Missing a pill isn’t the only way you can lose protection-some medicines and even herbal teas can quietly knock the hormone levels down or turn up your clotting risk.
- Antibiotics like rifampin can cut pill effectiveness by up to 30 %.
- Enzyme inducers such as carbamazepine or efavirenz speed up hormone clearance.
- Strong CYP3A4 inhibitors (ketoconazole) may raise clot‑risk.
- Herbal boosters like St.‑John’s‑Wort reduce contraceptive levels.
- Always use backup birth control when starting or stopping these meds.
Desogestrel‑Ethinyl Estradiol is a combined oral contraceptive that blends desogestrel (a progestin) and ethinyl estradiol (an estrogen) to prevent pregnancy. Understanding desogestrel ethinyl estradiol interactions helps you stay safe.
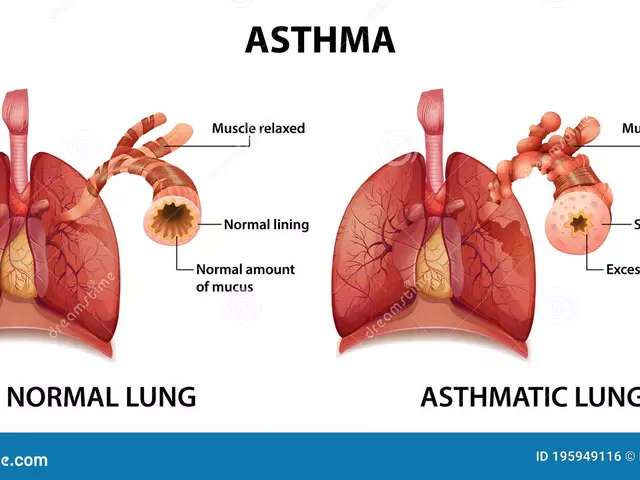
How Desogestrel‑Ethinyl Estradiol Works
Desogestrel blocks the surge of luteinizing hormone, stopping the ovary from releasing an egg. Ethinyl estradiol stabilizes the uterine lining and maintains consistent hormone levels, creating an environment where fertilisation is unlikely.
The Role of CYP3A4 in Hormone Metabolism
CYP3A4 enzyme is a key liver enzyme that breaks down many drugs, including the estrogen component of combined pills. When something speeds up CYP3A4, your hormone levels dip fast; when something blocks it, they can climb too high, raising the risk of blood clots.
Drugs That Reduce Pill Effectiveness
Any medication that cranks up CYP3A4 can shave off a chunk of the estrogen dose you rely on.
Antibiotics are the most talked‑about culprits. Rifampin is an antibiotic used for tuberculosis that strongly induces CYP enzymes, cutting estrogen levels by up to 30 % in some women. Missing that extra dose feels just like a forgotten pill, and the outcome can be an unexpected pregnancy.
Carbamazepine is an anticonvulsant and mood‑stabilizer that also triggers CYP3A4. Women on carbamazepine report a 20 % drop in contraceptive efficacy, so doctors usually recommend a backup barrier method.
Efavirenz is an non‑nucleoside reverse‑transcriptase inhibitor used in HIV therapy that accelerates hormone metabolism. The drug can halve the plasma concentration of ethinyl estradiol, rendering the pill unreliable.
Other enzyme inducers you’ll see in clinic notes include phenobarbital, phenytoin, and high‑dose glucocorticoids. They all turn up the liver’s “speed‑up” gear, so the hormone window narrows and the chance of breakthrough bleeding rises.
Medications That Heighten Blood Clot Risk
Some drugs don’t knock the pill out; they push the estrogen side up, making clots more likely.
Warfarin is an anticoagulant that interferes with vitaminK recycling and can be affected by estrogen levels. When you start a combined pill while on warfarin, the extra estrogen can tip the balance toward clot formation, especially in smokers or women over 35.
Hormone replacement therapy (HRT) for menopausal symptoms adds more estrogen on top of your pill. The cumulative effect can boost clot risk by 1.5‑fold, so many clinicians suggest switching to a progestin‑only pill or an intrauterine device.
Ketoconazole is an potent antifungal that blocks CYP3A4, causing estrogen levels to rise. The spike can aggravate hypertension and raise the chance of deep‑vein thrombosis, particularly in women with a personal or family clot history.
Protease inhibitors such as ritonavir also slam the brakes on CYP3A4, leading to higher estrogen exposure. If you’re on these drugs, your provider may advise a lower‑dose estrogen formulation or a different contraceptive method.

