Coronary artery disease (CAD) isn’t just a slow leak in your heart’s plumbing-it’s a silent, creeping threat that kills more people worldwide than any other condition. It’s the main reason heart attacks happen, and it starts long before you feel any symptoms. At its core, CAD is caused by atherosclerosis: the buildup of fatty, fibrous plaques inside the arteries that feed your heart. These plaques don’t just clog the pipes-they can suddenly rupture and trigger a clot that blocks blood flow completely. That’s when the emergency room lights flash.
How Atherosclerosis Turns Coronary Arteries Into Time Bombs
Atherosclerosis begins when low-density lipoprotein (LDL), often called "bad cholesterol," slips through the inner lining of your arteries. Your body sees it as an invader and sends in immune cells. Over time, these cells, along with calcium and other debris, form plaques that harden and narrow the arteries. Think of it like rust building up inside a water pipe-except here, the rust is made of fat, inflammation, and scar tissue.
Not all plaques are the same. Some are stable-thick, fibrous, and slow-growing. These can narrow the artery by more than 50% and cause predictable chest pain when you’re exerting yourself. But the real danger lies in unstable plaques. These have a large oily core, thin outer walls, and are packed with immune cells. They might only block 30% of the artery, but they’re ticking time bombs. One sneeze, a spike in blood pressure, or even a stressful morning can make them rupture. That’s when a blood clot forms instantly, cutting off oxygen to part of your heart muscle. That’s a heart attack.
Research shows that 75% of all major heart events happen in people with these unstable plaques. And here’s the twist: many people with severe narrowing never have symptoms, while others with minimal narrowing suffer sudden cardiac events. That’s why diagnosis isn’t just about how clogged the artery looks-it’s about what the plaque is made of.
The Real Risk Factors Behind CAD-Beyond Just High Cholesterol
Most people think high cholesterol is the main culprit. It’s a big piece, but not the whole puzzle. The 2023 American College of Cardiology and American Heart Association guidelines list clear risk categories that go far beyond diet:
- Smoking-Even occasional smoking damages the artery lining and speeds up plaque formation. One pack a day triples your risk.
- Diabetes-High blood sugar eats away at blood vessels. People with diabetes have the same heart attack risk as someone who already had one.
- High blood pressure-Constant pressure on artery walls makes them crack and scar, giving plaques a place to stick.
- Obesity-Especially belly fat. It’s not just weight-it’s inflammation. Fat tissue releases chemicals that trigger arterial damage.
- Family history-If a parent had heart disease before 55 (men) or 65 (women), your risk jumps.
- Chronic kidney disease-A kidney function below 60 mL/min (eGFR) is a red flag. Your arteries and kidneys suffer together.
- Atrial fibrillation-This irregular heartbeat doesn’t just raise stroke risk-it also increases heart attack risk.
Here’s what most don’t realize: You can have normal cholesterol and still be at high risk. A 2023 study found that 60% of people with CAD had at least two of these high-risk features. That’s why doctors now classify risk into three levels:
- Low risk: Less than 1% chance of heart attack or death per year
- Intermediate risk: 1% to 3% per year
- High risk: Over 3% per year-this group accounts for most heart attacks
If you’ve had a prior heart attack, bypass surgery, or stent, you’re automatically in the high-risk category. No matter how good your numbers look.

How Doctors Diagnose CAD-What Tests Actually Tell You
There’s no single test that catches CAD early. It’s a process. Most people don’t get diagnosed until they’re in pain.
An ECG (electrocardiogram) is the first step. It reads your heart’s electrical activity. If you’re having a heart attack, it shows clear signs. But if you’re not in crisis, it might look normal-even if plaques are forming.
Stress tests are more revealing. You walk on a treadmill or take medicine to make your heart work harder. If your heart doesn’t get enough blood during stress, it shows up as abnormal patterns. This catches blockages that ECGs miss.
The gold standard is coronary angiography. A thin tube is threaded into your artery, dye is injected, and X-rays show exactly where blockages are. It’s invasive, but it’s the only way to see plaque size, location, and whether a vessel is fully blocked.
