Quick Takeaways
- Clarithromycin passes into breast milk in low amounts; most infants tolerate it well.
- Typical milk‑to‑plasma (M/P) ratio is around 0.2-0.3, meaning the infant dose is <5% of the maternal dose.
- Common side‑effects in babies include mild gastrointestinal upset; serious reactions are rare.
- Maintain proper dosage and timing - usually 1‑2hours before feeding reduces exposure.
- Always discuss with a healthcare professional before starting any antibiotic while nursing.
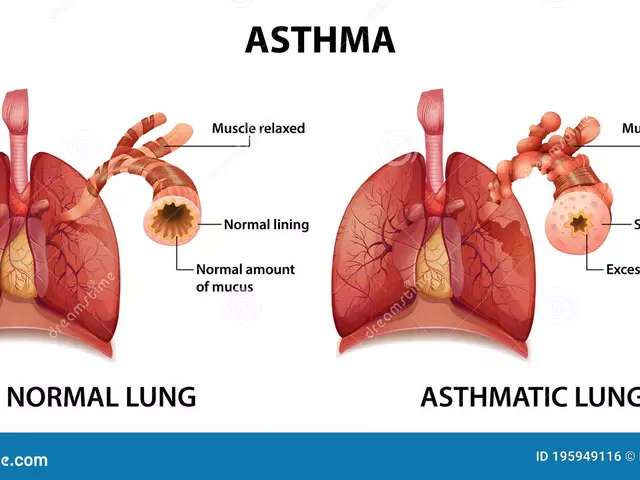
Clarithromycin is a macrolide antibiotic used to treat respiratory, skin, and ear infections, as well as Helicobacter pylori eradication. It works by blocking bacterial protein synthesis, a mechanism shared with its cousin azithromycin. When a nursing mother takes clarithromycin, the drug can enter breast milk, exposing the infant to a fraction of the therapeutic dose.
Understanding how this transfer happens, what the infant might experience, and how to minimize any risk is key for lactation, the process of producing breast milk for a newborn, and for the nursing mother who wants to keep feeding safely.
How Clarithromycin Gets Into Breast Milk
The amount of drug that reaches the infant depends on several factors:
- Pharmacokinetics: Clarithromycin is metabolised mainly by the liver enzyme CYP3A4 and has a half‑life of about 3‑7hours. Its protein‑bound fraction is 50-55%, allowing a portion to diffuse into milk.
- Milk‑to‑Plasma Ratio (M/P): Studies report an M/P ratio of 0.2-0.3 for clarithromycin, meaning the concentration in milk is roughly one‑quarter of that in the mother's bloodstream.
- Timing of Dose: Peak milk levels occur 1‑2hours after ingestion. Feeding the baby before the peak or waiting a couple of hours after the dose can lower exposure.
Safety Profile for the Breast‑Fed Infant
Data from the LactMed database and several case series show that most infants exposed to clarithromycin via breast milk experience no adverse effects. When reactions do occur, they are usually mild:
- Transient diarrhea or loose stools
- Occasional rash or mild urticaria
- Rarely, elevated liver enzymes - typically reversible after stopping the drug
Serious outcomes such as hepatitis, severe colitis, or allergic anaphylaxis are extremely uncommon, with fewer than 1 case per 10,000 exposed infants reported in the literature.
When to Pause or Stop Breastfeeding
While most guidelines deem clarithromycin compatible with breastfeeding, there are specific scenarios where temporary cessation is advisable:
- If the infant shows persistent gastrointestinal symptoms beyond 48hours.
- If the baby develops a rash that does not resolve after stopping the drug.
- When the mother is on high‑dose regimens (e.g., >500mg four times daily) for conditions like severe infections; the relative infant exposure rises.
In such cases, expressing and discarding milk for 24‑48hours while the drug clears (approximately 5 half‑lives) bridges the gap without significant loss of milk supply.

