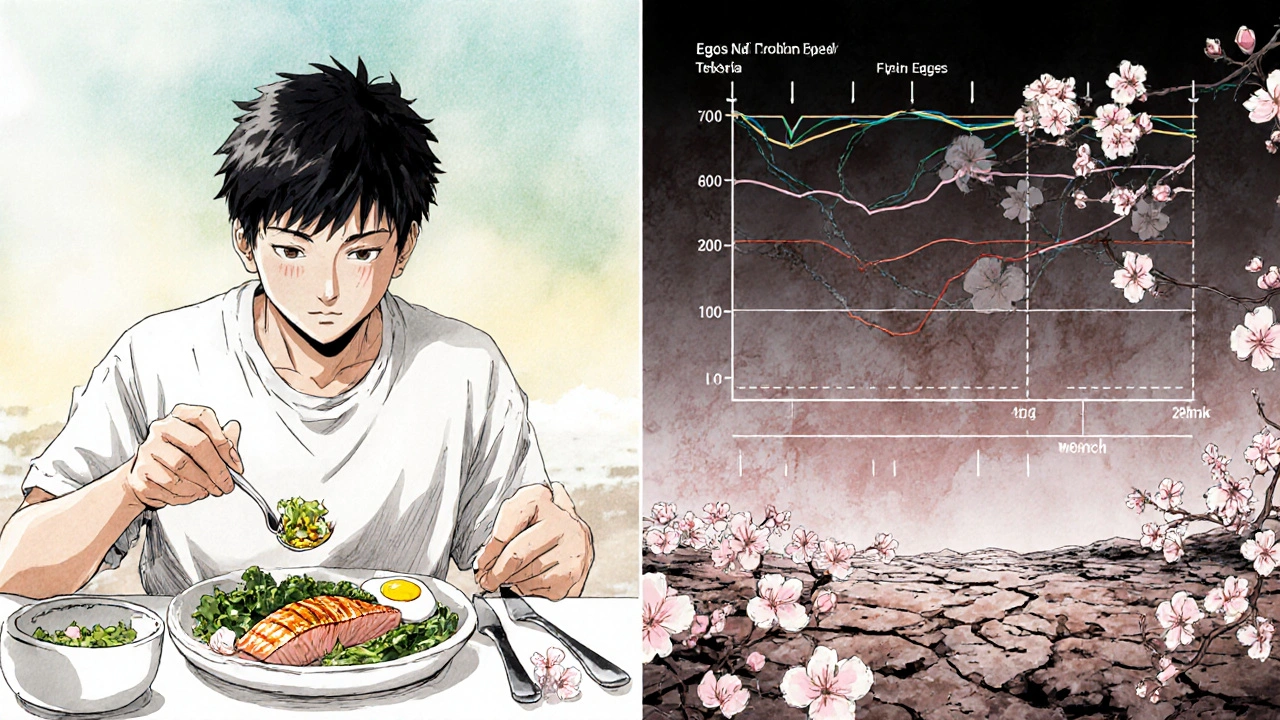
Protein is just as important. Your liver needs amino acids to rebuild tissue. Experts recommend 1.2 to 1.5 grams of protein per kilogram of body weight each day. For a 70kg person, that’s 84 to 105 grams daily. Eggs, lean meats, fish, beans, and dairy are good sources. A high-protein diet can speed up liver enzyme normalization by 40%, according to NHS guidelines.
Also, don’t forget zinc, magnesium, and B vitamins. These help reduce inflammation and support detox pathways. A simple multivitamin won’t cut it. You need targeted, medical-grade supplementation during this phase.
How Long Does It Take for the Liver to Heal?
It depends on how damaged your liver was before you quit.
If you have fatty liver-early-stage alcohol-related liver disease-your liver can start to repair itself within weeks. Liver enzymes often begin normalizing between 7 and 14 days after quitting. After 6 weeks of abstinence, many people see significant improvement, sometimes even full recovery.
But if you have alcoholic hepatitis or cirrhosis, it’s a different story. Alcoholic hepatitis can reverse if caught early and you stop drinking completely. But if you keep drinking, it will progress to cirrhosis-and that’s permanent scarring. Once cirrhosis sets in, the liver can’t fully heal, but it can stabilize. Stopping alcohol at this stage can still add years to your life.
Research published in Scientific Reports (2021) found that even after years of heavy drinking, the liver can show major regeneration within 3 to 12 months of total abstinence. That’s not magic. It’s biology. The liver is the only organ that can regrow its own tissue. But it needs time, no toxins, and proper nutrition.
Don’t rush it. Don’t test yourself with “just one drink.” One drink can undo months of progress.
