Chronic eczema isn’t just dry skin. It’s a broken barrier, a misfired immune system, and a relentless itch that steals sleep, confidence, and quality of life. If you’ve been dealing with this for months or years, you know the cycle: scratch → flare → moisturize → scratch again. But what if the real problem isn’t the itch itself, but what’s happening beneath the surface? The truth is, chronic eczema starts with a damaged skin barrier - and fixing that changes everything.
Why Your Skin Barrier Is the Root Cause
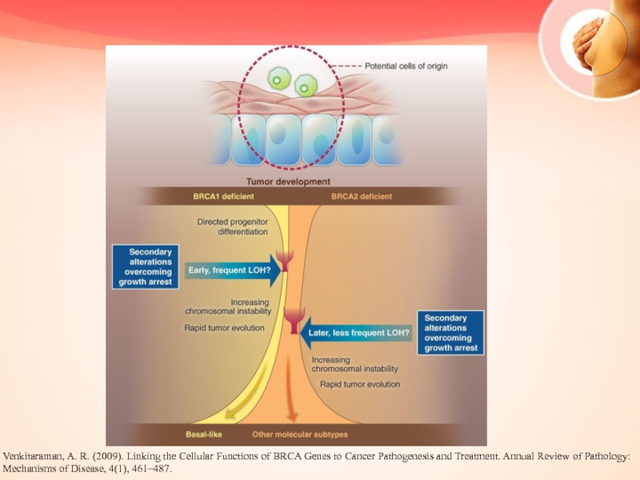
Your skin isn’t just a layer of cells. It’s a complex, multi-layered wall designed to keep water in and germs out. In chronic eczema, especially atopic dermatitis, that wall is cracked. Research shows this damage happens before any redness or itching shows up - often 3 to 6 months earlier in babies who later develop eczema. The problem? A genetic flaw in the filaggrin gene, found in about half of people with moderate to severe eczema. This gene makes a protein that helps hold skin cells together and creates natural moisturizers. When it’s broken, your skin loses water fast - up to 30 to 40 grams per square meter per hour, compared to 8 to 12 in healthy skin. That’s where Transepidermal Water Loss (TEWL) comes in. High TEWL means your skin is drying out from the inside out. As it dries, it cracks. Those cracks let in irritants, allergens, and bacteria like Staphylococcus aureus - which then trigger inflammation and itching. This isn’t just a reaction. It’s a chain reaction that starts with barrier failure.Barrier Repair: The Science Behind the Cream
Not all moisturizers are created equal. Basic lotions with petrolatum or glycerin might feel soothing, but they don’t fix the broken structure. True barrier repair means replacing what’s missing: ceramides, cholesterol, and free fatty acids - in the exact ratio your skin naturally uses: 1:1:1. Clinical trials show products with this ratio restore the skin’s lipid layers 87% of the time, compared to just 52% with regular emollients. Why? Because your skin recognizes these ingredients as its own. They slip into the cracks and rebuild the wall. One study found that after four weeks, people using these advanced formulations saw a 78% improvement in their eczema severity scores - nearly double the results of standard creams. The best products contain 3-5% ceramides, 2-4% cholesterol, and 1-3% free fatty acids. They’re also pH-balanced to 5.0-5.5. Why does pH matter? Because the enzyme that turns raw lipids into usable ones - β-glucocerebrosidase - works at 90% efficiency at pH 5.0, but only 40% at normal skin pH of 7.0. If the product is too alkaline, it won’t work. Brands like CeraVe, EpiCeram, and Vanicream have versions designed for this. Real users report dramatic changes: one Reddit user tracked their TEWL dropping from 38 to 15 g/m²/h after 30 days of daily use. Another said nighttime scratching dropped by 70%.What Makes Your Eczema Flare Up
Even with a repaired barrier, triggers can still set off flares. These aren’t random. They’re predictable - if you know what to look for.- Harsh soaps and detergents - even "fragrance-free" ones can strip lipids. Switch to soap-free cleansers like Cetaphil Gentle Skin Cleanser or Vanicream Cleansing Bar.
- Dry air - winter heating or air conditioning cuts humidity. Use a humidifier in bedrooms, especially during sleep.
- Sweat - salt and moisture irritate cracked skin. Rinse off after exercise and pat dry gently.
