Antipsychotic Treatment Matchmaker
How This Tool Works
Answer these questions to get a personalized recommendation for your situation. Based on the article content, this tool helps you compare Clozapine and other antipsychotics against your specific needs and concerns.
Quick Summary
- Clozapine is reserved for treatment‑resistant schizophrenia because it works when other drugs fail.
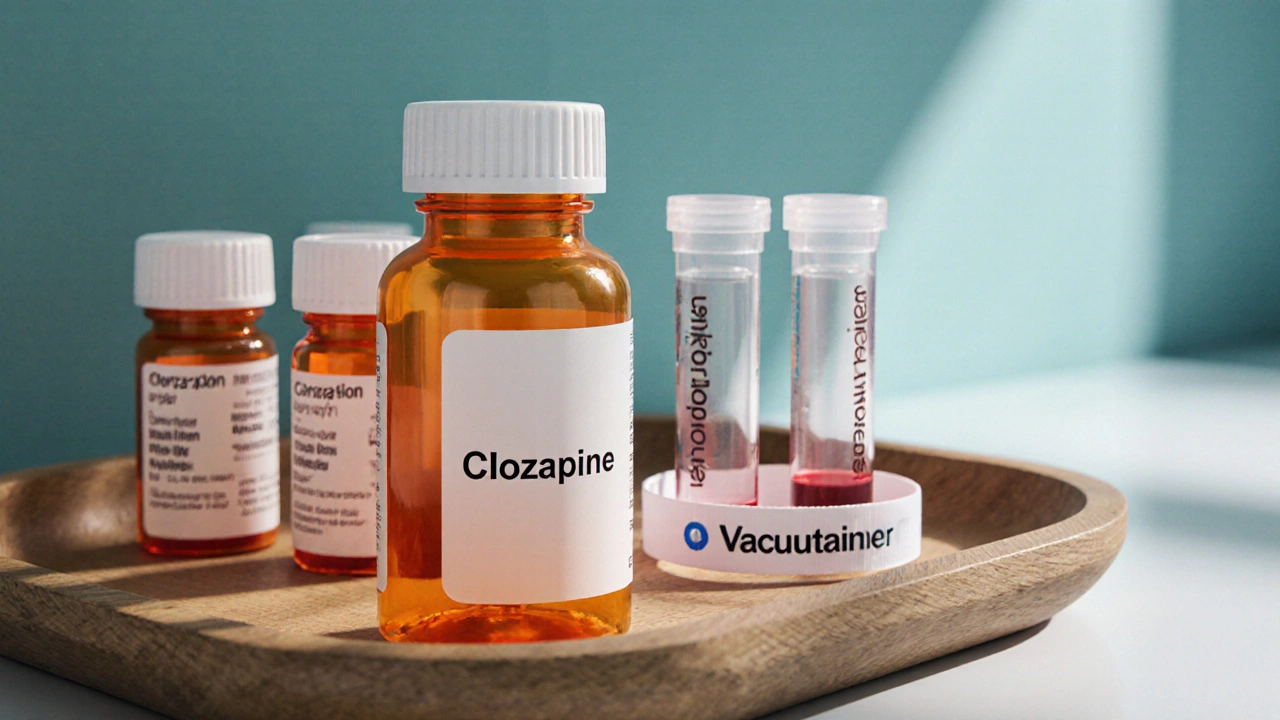
- It requires regular blood monitoring to avoid rare but serious side effects such as agranulocytosis.
- Common alternatives (Risperidone, Olanzapine, Quetiapine, Haloperidol, Aripiprazole) differ in efficacy, metabolic risk, and monitoring needs.
- Cost and insurance coverage vary widely; generic versions of many alternatives are cheaper than Clozapine.
- Choosing the right drug means balancing symptom control, side‑effect profile, lifestyle, and the ability to stick to monitoring schedules.
When treating treatment‑resistant schizophrenia, Clozapine is a second‑generation antipsychotic that uniquely blocks dopamine D2 receptors while also modulating serotonin 5‑HT2A. It was first approved in the United States in 1989 and quickly became the gold standard for patients who do not respond to at least two other antipsychotics.