What Not to Do During Detox
Here are the biggest mistakes people make:
- Trying to detox alone at home-especially if you’ve been drinking heavily for years
- Taking paracetamol or other OTC painkillers without medical approval
- Skipping thiamine or protein-rich meals
- Believing that “I stopped, so I’m fine” and skipping follow-up care
- Using herbal detox teas or “liver cleanses”-they’re not proven and can be toxic
Also, don’t underestimate the emotional side. Withdrawal can last weeks. Anxiety, insomnia, and cravings don’t vanish after the first few days. That’s why ongoing support-therapy, counseling, support groups-is just as important as medical care.
Long-Term Success: Beyond the First Week
Detox is just step one. The real challenge is staying sober. Studies show 70% of people who complete detox but don’t get ongoing support relapse within six months. And every relapse sets back liver recovery.
Recovery isn’t a sprint. It’s a lifestyle change. That means:
- Regular liver function tests every 3 to 6 months
- Sticking to NHS guidelines: no more than 14 units of alcohol per week (and even that’s not recommended if you’ve had liver damage)
- Building a support network-whether it’s Alcoholics Anonymous, a therapist, or a recovery coach
- Monitoring for signs of relapse: mood swings, isolation, skipping meals, returning to old habits
For those with cirrhosis, lifelong abstinence is non-negotiable. For others, even a single drink can restart the cycle of inflammation and scarring.
What’s New in Liver Recovery Science
Researchers are now looking beyond just stopping alcohol. They’re studying how to actively help the liver heal faster.
Biomarkers like TIMP1 and PIIINP are being used to track fibrosis-the buildup of scar tissue-during withdrawal. Even after someone stops drinking, these markers can stay high, meaning the liver is still trying to repair itself. New drugs targeting these pathways are in early trials.
Telemedicine is helping people in rural areas access detox support. Real-time liver enzyme monitoring in clinics has cut severe complications by 35%. And scientists are exploring personalized medicine-using genetic tests to tailor benzodiazepine doses, reducing liver strain.
But none of this replaces the basics: medical supervision, no toxins, good nutrition, and long-term commitment.
Final Thoughts: Your Liver Can Heal-If You Let It
Quitting alcohol is one of the most powerful things you can do for your liver. But quitting alone isn’t enough. You need a smart, safe, supported plan. The liver is resilient. It can regenerate. But it needs time, care, and protection.
If you’re thinking about quitting, don’t wait until you’re in crisis. Talk to a doctor. Get tested. Start with a plan. Your liver has been working for you for years. Now it’s time to give it the chance to heal.
Can I detox from alcohol at home safely?
For mild cases-like someone who drinks moderately and has no liver damage-home detox with support might be possible. But for anyone who’s been drinking heavily for months or years, home detox is dangerous. Withdrawal can cause seizures, delirium tremens, or sudden liver stress. Medical supervision reduces complications by 30% and is strongly recommended for anyone with a history of heavy drinking or liver issues.
How long until liver enzymes return to normal after quitting alcohol?
In people with mild to moderate alcohol-related liver damage, liver enzymes like AST and ALT usually begin to drop within 7 to 14 days after quitting. Normalization can take 4 to 8 weeks. If enzymes stay high beyond that, it may indicate more advanced disease like alcoholic hepatitis or early cirrhosis, which requires further testing and long-term management.
Is it safe to take paracetamol after quitting alcohol?
No, it’s not safe during early withdrawal. Even small doses of paracetamol (acetaminophen) can cause serious liver injury in people recovering from alcohol dependence. The liver’s ability to process toxins is impaired for weeks after stopping drinking. Avoid all OTC painkillers unless your doctor approves them. Use non-medication methods like rest, hydration, and heat packs for pain relief.
Can the liver recover from cirrhosis after quitting alcohol?
Cirrhosis means permanent scarring. The liver can’t fully reverse it. But stopping alcohol completely can stop further damage and allow the liver to stabilize. Many people with cirrhosis live for years without progression if they stay sober, eat well, avoid toxins, and get regular medical care. The goal shifts from healing to preventing complications like liver failure or cancer.
What vitamins are most important for liver recovery after alcohol use?
Thiamine (B1) is critical-deficiency can cause brain damage. Doctors typically give 500mg IV daily for 3-5 days. After that, oral B-complex vitamins help. Vitamin D, zinc, magnesium, and antioxidants like N-acetylcysteine (NAC) also support liver repair. A high-protein diet with lean meats, eggs, beans, and dairy provides the amino acids your liver needs to rebuild.
How soon can I start drinking again after detox?
If you’ve had any form of alcohol-related liver disease-including fatty liver-do not resume drinking. Even moderate drinking can restart inflammation and scarring. For those with mild disease and no liver damage, some guidelines suggest 6 weeks of abstinence may allow cautious return to low-risk drinking (14 units per week max). But this is rare. Most doctors recommend lifelong abstinence after any alcohol-related liver injury. The safest choice is no alcohol at all.