Another underrated tool? The Ankle-Brachial Index (ABI). It measures blood pressure in your ankle compared to your arm. If it’s low, it means arteries in your legs are clogged-and if your leg arteries are blocked, your heart arteries likely are too. About half of people with CAD also have peripheral artery disease.
And here’s something new: doctors are now using advanced imaging to look at plaque composition, not just size. CT scans with special software can tell if a plaque is fatty and unstable-or thick and safe. This helps decide whether you need surgery or just medication.
Treatments That Work-From Lifestyle to Surgery
There’s no magic pill that erases plaque. But there are proven ways to stop it from getting worse-and even shrink it.
Lifestyle changes aren’t just advice-they’re medicine. The 2023 guidelines say this is the foundation of treatment:
- Stop smoking-your arteries start healing within weeks
- Move daily-even 30 minutes of brisk walking lowers risk by 30%
- Eat real food: vegetables, whole grains, nuts, fish. Avoid processed carbs and trans fats
- Lose weight if you’re overweight-just 5-10% can improve blood pressure and insulin sensitivity
Medications are non-negotiable for most people with CAD:
- Statins-Lower LDL cholesterol by 50% or more. They also stabilize plaques and reduce inflammation. Most people need them for life.
- Aspirin-Low-dose daily aspirin prevents clots. Not for everyone-only if your risk is high enough.
- BP meds-ACE inhibitors or ARBs protect your heart and kidneys.
- SGLT2 inhibitors or GLP-1 agonists-Originally for diabetes, these now show strong heart protection even in non-diabetics.
If medications aren’t enough, procedures come in:
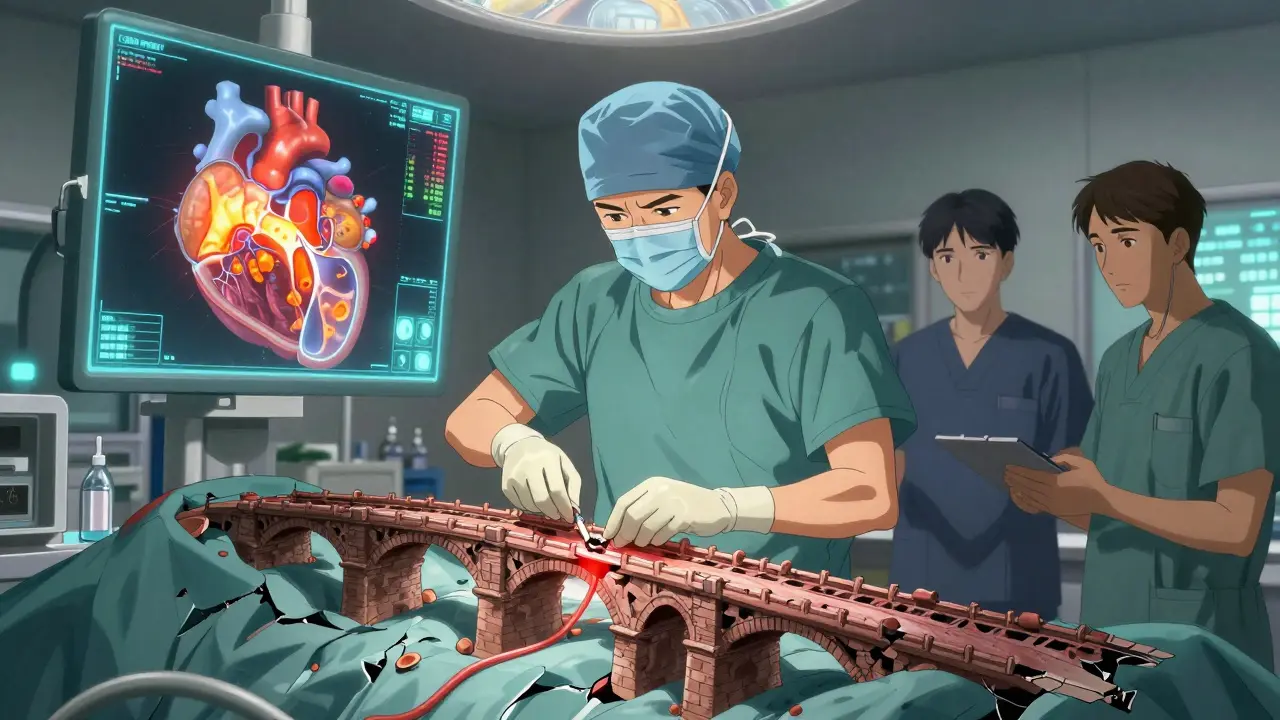
- Percutaneous coronary intervention (PCI)-Also called angioplasty. A balloon opens the blockage, and a metal stent holds it open. Quick, effective, and common. But it doesn’t stop disease elsewhere.
