When a child’s vision doesn’t develop properly, it’s not just about seeing blurry. It’s about the brain learning to ignore one eye - a silent, invisible problem called amblyopia. Often called "lazy eye," it’s the most common cause of vision loss in kids, affecting 2% to 4% of children. And here’s the hard truth: if it’s not caught early, that lost vision might never fully come back.
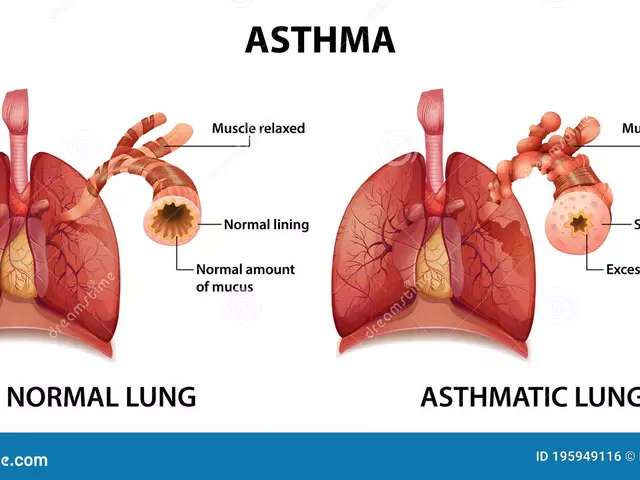
What Exactly Is Amblyopia?
Amblyopia isn’t a problem with the eye itself. The eye might look perfectly normal. The issue is in the brain. During the first few years of life, the brain learns how to process what the eyes see. If one eye sends a blurry, misaligned, or blocked image - because of a cataract, a turned eye, or a big difference in glasses prescription - the brain starts to ignore it. Over time, that eye becomes weaker, not because of damage, but because it’s unused. There are three main types:- Strabismic amblyopia - when one eye turns in, out, up, or down. The brain shuts off the misaligned eye to avoid double vision. This is the most common type, making up about half of all cases.
- Anisometropic amblyopia - when one eye has a much stronger prescription than the other. The brain prefers the clearer image and ignores the blurry one. This often goes unnoticed because the child can still see fine with the good eye.
- Deprivation amblyopia - when something physically blocks light from entering the eye, like a congenital cataract or droopy eyelid. This is the most serious form and needs urgent treatment.
Bilateral amblyopia - where both eyes are affected - happens when both eyes have high uncorrected prescriptions. Kids with this type often don’t realize they’re seeing poorly because everything is blurry.
Why Early Detection Is Non-Negotiable
The window for fixing amblyopia is narrow. The brain’s ability to rewire itself - called neuroplasticity - is strongest before age 5. After age 7, it gets harder. After 8, improvements become much slower and less complete. Studies show that kids treated before age 5 have an 85-90% chance of recovering near-normal vision. Those treated between 5 and 7 see about 50-60% improvement. After age 8, gains are often minimal. That’s why the American Academy of Pediatrics recommends a full eye exam by age 3. Many parents think, "My child can see the TV fine," or "They don’t squint or rub their eyes." But amblyopia often has no obvious signs. A child might cover one eye to see better, tilt their head, or have trouble with depth perception - like catching a ball or climbing stairs. A simple vision screening at school or the pediatrician’s office isn’t enough. A comprehensive exam by a pediatric ophthalmologist or optometrist is needed. That means checking visual acuity, refraction (glasses prescription), eye alignment, and the back of the eye to rule out cataracts or other structural issues.Patching Therapy: The Gold Standard
The most proven, time-tested treatment for amblyopia is patching. Cover the stronger eye with a patch, and the brain is forced to use the weaker one. It’s simple, cheap, and backed by decades of research. The old rule was to patch for 6 hours a day. But the landmark Amblyopia Treatment Study (ATS) changed that. Researchers found that for moderate amblyopia (vision between 20/40 and 20/100), just 2 hours of patching daily gave the same results as 6 hours. That’s a huge win for families. For severe cases (vision worse than 20/100), 6 hours is still recommended. For mild cases (20/25 to 20/40), 2 hours is often enough. The exact time depends on the child’s age, severity, and how well they respond.
What If My Child Won’t Wear the Patch?
This is the biggest hurdle. Studies show only 40-60% of kids stick with patching as prescribed. Parents report tears, tantrums, social teasing, and skin irritation from adhesive patches. Here’s what actually works in real life:- Start slow - Begin with 30 minutes a day and build up. Don’t throw them into 6 hours on day one.
- Make it fun - Turn patching into a game. "Superhero time!" Let them pick fun patch designs. Reward them with stickers or extra story time after patching.
- Use it during focused activities - Put the patch on during coloring, puzzles, tablet games, or reading. The more the eye is used for detail work, the better it strengthens.
- Use digital tools - Apps like "LazyEye Tracker" let parents log hours and get reminders. Some clinics report 22% of families now use them.
- Involve the school - Talk to teachers. Most kids are fine once peers understand it’s not a punishment - it’s their vision therapy.