What Is Clozapine and When Is It Used?
Clozapine is indicated for schizophrenia that has not improved after trials of other antipsychotics. The drug is especially effective at reducing both positive symptoms (hallucinations, delusions) and negative symptoms (social withdrawal, flat affect). Because of its superior efficacy, clinicians reserve it for patients who have failed at least two other agents.
Typical dosing starts at 12.5mg once or twice daily, titrating up to 300-600mg per day depending on response and tolerability. Clozapine reaches steady‑state levels after about two weeks, but the therapeutic window is narrow, which is why blood tests are mandatory.
How Clozapine Works - A Brief Mechanism
The drug’s affinity for dopamine D2 receptors is weaker than that of many older antipsychotics, reducing the risk of extra‑pyramidal symptoms (EPS). Simultaneously, it strongly antagonizes serotonin 5‑HT2A receptors, a property linked to improvements in mood and cognition. This dual action explains why Clozapine can calm severe psychosis without causing the stiffness common to first‑generation drugs.
Besides dopamine and serotonin, Clozapine also interacts with muscarinic, histamine, and α‑adrenergic receptors, contributing to side‑effects like weight gain, sedation, and sialorrhea (excessive saliva).
Key Alternatives to Clozapine
Below are the most frequently considered alternatives, each with its own balance of efficacy, side‑effects, and monitoring requirements.
- Risperidone a second‑generation antipsychotic with strong D2 antagonism and moderate 5‑HT2A blockade
- Olanzapine known for high efficacy but a high risk of metabolic syndrome
- Quetiapine offers sedation and mood‑stabilising benefits, useful in schizoaffective disorder
- Haloperidol a first‑generation antipsychotic with potent D2 blockade, high EPS risk
- Aripiprazole a partial D2 agonist that can feel “lighter” for patients sensitive to sedation
Side‑Effect Profiles - What Sets Clozapine Apart?
All antipsychotics carry side‑effects, but Clozapine’s rare, life‑threatening risks demand special attention.
- Agranulocytosis: a drop in white‑blood‑cell count occurring in 0.5-1% of patients; requires weekly blood draws for the first six months, then bi‑weekly.
- Myocarditis: inflammation of the heart muscle, most common in the first month of treatment.
- Metabolic changes: weight gain, glucose intolerance, and dyslipidaemia are moderate compared with Olanzapine.
- Seizures: risk rises when doses exceed 600mg/day.
In contrast, Risperidone and Haloperidol have higher EPS rates, while Olanzapine’s metabolic impact can be severe enough to trigger type2 diabetes. Quetiapine’s sedation can be beneficial for insomnia but may impair daytime functioning. Aripiprazole often has the cleanest metabolic profile but may be less effective for severe positive symptoms.
Comparison Table - Efficacy, Side Effects, Monitoring, Cost
| Drug | Efficacy in Treatment‑Resistant Schizophrenia | Major Side‑Effects | Monitoring Needed | Typical Monthly Cost (USD) |
|---|---|---|---|---|
| Clozapine | High - 30‑60% remission when others fail | Agranulocytosis, myocarditis, weight gain, seizures | Weekly CBC for 6months, then bi‑weekly | $150-$250 (brand) / $80-$120 (generic) |
| Risperidone | Moderate - effective for many, limited in resistant cases | EPS, hyperprolactinaemia, mild weight gain | None beyond routine labs | $30-$60 |
| Olanzapine | High - comparable efficacy, but metabolic risks | Weight gain, hyperglycaemia, dyslipidaemia | Fasting glucose & lipid panel every 3months | $45-$90 |
| Quetiapine | Low‑moderate - good for mood symptoms | Sedation, orthostatic hypotension, modest weight gain | Blood pressure & glucose quarterly | $35-$70 |
| Haloperidol | Moderate - strong for positive symptoms | High EPS, tardive dyskinesia, prolactin elevation | Movement‑disorder monitoring regularly | $15-$30 |
| Aripiprazole | Moderate - may be less potent for severe cases | Akathisia, insomnia, low metabolic impact | None specific beyond routine checks | $60-$120 |
How to Decide Which Medication Fits Your Situation
Think of the choice as a simple decision tree:
- Is the current regimen failing? If you’ve tried two different antipsychotics at adequate doses, Clozapine becomes a serious option.