- Coronary artery bypass grafting (CABG)-A surgeon takes a healthy blood vessel from your leg or chest and routes it around the blocked artery. Used when multiple arteries are damaged or the left main artery is affected. More serious surgery, but it lasts longer than stents.
There’s no one-size-fits-all. A 68-year-old with diabetes and three blocked arteries needs bypass. A 52-year-old with one moderate blockage might do fine with statins and walking.
The New Frontiers: Personalized Care and Cardio-Oncology
The future of CAD treatment isn’t just about drugs and stents-it’s about personalization. The 2023 guidelines stress that treatment must match your risk level, not just your symptoms.
For example, someone with high-risk features (diabetes, kidney disease, prior heart attack) may need dual therapy: a statin plus a second drug like a PCSK9 inhibitor to drive LDL even lower. Others might benefit from newer anti-inflammatory drugs like colchicine, which reduce plaque inflammation.
And then there’s cardio-oncology. As cancer survival rates rise, more people live long enough to develop heart disease. Chemotherapy, radiation, and targeted drugs can damage the heart. Now, specialists work together to treat both cancer and heart disease at once-monitoring heart function during chemo, adjusting medications, and preventing heart attacks in survivors.
This isn’t science fiction. It’s happening now in hospitals across the UK and US. Your heart and your cancer treatment aren’t separate issues-they’re connected.
What You Can Do Today
If you’re over 40, or have any risk factors, don’t wait for chest pain. Ask your doctor for:
- A full lipid panel (not just total cholesterol)
- Blood pressure check
- Diabetes screening (HbA1c)
- Discussion of your 10-year heart risk using the ACC/AHA calculator
And if you’re already diagnosed? Stick with your meds. Even if you feel fine. The plaques aren’t gone-they’re just being managed. Every day you take your statin, you’re buying yourself more time.



Justin Fauth February 3, 2026
They say atherosclerosis is silent? Nah, it’s screaming - you just don’t wanna hear it until your heart throws a fit. I watched my pops go from ‘I’m fine’ to a stent in 72 hours. No warning. Just a cough and then BAM - ER lights. They treat this like it’s a vitamin deficiency. It’s not. It’s war in your veins.
Meenal Khurana February 5, 2026
Statins save lives. Take them.
Joy Johnston February 6, 2026
This is one of the most accurate summaries of CAD I’ve seen in a public forum. The distinction between stable and unstable plaques is critical - and often misunderstood. The 75% statistic about unstable plaques causing 75% of events is backed by multiple large-scale trials, including the CANTOS and FOURIER studies. Also, the inclusion of SGLT2 inhibitors and GLP-1 agonists in guidelines reflects a paradigm shift: we’re no longer just lowering LDL - we’re targeting inflammation, glucose metabolism, and cardiac remodeling simultaneously. For clinicians, this means individualized risk stratification isn’t optional - it’s mandatory.
Shelby Price February 7, 2026
So… if I eat avocado every day and do yoga, does that mean I’m safe? 😅 I ask because my mom’s on 5 meds and still says she feels ‘fine’ but also says ‘don’t tell Dad I’m on blood thinners.’
Keith Harris February 8, 2026
Oh wow, another ‘statins are magic’ cult post. Let me guess - you also think fluoride in water is a government plot and that your kale smoothie can reverse plaque? Newsflash: arteries don’t care about your Instagram wellness aesthetic. You think you’re ‘preventing’ CAD by drinking bone broth? The only thing that shrinks plaque is a statin + lifestyle that doesn’t involve ‘eating clean’ while binge-watching Netflix. And don’t get me started on ‘natural remedies’ - if your grandpa’s garlic pills worked, we wouldn’t have coronaries in the first place. Wake up.