Parental education makes a huge difference. Clinics that spend 20-30 minutes explaining how the brain rewires itself see 89% adherence. Those that just hand out a patch and say "wear it for 4 hours" get only 45% compliance.
Alternatives to Patching
Not every child tolerates a patch. There are other options:- Atropine drops - One drop of atropine in the stronger eye once a day blurs near vision, making the brain rely on the weaker eye. Studies show it works just as well as patching for moderate amblyopia. It’s great for kids who hate patches, though it can cause light sensitivity.
- Bangerter filters - These are translucent stickers you stick on the lens of glasses over the stronger eye. They’re less noticeable than a patch and work well for older kids who are self-conscious.
- Digital vision therapy - Platforms like AmblyoPlay use video games designed to stimulate the weaker eye. A 2023 study found 75% compliance with these apps - far higher than patching. They’re FDA-cleared and used widely in Europe and the U.S.
For kids with strabismus (eye turn), surgery to straighten the eye might be needed first. But even after surgery, patching or drops are still required to train the brain to use the eye properly.
How Long Does Treatment Take?
This isn’t a quick fix. Most children need treatment for 6 to 12 months. Some need it longer. Follow-ups every 4 to 8 weeks are critical. Vision improves in stages - sometimes slowly, sometimes with sudden jumps. The goal isn’t just better eyesight. It’s binocular vision - the ability for both eyes to work together. That’s what gives us depth perception. Without it, kids struggle with sports, driving later in life, or even reading for long periods. Vision therapy - specific exercises for eye tracking, focusing, and coordination - can boost results. When added to patching, studies show a 15-20% improvement in depth vision compared to patching alone.
What About Older Kids and Adults?
For years, doctors thought amblyopia couldn’t be treated after childhood. That’s changing. New research shows adults with amblyopia can improve vision with intensive perceptual learning - like playing specially designed video games for hours a day over months. But the gains are modest. A 30-year-old might go from 20/100 to 20/60. Not perfect, but better. The real takeaway? Don’t wait. The brain’s ability to adapt drops sharply after age 8. The earlier you act, the more likely your child will see clearly - and permanently.What Happens If You Don’t Treat It?
Untreated amblyopia doesn’t get better on its own. The weaker eye stays weak. If the good eye gets injured or develops disease later in life - say, diabetes or an accident - the child is left with permanent, irreversible vision loss in both eyes. That’s why screening isn’t optional. It’s essential.Even in places with great healthcare, many kids slip through the cracks. A 2022 study found that nearly 40% of children with amblyopia weren’t diagnosed until after age 5 - too late for full recovery.
Final Thoughts
Amblyopia isn’t rare. It’s common, treatable, and often invisible. Patching therapy isn’t glamorous, but it’s the most effective tool we have. The science is clear: early detection, consistent treatment, and parental support make all the difference. Your child doesn’t need to wear a patch forever. But if they wear it now - even for just a few hours a day - they might never have to live with one eye seeing poorly for the rest of their life.Can amblyopia fix itself without treatment?
No. Amblyopia won’t fix itself. The brain continues to ignore the weaker eye, and vision doesn’t improve on its own. Without treatment, the vision loss becomes permanent, especially after age 8.
How long should a child wear a patch each day?
It depends on severity. For moderate amblyopia (vision between 20/40 and 20/100), 2 hours a day is just as effective as 6 hours, according to major clinical trials. For severe cases, 6 hours is still recommended. The doctor will tailor the schedule based on age and response.
Is atropine eye drops as good as patching?
Yes, for moderate amblyopia. Daily atropine drops blur the stronger eye, forcing the brain to use the weaker one. Studies show 79% of children using atropine reach 20/30 vision or better within 6 months - matching patching results. It’s a good alternative for kids who resist patches.
Can a child outgrow amblyopia?
No. Amblyopia doesn’t go away with age. If untreated, it leads to lifelong vision loss in the affected eye. Even if the child seems to see fine, they’re likely relying only on their stronger eye. Without treatment, the weaker eye will never develop normal vision.
How do I know if my child has amblyopia?
Signs include squinting, tilting the head, closing one eye to see better, poor depth perception, or difficulty with tasks like catching a ball. But many children show no obvious symptoms. The only sure way is a comprehensive eye exam by a pediatric eye specialist before age 3.
Are digital vision games effective for amblyopia?
Yes. FDA-cleared platforms like AmblyoPlay use gamified exercises to stimulate the weaker eye. Real-world data shows 75% compliance - far higher than traditional patching. They’re especially helpful for older children who find patches uncomfortable or embarrassing.
Can adults be treated for amblyopia?
Adults can see modest improvements with intensive vision training, like daily perceptual learning tasks or specialized video games. But results are limited - usually a 10-30% improvement in vision. Treatment is far less effective than in children, which is why early screening is so critical.
How often should follow-up visits happen during treatment?
Follow-ups every 4 to 8 weeks are standard. The doctor checks visual acuity, adjusts patching time, and monitors for side effects. Progress isn’t always linear - some kids improve slowly, others have sudden jumps. Regular check-ins ensure treatment stays on track.