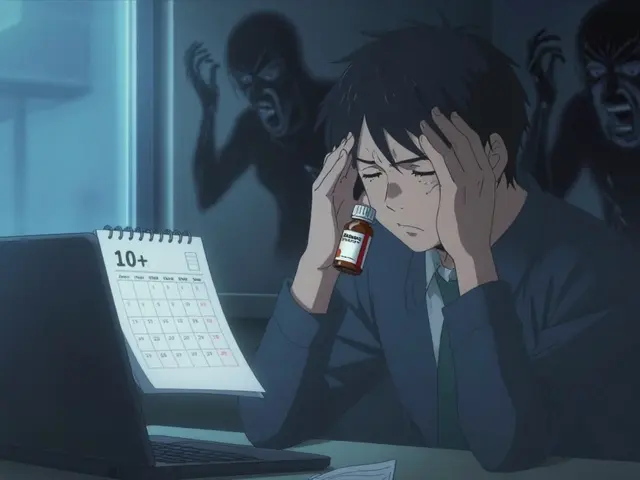
- Stress - cortisol spikes increase inflammation. It doesn’t cause eczema, but it fuels it.
- Food allergies - only relevant in about 30% of children with eczema, rarely in adults. Don’t eliminate foods without testing.
- Wool and synthetic fabrics - scratchy textures rub against broken skin. Stick to soft cotton.

How to Break the Itch-Scratch Cycle
Itching isn’t just annoying - it’s damaging. Scratching tears the barrier, releases more inflammation, and rewires your brain to crave the relief it gives. You’re not weak. You’re trapped in a biological loop. Here’s how to break it:- Cool compresses - damp, cool (not cold) washcloth on itchy spots for 10 minutes. Reduces nerve signals.
- Wet wrap therapy - after applying moisturizer, cover with damp cotton clothing or gauze, then a dry layer. Locks in moisture and blocks scratching. Works even better at night.
- Topical anti-itch creams - non-steroidal options like pimecrolimus or crisaborole reduce inflammation without thinning skin. Steroids like hydrocortisone 1% are fine short-term but shouldn’t be used daily long-term.
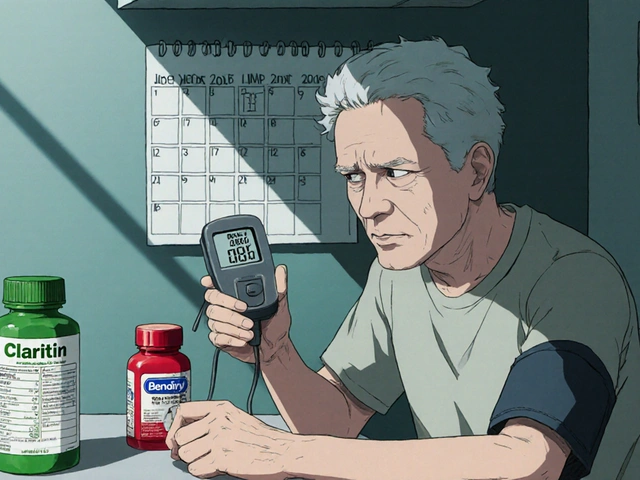
- Oral antihistamines - they don’t stop the itch from eczema (it’s not histamine-driven), but they help with sleep. Diphenhydramine or hydroxyzine at night can give you rest.
- Behavioral tricks - keep nails short. Wear cotton gloves at night. When the itch hits, press - don’t scratch. Tap. Pinch. Rub. Redirect the urge.
When Barrier Repair Alone Isn’t Enough
Here’s the hard truth: 30-40% of people with severe eczema won’t get full relief from barrier repair alone. Why? Because inflammation becomes self-sustaining. The immune system keeps firing, even after the barrier is fixed. If you’ve been using a ceramide cream twice daily for 8-12 weeks with no improvement, it’s time to talk to a dermatologist about immunomodulators. Topical JAK inhibitors like ruxolitinib cream reduce inflammation at the source. Oral medications like dupilumab (Dupixent) block key inflammatory signals. These aren’t "last resort" options - they’re tools. And they work best when paired with barrier repair. One case study followed a 7-year-old with severe eczema. After 6 months of barrier repair and dupilumab, his flare frequency dropped from weekly to once every 3 months. His steroid use dropped by 90%. He started sleeping through the night. He went back to swimming.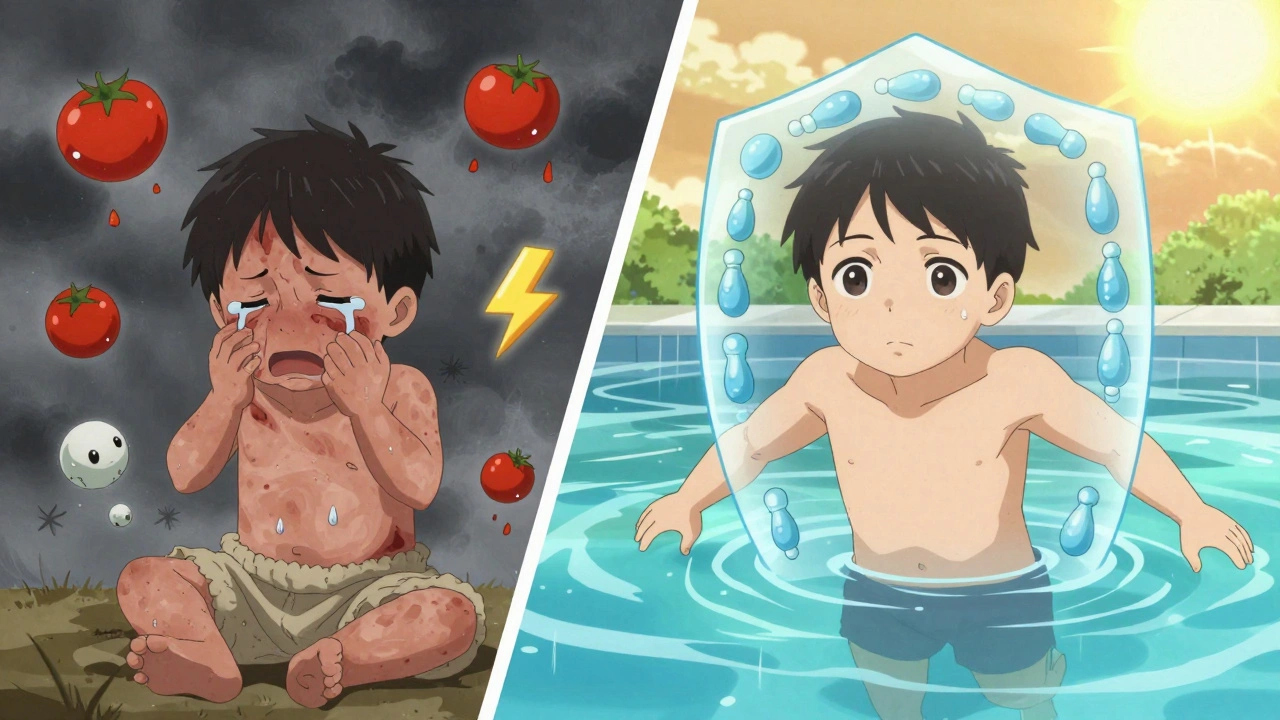