Mandy Vodak-Marotta February 10, 2026
Okay, so I’m 48, had a weird chest tightness last month during a hike, went to the doc, they did an ECG and said ‘nothing’s wrong’ - but I’m like, ‘but I felt it!’ So I pushed for a stress test and turns out I had a 60% blockage in my LAD. No symptoms before that. No family history. Just… me. And I was told I was ‘low risk’ because my cholesterol was ‘fine.’ Turns out, my CRP was through the roof, my BP was creeping up, and I’ve been sitting on my ass for 20 years. Now I’m walking 5 miles a day, cut out soda, and I’m on a low-dose statin. I didn’t want to believe it - but your body doesn’t lie. If you feel something, even if it’s ‘just’ fatigue or jaw pain or weird indigestion - don’t ignore it. Especially if you’re over 40. This isn’t fearmongering. It’s survival.
rahulkumar maurya February 11, 2026
How quaint. You speak of ‘guidelines’ as if they are divine scripture. The ACC/AHA is a pharmaceutical puppet show. Real medicine doesn’t rely on algorithmic risk calculators - it relies on clinical intuition, pulse diagnosis, and ancient wisdom. In Ayurveda, we’ve understood vata imbalance as the root of arterial rigidity for millennia. No statin can restore dhatus. You medicate symptoms, but the soul remains unhealed. I’ve treated patients with turmeric, ashwagandha, and breathwork - plaque regression in 14 weeks. No stents. No blood thinners. Just discipline. Your modern medicine is a crutch for the spiritually lazy.
Alec Stewart Stewart February 13, 2026
Just wanted to say thank you for writing this. My brother got diagnosed last year at 51 - he thought he was fine because he ‘didn’t smoke.’ But he had diabetes, high BP, and zero exercise. He’s on statins now, walks every morning, and actually sleeps better. It’s scary how quiet this disease is. If you’re reading this and you’re over 40 - get checked. Even if you feel fine. Your future self will thank you. 💪❤️
Geri Rogers February 13, 2026
Okay, I’m calling BS on the ‘you don’t need symptoms’ thing - I’ve been on a statin for 3 years and my doctor just told me my plaque is shrinking. I didn’t even know that was possible. 😱 I used to think ‘heart disease’ meant you’re old and fat - turns out, I was the walking time bomb. Now I eat salmon, walk my dog for 45 minutes every day, and I’m not even mad about it. My mom’s still eating fried chicken, but I’m living proof: it’s never too late. 🙌❤️
Janice Williams February 13, 2026
While the clinical data presented is methodologically sound, the implicit endorsement of pharmacological intervention as the primary modality raises ethical concerns regarding medicalization of normal aging. The conflation of risk stratification with therapeutic necessity, particularly in asymptomatic individuals, constitutes a form of iatrogenic coercion. Moreover, the normalization of lifelong statin therapy without adequate discussion of pleiotropic effects - including myopathy, cognitive dysfunction, and mitochondrial impairment - represents a systemic failure of informed consent. One must question whether this paradigm serves patient autonomy, or merely the financial interests of the lipid-lowering industrial complex.
Jhoantan Moreira February 14, 2026
I love how this post balances science with humanity. My dad had a bypass at 67 - he was a smoker, diabetic, and stubborn as hell. But after the surgery, he started walking with me every morning. We didn’t talk about meds or LDL. We talked about birds, his childhood in Glasgow, and how he missed his wife. He lived 8 more years. Medicine saves lives, but connection keeps them worth living. 🌿❤️
Amit Jain February 16, 2026
My uncle in Delhi had heart attack at 50. No history. Just high BP and stress. He quit chai, started walking, ate roti with dal, and now he’s 70 and plays cricket with grandkids. No stent. No meds. Just simple life. You don’t need fancy tech - just move, eat real food, and sleep well. This is not rocket science. People forget: heart is muscle. It needs work. Not just pills.