- Can you commit to regular blood tests? Weekly draws are a non‑negotiable safety measure for Clozapine.
- What side‑effects are most concerning? If weight gain or diabetes is a red flag, you might lean toward Risperidone or Aripiprazole. If EPS is intolerable, avoid Haloperidol.
- What does your insurance cover? Many health plans place Clozapine on a specialty tier, raising out‑of‑pocket costs.
Talk with your psychiatrist about these factors. They can run a simple metabolic panel, assess your blood‑count baseline, and weigh the benefits of symptom control against the logistics of monitoring.

Monitoring & Safety - Practical Tips
Regardless of the drug you end up on, a few universal safety habits help keep you on track.
- Maintain a medication diary: note dose changes, side‑effects, and how you feel each day.
- Schedule blood work in advance - many labs allow you to drop off a sample without an appointment.
- Stay hydrated and eat a balanced diet; this mitigates weight gain and metabolic drift.
- If you experience fever, sore throat, or flu‑like symptoms while on Clozapine, contact your clinician immediately - these can precede agranulocytosis.
Real‑World Scenario: Why Some Patients Switch Away from Clozapine
Sarah, a 28‑year‑old from Manchester, was diagnosed with schizophrenia at 22. After trials of Risperidone and Olanzapine, she still heard voices. Her psychiatrist started Clozapine; within weeks, the voices faded. However, Sarah struggled with weekly blood tests because of a demanding job and long commute. After a year, she experienced mild weight gain and occasional dizziness. Her doctor transitioned her to Aripiprazole, which preserved most of the symptom relief while eliminating the need for CBC monitoring. Sarah’s story illustrates that Clozapine’s power can be a temporary bridge rather than a lifelong solution for many patients.
Bottom Line
If you or a loved one have not responded to at least two other antipsychotics, Clozapine is the most evidence‑backed option, but it comes with strict monitoring and a unique side‑effect profile. Alternatives like Risperidone, Olanzapine, Quetiapine, Haloperidol, and Aripiprazole each have strengths-lower monitoring burden, different metabolic risks, or fewer movement‑related side‑effects. The right choice hinges on efficacy, safety, lifestyle, and cost considerations.
Frequently Asked Questions
Can I stop Clozapine abruptly?
No. Stopping suddenly can cause withdrawal symptoms and a rebound of psychosis. Any change should be tapered under a psychiatrist’s supervision.
How long does the blood‑test schedule last?
Weekly during the first six months, then every two weeks for the next six months. After a year of stable counts, some clinicians shift to monthly checks.
Is Clozapine safe during pregnancy?
Data are limited. The drug crosses the placenta and may cause neonatal neutropenia. Only use if the benefits outweigh the risks, and involve both psychiatry and obstetrics.
What makes Olanzapine’s metabolic side‑effects worse than Clozapine’s?
Olanzapine has a stronger affinity for histamine H1 and serotonin 5‑HT2C receptors, which drive appetite and insulin resistance. Clozapine’s metabolic impact is moderate because its receptor profile is less skewed toward those pathways.
Do all antipsychotics require blood monitoring?
Only Clozapine (and its close relative, Olanzapine in rare cases) demands routine CBCs. Other agents rely on periodic metabolic panels or movement‑disorder checks, but no weekly blood draws.