Cost, Compliance, and Real-Life Hurdles
The best barrier repair creams cost $25-$35 for 200g. Basic moisturizers? $10. That’s a big difference when you’re using 5 grams twice a day - that’s 300g a month. Insurance often covers prescription barrier creams like EpiCeram, but not OTC ones. Many people give up because of cost. Then there’s the texture. These creams are thicker. Greasier. They take time to absorb. Forty percent of users quit because they say it feels "too heavy." But here’s the trick: apply right after your shower, within 3 minutes. Your skin is still wet. The moisture gets trapped. You need less product. It absorbs faster. It feels less greasy. Use two fingertip units (the amount from the tip of your finger to the first joint) per arm. One for each leg. One for your torso. One for your face and neck. That’s about 30 grams a day. Sounds like a lot? It is. But think of it like brushing your teeth - it’s non-negotiable for your skin health.What’s Next for Eczema Treatment
The future is personal. Researchers are now linking filaggrin gene test results (like those from 23andMe) to specific barrier repair formulations. Algorithms can predict which ceramide mix will work best for your mutation - with 85% accuracy. Clinical trials are testing microbiome-targeted creams that add beneficial bacteria to crowd out staph. Platelet-rich plasma (PRP) injections are being studied for their ability to boost filaggrin production by 300%. By 2030, barrier repair is expected to make up half of all eczema treatment. Right now, it’s 35%. The shift is happening. But you don’t have to wait. The tools are here now.Start Here: Your 7-Day Barrier Repair Plan
- Day 1-2: Stop using harsh soaps. Switch to a soap-free cleanser. Buy a ceramide-based cream (CeraVe, Vanicream, or EpiCeram). Start applying twice daily - morning and night.
- Day 3-4: Apply immediately after showering. Use 5g per limb. Don’t rub. Pat gently. Use gloves at night if you scratch.
- Day 5-6: Track triggers. Write down what you ate, wore, or did before a flare. Note humidity, stress, sweat.
- Day 7: Reassess. Are you itching less? Is skin less red? Are you sleeping better? If yes - keep going. If no - talk to a dermatologist about next steps.
Can I use regular lotion for chronic eczema?