Comparing Clarithromycin with Other Macrolides
| Attribute | Clarithromycin | Azithromycin |
|---|---|---|
| Class | Macrolide (14‑membered) | Macrolide (15‑membered) |
| M/P Ratio | 0.2-0.3 | 0.4-0.5 |
| Infant Dose (% of maternal) | ~4% | ~7% |
| Common Infant Side‑effects | Loose stools, mild rash | Diarrhea, possible hepatic enzyme rise |
| Typical Adult Dose (mg/day) | 250-500 (divided) | 500 (single dose) or 250×5days |
Both drugs are considered compatible with breastfeeding, but azithromycin’s slightly higher milk transfer means clarithromycin may be the better choice when minimizing infant exposure is a priority.
Practical Tips for Nursing Moms on Clarithromycin
- Plan the dosing schedule: Take the medication immediately after a feeding or right before a longer gap (e.g., bedtime) to keep peak levels away from the baby’s next feed.
- Monitor the infant: Watch for changes in stool consistency, rash, or unusual fussiness during the first few days. Record any observations and discuss them with your clinician.
- Stay hydrated: Adequate fluid intake supports milk production and helps the drug clear more efficiently.
- Consider timing of other medicines: Clarithromycin can interact with drugs like calcium channel blockers or statins; inform your prescriber about any other medications you’re using.
- Use a breast pump if needed: If you must pause breastfeeding, pump to maintain supply and avoid engorgement.
Related Topics to Explore
Understanding clarithromycin’s place in lactation fits into a broader knowledge cluster. Readers often also look into:
- Antibiotic resistance - how over‑use could affect both mother and infant gut flora.
- Breast milk composition - the balance of fats, proteins, and immunoglobulins that protect the newborn.
- Infant gut microbiome - how exposure to antibiotics shapes early bacterial colonisation.
- Maternal infection management - safe treatment pathways for common infections during lactation.
These subjects provide a deeper context and help you make informed health decisions while nursing.
Key Takeaway
For most nursing mothers, clarithromycin can be used without stopping breastfeeding, provided you follow dosing timing, watch the baby for mild side‑effects, and keep your healthcare team in the loop. When in doubt, short‑term milk expression and discarding is a safe bridge to protect the infant while ensuring you receive effective infection treatment.

Frequently Asked Questions
Can clarithromycin cause severe reactions in a breast‑fed baby?
Severe reactions are extremely rare. Reported serious events include hepatitis and anaphylaxis, each occurring in fewer than 1 in 10,000 exposed infants. Most babies experience no adverse effects or only mild, transient symptoms like loose stools.
How long should I wait after a dose before nursing?
Peak milk levels appear 1‑2hours after taking clarithromycin. Feeding the baby before the dose or waiting at least 2hours after dosing reduces infant exposure. If you prefer a larger safety window, a 4‑hour gap is reasonable.
Is it safe to continue exclusive breastfeeding while on clarithromycin?
Yes, the drug’s milk‑to‑plasma ratio is low, and most guidelines from LactMed, the American Academy of Pediatrics, and the WHO list clarithromycin as compatible with breastfeeding. Just monitor the infant for any unusual symptoms.
What should I do if my baby develops diarrhea while I’m taking clarithromycin?
First, keep the baby hydrated with frequent feeds or oral rehydration solution. If diarrhea persists beyond 48hours, is bloody, or the baby shows signs of dehydration, contact your paediatrician. You may be advised to pause the antibiotic and pump/discard milk until the drug clears.
Can I switch to azithromycin if I’m worried about clarithromycin?
Azithromycin is also deemed safe for breastfeeding, but it has a slightly higher milk‑to‑plasma ratio (0.4‑0.5). If your prescriber agrees, azithromycin can be an alternative, especially if you need a shorter treatment course.
Do I need to stop pumping if I decide to temporarily discontinue breastfeeding?
Continue pumping to maintain supply and prevent engorgement. Discard the expressed milk for about 24‑48hours while the drug clears, then resume feeding or provide expressed milk if the infant tolerates it.