Leah Robinson October 11, 2025
Sounds like a solid guide-if you can handle the blood draws, Clozapine can be a game‑changer 😊
Abhimanyu Lala October 19, 2025
Clozapine is like the final boss of meds no chill
Richard Sucgang October 27, 2025
Clozapine remains the most effective option for treatment‑resistant schizophrenia, a fact supported by decades of clinical trials. Its unique receptor profile, with moderate dopamine D2 antagonism and strong serotonin 5‑HT2A blockade, accounts for its superior efficacy on both positive and negative symptoms. However, this pharmacologic advantage comes with a responsibility to monitor blood counts because of the rare but serious risk of agranulocytosis. Weekly complete blood counts are required for the first six months, after which the schedule can be reduced to bi‑weekly if counts remain stable. In addition to hematologic concerns, clinicians must remain vigilant for myocarditis, especially during the first month of therapy. Metabolic side effects such as modest weight gain and dyslipidemia are also observed, though they are generally less severe than those seen with olanzapine. Seizure risk increases at doses above 600 mg per day, so dose titration should be cautious. Compared with first‑generation agents like haloperidol, Clozapine produces far fewer extrapyramidal symptoms, making it a preferred choice when movement disorders are a major worry. The drug’s cost, ranging from $80 to $250 monthly depending on brand or generic status, can be a barrier for patients without comprehensive insurance coverage. Some health plans place Clozapine on a specialty tier, which may increase out‑of‑pocket expenses and require prior authorization. Despite these hurdles, the remission rates of 30‑60 % in patients who have failed two other antipsychotics highlight its clinical value. It is essential for prescribers to discuss the monitoring schedule, potential side effects, and financial considerations before initiating therapy. Patients should also be educated to report any flu‑like symptoms promptly, as they may herald an impending drop in neutrophil counts. In practice, many clinicians use Clozapine as a bridge, eventually switching to a less burdensome agent once symptom control is achieved. Ultimately, the decision balances efficacy against the logistical and safety demands of regular blood testing.
Russell Martin November 4, 2025
If you start Clozapine, set up your weekly CBCs now so you don’t miss a beat and can keep the medication working for you.
Jenn Zee November 12, 2025
It is frankly astonishing how often clinicians overlook the moral imperative of presenting the full spectrum of risks before prescribing a drug that can literally take a patient’s blood. The literature is replete with data on agranulocytosis, yet many prescribers gloss over it in favor of a shiny efficacy headline. One must consider not only the pharmacodynamics but also the socioeconomic fallout when patients are forced into a regime of weekly phlebotomy. The hidden costs-transportation, time off work, childcare-are rarely quantified in trial reports, creating a veneer of accessibility that quickly crumbles in real‑world practice. Moreover, the emphasis on remission rates can obscure the lived experience of patients who endure months of fatigue and anxiety awaiting lab results. It is a disservice to the patient community to treat Clozapine as a panacea without acknowledging its demanding monitoring choreography. Ethical prescribing demands transparency, shared decision‑making, and a realistic appraisal of both benefits and burdens. Anything less betrays the trust that underpins the therapeutic alliance.
don hammond November 19, 2025
Oh sure, because we all have a spare hour every week to sit in a clinic-*sarcasm intensifies* 😂 If you love paperwork more than Netflix, Clozapine’s your jam.
Ben Rudolph November 27, 2025
Some of the side‑effect statistics feel cherry‑picked, leaving out the thousands who drop out early.
Ian Banson December 5, 2025
Let’s not forget that Clozapine’s average monthly cost sits well above most generics, often exceeding $200 without insurance subsidies-a fact that many tables skim over in favor of efficacy charts.
marcel lux December 13, 2025
You make a solid point about cost; it’s also worth noting that many insurers require prior authorization, which can add weeks to the start date and frustrate patients who need rapid symptom control.
Charlotte Shurley December 21, 2025
The article does a good job summarizing the monitoring schedule, but remember that adherence to weekly labs is the single biggest predictor of safe Clozapine use.
Steph Hooton December 28, 2025
In conclusion, for anyone facing treatment‑resistant schizophrenia, Clozapine offers unparalleled efficacy, yet the decision must weigh the rigorous monitoring requirements, potential side‑effects, and financial implications. With proper support and a clear plan, many patients achieve meaningful improvement.