What if my child develops a rash from the patch?
Skin irritation is common. Try hypoallergenic patches, change the placement daily, or use a cloth patch held with tape. If irritation persists, talk to your doctor - atropine drops or Bangerter filters may be better options.
Is surgery ever needed for amblyopia?
Surgery isn’t used to treat amblyopia directly. But if the cause is a turned eye (strabismus), surgery to straighten the eye may be needed first. After surgery, patching or drops are still required to train the brain to use the eye properly. Surgery fixes alignment; therapy fixes vision.






Phil Maxwell January 23, 2026
My nephew got patched for 6 months when he was 4. At first, he cried like his soul was being ripped out. Now he’s 10, plays baseball like a pro, and doesn’t even remember wearing it. Weird how something so simple changes your whole life.
Parents, don’t give up. It’s hell for a few weeks, but it’s worth it.
Dolores Rider January 23, 2026
Okay but have you ever wondered if the government is using amblyopia patches to control kids’ brain development? I mean, why only ONE eye? What if they’re syncing it with school WiFi signals? I saw a guy on TikTok who said the patches have microchips embedded in the adhesive. 😳
venkatesh karumanchi January 24, 2026
As a dad from India, I thought my son’s squinting was just him being dramatic. Took us 2 years to get a proper checkup. When the doctor said ‘amblyopia’, I felt like I failed him. But patching? We made it a daily ritual with cartoon stickers. Now he sees everything clearly. Thank you for this post - it gave me hope.
Never underestimate a 2-hour patch. It’s not punishment. It’s love in disguise.
Kat Peterson January 25, 2026
Ugh. Patching? So 2010. 😒 I mean, really? We have AI-powered vision games now. Why are we still forcing toddlers to wear sticky bandages like they’re pirates? It’s so… low-tech. My daughter uses AmblyoPlay for 20 mins a day and she thinks it’s Fortnite. The brain doesn’t need coercion - it needs engagement. 🙄
blackbelt security January 26, 2026
My kid wore a patch for 8 months. We used a timer. We had a reward chart. We celebrated every week like it was a holiday. You want results? You show up. You don’t quit because your kid whines. This isn’t a suggestion - it’s a mission.
Be the parent who doesn’t let the system fail their child.
Patrick Gornik January 26, 2026
Let’s deconstruct the neuroplasticity paradigm. The brain doesn’t ‘ignore’ the eye - it optimizes resource allocation under sensory asymmetry. Patching is a crude intervention, a brute-force retraining of cortical dominance hierarchies. But here’s the real epistemological rupture: if the brain adapts by suppressing input, then perhaps the problem isn’t the eye… it’s the *cultural expectation* of binocular normativity. We pathologize difference. We pathologize asymmetry. We pathologize the child’s neural autonomy. What if the ‘lazy’ eye isn’t lazy at all - but the *brain’s* way of saying, ‘I’m not buying this binary’?
Atropine is just pharmacological coercion. Digital games? Algorithmic behavioral conditioning. We’re not healing vision - we’re enforcing visual conformity. And yet… I still patched my kid. Because I’m complicit too.
Tommy Sandri January 28, 2026
Thank you for the comprehensive and clinically accurate overview. The data on early intervention windows and adherence rates is particularly valuable. In many low-resource settings, access to pediatric ophthalmology remains limited. This information should be disseminated through primary care networks and community health programs to prevent irreversible vision loss in underserved populations.
Luke Davidson January 29, 2026
I never knew amblyopia could be this invisible. My daughter never squinted, never complained - she just didn’t catch balls well. We thought she was clumsy. Turns out her brain was choosing to see with one eye and ignoring the other. We started patching at 4.5, and after 3 months, she started reading signs on the highway. Like, full sentences. I cried in the car.
And yeah - the patches itch. The tantrums are real. But when she told me last week, ‘Daddy, I can see the stars with both eyes now’ - that’s the kind of moment that makes you want to hug the whole medical system.
Don’t wait. Don’t assume. Get the exam. Even if they seem fine.
Also - AmblyoPlay is legit. We used it with the patch. Made it feel like a game. My 5-year-old asked to play it on weekends. Who knew vision therapy could be fun?
Karen Conlin January 30, 2026
As a pediatric nurse, I’ve seen hundreds of kids go through this. The ones who get it early? They thrive. The ones who don’t? They struggle in school, in sports, in life. Patching isn’t cute. It’s not glamorous. But it’s the single most effective thing we’ve got.
And to the parents who say ‘my kid won’t wear it’ - I get it. I’ve held sobbing toddlers while their moms cried too. But here’s what works: make it a ritual. 20 minutes after breakfast. Same time. Same place. No negotiating. Then reward with something they love - not candy. A walk. A song. A hug.
And if your kid hates the patch? Try atropine. Try the filters. But don’t give up. Their future vision is worth every tear.
Also - yes, adults can improve. But it’s harder. So don’t wait. Not one more day.