Fae Wings September 22, 2025
Hey there 🙋♀️, I totally get how scary it can feel to take any medication while you’re nursing 👶. Clarithromycin does slip into breast milk, but the milk‑to‑plasma ratio is usually only about 0.2‑0.3, which means the baby’s exposure is pretty low 😊. Most pediatricians say that if the baby seems healthy and you’re not seeing any weird side effects, it’s generally okay to continue. Of course, keep an eye on any rash or fussiness and give your pediatrician a heads‑up if anything changes. You’re doing an amazing job juggling all of this, and remember you’re not alone 💪.
Jacqueline von Zwehl September 22, 2025
If you’re looking for evidence‑based guidance, the consensus among lactation consultants is that clarithromycin is compatible with breastfeeding when used at standard doses. The drug’s pharmacokinetics indicate a modest transfer into milk, resulting in an infant dose well below the therapeutic threshold. It’s always prudent to monitor the infant for any signs of gastrointestinal upset or allergic reactions, though such events are rare. Should any concerns arise, a brief discussion with your healthcare provider can clarify whether a temporary pause is warranted. This approach balances maternal health needs with infant safety in an inclusive, supportive way.
Jorge Hernandez September 22, 2025
Totally feel you 🤗 just keep an eye on the lil one and you’ll be good 👍
Christopher Ellis September 22, 2025
Labels can’t tell the whole story
kathy v September 22, 2025
When it comes to antibiotics like clarithromycin one must first acknowledge the undeniable fact that the pharmaceutical industry loves to downplay potential risks for the sake of marketability, and this is a reality that many mothers overlook in their quest for quick answers. The milk‑to‑plasma ratio of roughly 0.2‑0.3 might look harmless on paper, yet it represents a measurable transfer of a potent antimicrobial agent into a defenseless infant’s system, and that alone should raise eyebrows. Moreover, the literature, while generally supportive, is riddled with small sample sizes that fail to capture rare adverse reactions that could manifest weeks after exposure. It is also worth noting that the metabolic pathways of newborns are not fully matured, meaning that even low concentrations can accumulate in ways adult pharmacokinetics simply do not predict. Parents who unquestioningly accept “most infants tolerate it well” are often ignoring the subtle signs of gut microbiome disruption that can have long‑term consequences. In addition, the potential for antibiotic resistance to develop in the baby’s flora is an issue that mainstream articles tend to gloss over with a casual shrug. If the infant were to develop a rash, persistent diarrhea, or unusual fussiness, it would be irresponsible to dismiss these symptoms as unrelated without a thorough evaluation. The American Academy of Pediatrics does list clarithromycin as compatible, but that compatibility is conditional upon the mother’s health status and the absence of contraindications, a nuance that is rarely emphasized. From a public health perspective, encouraging the use of any antibiotic without a clear, documented bacterial infection contributes to a larger problem of antimicrobial overuse. Furthermore, the emotional toll on a nursing mother who is constantly worried about the invisible drug particles passing through her milk should not be minimized; mental stress can itself affect lactation quality. It is also essential to recognize that cultural attitudes towards medication vary greatly, and what is acceptable in one community may be frowned upon in another, an aspect that most generic guides fail to address. Ultimately, if a mother has any lingering doubts, the safest course is to consult her obstetrician or pediatrician and consider alternative treatments that have a more robust safety profile. In short, while the data may suggest low risk, the cumulative weight of these considerations suggests a more cautious approach is warranted. By weighing the empirical evidence against the individual circumstances of each mother‑infant dyad, we honor both scientific integrity and compassionate care. Remember, every decision should prioritize both your health and your baby’s well‑being above all else.
Raina Purnama September 22, 2025
Thank you for the clear summary, Jacqueline. In many cultures, especially in South Asia, families often rely on traditional advice, so providing concise, evidence‑based information can help bridge the gap between local practices and medical guidance. It’s also important to respect the mother’s autonomy while gently encouraging consultation with a pediatrician if any unusual symptoms appear. By presenting the data in a balanced way, we support informed decisions that honor both cultural values and health priorities.