Regular lotions with water, glycerin, or petrolatum can soothe dryness, but they don’t repair the skin’s lipid barrier. For chronic eczema, you need products with ceramides, cholesterol, and free fatty acids in a 1:1:1 ratio. These mimic your skin’s natural structure and actually rebuild it. Basic lotions are like putting tape over a broken pipe - they mask the problem. Ceramide creams fix the pipe.
How long does it take to see results from barrier repair?
You’ll notice less dryness in a few days, but real barrier repair takes time. Clinical studies show significant TEWL reduction after 2 weeks, and major improvements in eczema severity after 4-6 weeks of consistent use. Don’t give up before day 28. The skin rebuilds slowly, like healing a fracture. You wouldn’t stop wearing a cast after 5 days.
Why does my eczema cream sting when I apply it?
Stinging usually means your skin is cracked and inflamed. Barrier repair creams often have a slightly acidic pH (5.0-5.5) to activate repair enzymes. That can burn on open cracks. It’s not the product - it’s the damage. Apply over damp skin, not dry. Use a thin layer. The sting should fade within 3-5 days as the barrier heals. If it doesn’t, switch to a neutral pH product like Vanicream.
Can I use steroid cream and barrier cream together?
Yes - but not at the same time. Apply steroid cream first, wait 15 minutes, then apply barrier cream. If you apply them together, the steroid can’t penetrate properly, and the barrier cream may dilute it. Think of it like applying sunscreen after moisturizer - order matters. Always follow your doctor’s instructions.
Is eczema caused by allergies?
Allergies can trigger flares, but they don’t cause eczema. The root cause is genetic - specifically, a faulty skin barrier. Many people with eczema have no food or environmental allergies. Even if you do have allergies, treating them won’t cure eczema. You still need barrier repair. Think of allergies as sparks - the barrier is the fuel. Fix the fuel, and the sparks matter less.
Do I need to use barrier cream forever?
Not forever - but long-term maintenance is key. Once your skin is healed, you can reduce frequency to once a day or every other day. But stop completely, and the barrier will weaken again. Eczema is a chronic condition, like high blood pressure. You don’t take blood pressure meds forever because you’re cured - you take them because your body needs support. Same here.




Webster Bull December 13, 2025
Barriers don’t fix themselves. You gotta rebuild ‘em like a damn brick wall. Ceramides = mortar. Cholesterol = rebar. Fatty acids = the damn bricks. Stop slapping on lotion like it’s perfume. This ain’t skincare. It’s structural repair.
John Fred December 14, 2025
YES. YES. YES. 🙌 Ceramide trio is the holy trinity. I used CeraVe for 6 weeks and my hands stopped looking like dragon skin. Also, wet wraps at night? Game. Changer. 🛌💧
Harriet Wollaston December 14, 2025
I used to think I was just ‘dry’ until I read this. My skin wasn’t broken-it was abandoned. And honestly? The fact that you said ‘you’re not weak’? I cried. Thank you for seeing us.
Lauren Scrima December 14, 2025
Ohhh so THAT’S why my ‘natural’ coconut oil cream made it worse… 🤦♀️. I mean, I knew it was greasy, but I didn’t realize I was literally gluing my skin’s front door shut with butter. Thanks for the reality check.
Hamza Laassili December 15, 2025
Why are we paying $30 for cream when we got soap and water for 1000 years?! This is just corporate greed dressed up as science. My grandpa had eczema and he just used lard. And he lived to 92. 🇺🇸
Casey Mellish December 15, 2025
Barriers aren’t just physical-they’re psychological too. The itch-scratch loop rewires your nervous system. That’s why behavioral tricks work. It’s not discipline. It’s neuroplasticity. You’re literally retraining your brain to stop screaming for damage.
Emily Haworth December 16, 2025
Wait… so if you’re using ceramides, are you basically feeding your skin GMO ingredients? Who’s testing these creams? Are they linked to the 5G skin cancer plot? I’ve been getting rashes since the new iPhone 15…
Yatendra S December 18, 2025
Is it possible… that the skin barrier is just a metaphor? Like… our emotional walls? The itch… is unresolved trauma? I’ve been meditating for 2 months and my eczema improved. Coincidence? Or… deeper truth?
Himmat Singh December 20, 2025
While the biochemical rationale presented is methodologically sound, it is imperative to acknowledge that the empirical efficacy of ceramide-based formulations remains contingent upon adherence to rigid application protocols and environmental control. The conflation of anecdotal testimonials with clinical outcomes constitutes a fallacy of composition, and the implicit recommendation of commercial products may constitute an implicit conflict of interest. One must exercise epistemological caution before embracing therapeutic paradigms that lack longitudinal, double-blind validation.