Do alcohol detox teas or supplements really help the liver?
No. Products marketed as “liver cleanses” or “alcohol detox teas” have no scientific backing. Some contain herbs like kava, comfrey, or green tea extract that can actually damage the liver. Your liver doesn’t need a “cleanse.” It needs rest, nutrition, and no toxins. Stick to evidence-based care: medical supervision, proper nutrition, thiamine, and abstinence.





james lucas November 23, 2025
man i never realized how much my liver was screaming until i quit. i thought i was just feeling hangover city for a week, but turns out my body was doing full-on surgery on itself. i took tylenol for a headache day 3 and felt like i was gonna die. not even kidding. my doctor flipped out when i told him. now i just drink water, eat eggs like they’re going out of style, and nap like it’s my job. the cravings are wild, but the liver feels better already. 3 weeks in and my skin isn’t yellow anymore. who knew giving up beer was basically giving your liver a spa day?
Jessica Correa November 24, 2025
i’m so glad someone finally said the paracetamol thing because i almost took some last week for my back pain and then i remembered reading something about it and just stopped myself. i didn’t even know it was that dangerous. i’ve been drinking for 12 years and thought quitting was the hard part. turns out the real danger is all the stuff you think is harmless. thank you for writing this. i’m going to get my thiamine levels checked tomorrow. i feel like i’ve been running on fumes for years
manish chaturvedi November 25, 2025
as someone from india where alcohol abuse is often stigmatized and rarely discussed openly, i find this post deeply valuable. many of my friends who quit drinking do so in isolation, without medical support, believing that willpower alone is enough. the liver’s ability to regenerate is a miracle of biology, but it requires respect, not just intention. in our culture, we often overlook nutrition and supplementation during recovery, focusing only on abstinence. this article correctly highlights that protein, thiamine, and avoiding toxins are not optional-they are the foundation of healing. i will share this with my community.
Nikhil Chaurasia November 25, 2025
you know what’s sad? people think detox is over when they stop shaking. but your liver? it’s still screaming in the dark. i watched my brother try to quit at home. he lasted 10 days. then he took ibuprofen for a headache, got nauseous, went to the ER, and they found his liver enzymes were through the roof. he’s lucky he didn’t die. now he’s in rehab, and i’m scared to even drink soda around him. this isn’t just about willpower. it’s about survival. please, if you’re reading this and you’re thinking about quitting-don’t be brave. be smart. call a doctor.
Michael Fitzpatrick November 27, 2025
i’ve been sober 11 months now and honestly the biggest surprise was how much better i slept after the first month. not just more sleep-deeper sleep. like my brain finally stopped screaming. i used to think i needed wine to unwind. turns out my liver was the one doing all the unwinding, and it was exhausted. i started eating more eggs, taking B-complex, and avoiding anything that says ‘pain relief’ on the label. i even started walking every morning just to feel alive again. it’s not glamorous. no detox tea, no juice cleanse. just food, rest, and time. and yeah, i still have days where i miss the taste of beer. but i don’t miss the hangover that lasted a week. this is better.
Shawn Daughhetee November 27, 2025
my cousin died last year from liver failure after quitting cold turkey at home. he thought he was fine after a week. he wasn’t. no one told him about the paracetamol thing or the thiamine. he took Advil for his headaches and just… stopped breathing in his sleep. i wish i’d known what i know now. if you’re thinking of quitting, please don’t do it alone. talk to someone. call a clinic. your liver doesn’t care how strong you are. it just needs care. rest in peace, danny.
Miruna Alexandru November 29, 2025
the notion that the liver ‘heals’ is dangerously oversimplified. regeneration is not restoration. fibrosis is not reversible in the clinical sense-it is merely stabilized. the liver does not ‘bounce back’; it adapts to trauma by scar formation. to call this healing is to romanticize pathology. the real victory is not regeneration-it is prevention of further damage. and yet, we still see people post on social media about their ‘liver detox’ after 30 days. this is not healing. this is delusion dressed as hope. the science is clear: cirrhosis is a life sentence. abstinence is not a cure. it’s damage control. stop selling fairy tales.
Melvina Zelee November 29, 2025
my mom quit drinking after 25 years and i watched her turn into someone i barely recognized in the best way. she started cooking again. she remembered my birthday. she laughed without sounding like she was forcing it. the thiamine thing? yeah she got IVs for 5 days. i thought that was extreme until i saw her eyes stop looking so foggy. now she eats salmon every sunday and takes her vitamins like they’re holy water. i used to think sobriety was about giving something up. now i know it’s about getting something back. your liver doesn’t need a cleanse. it needs you to show up. not perfectly. just consistently. and honestly? that’s the hardest part.
steve o'connor December 1, 2025
just one sentence: don’t be the guy who reads this and says ‘i’ll be fine’-you won’t be.