Herbal and Over‑the‑Counter Culprits
People often forget that “natural” doesn’t mean “harmless” for birth control.
St.‑John’s‑Wort is an herbal supplement used for mild depression that strongly induces CYP enzymes. Even a daily dose can shave 15‑20 % off hormone plasma levels, so it behaves like an antibiotic in this context.
Other popular supplements-ginkgo biloba, green‑tea extracts, high‑dose vitaminC-show modest enzyme‑inducing effects in lab studies. While concrete clinical data are scarce, it’s safer to treat them as potential interaction culprits until proven otherwise.
| Medication | Interaction Type | Mechanism | Clinical Recommendation |
|---|---|---|---|
| Rifampin | Reduced effectiveness | Strong CYP3A4 induction | Use backup barrier method; consider alternative contraceptive |
| Carbamazepine | Reduced effectiveness | CYP3A4 induction | Backup contraception; monitor for breakthrough bleeding |
| Efavirenz | Reduced effectiveness | Accelerated estrogen clearance | Backup method; discuss non‑hormonal options |
| Warfarin | Increased clot risk | Estrogen‑mediated clotting factor rise | Close INR monitoring; consider progestin‑only method |
| Ketoconazole | Increased clot risk | CYP3A4 inhibition → estrogen rise | Avoid if possible; use low‑estrogen formulation |
| St.‑John’s‑Wort | Reduced effectiveness | CYP3A4 induction | Backup barrier; discuss herbal discontinuation |
Managing and Preventing Interactions
First, always tell your prescriber every prescription, over‑the‑counter drug, and supplement you take. A quick medication review can spot inducers or inhibitors before they cause trouble.
When you start a known inducer (rifampin, carbamazepine, efavirenz, St.‑John’s‑Wort, etc.), add a reliable backup method-condoms, a diaphragm, or a copper IUD-for at least one full cycle. Once the inducing drug is stopped, keep the backup for another 28 days to let liver enzymes settle.
If you’re on a drug that raises clot risk (warfarin, high‑dose estrogen, ketoconazole), ask your doctor whether a low‑dose estrogen pill, a progestin‑only pill, or a non‑hormonal method better fits your health profile.
For short‑term antibiotics that don’t affect CYP3A4 (amoxicillin, azithromycin, doxycycline), no extra steps are needed. But for any drug that claims “enzyme‑inducing” in the label, treat it as a red flag.
Related Topics You Might Explore
Understanding the pharmacogenomics of oral contraceptives can explain why some women experience breakthrough bleeding while others don’t when on the same drug combo. Also, learning how to counsel patients on “drug‑review appointments” can improve adherence and reduce unintended pregnancies.
Other corners of the same knowledge cluster include “non‑hormonal emergency contraception”, “long‑acting reversible contraceptives (LARCs) and drug interactions”, and “managing hormonal therapy in women with clotting disorders”. These topics build a full picture of safe birth‑control use.
Key Take‑aways
- Enzyme inducers (rifampin, carbamazepine, efavirenz, St.‑John’s‑Wort) can lower hormone levels-use backup protection.
- Strong CYP3A4 inhibitors (ketoconazole, ritonavir) raise estrogen levels-watch for clot risk.
- Anticoagulants and HRT amplify clot potential-consider progestin‑only options.
- Always share a complete medication list with any prescriber.
- When in doubt, switch to a copper IUD or a non‑hormonal method for foolproof protection.
Frequently Asked Questions
Can I take a short course of antibiotics without extra contraception?
If the antibiotic does not induce CYP3A4 (for example amoxicillin, azithromycin, or doxycycline), you can continue using your pill as usual. Only enzyme‑inducing antibiotics like rifampin, griseofulvin, or certain antitubercular drugs require a backup method.
What should I do if I’m prescribed carbamazepine for epilepsy?
Tell your neurologist you’re on a combined oral contraceptive. The safest move is to add a barrier method (condom or diaphragm) for at least one month after starting carbamazepine, then re‑evaluate whether a non‑hormonal or progestin‑only method fits better.
Is St.‑John’s‑Wort really that risky?
Yes. Clinical studies show that daily St.‑John’s‑Wort can lower ethinyl estradiol levels by 15‑20 %. If you don’t want to stop the herb, use a backup contraceptive or switch to a method not affected by enzyme induction, such as a copper IUD.
My doctor wants to start me on ketoconazole for a fungal infection-do I need to change my birth control?
Ketoconazole blocks CYP3A4, causing estrogen levels to rise and increasing clot risk. Discuss with your doctor the possibility of switching to a low‑dose estrogen pill, a progestin‑only option, or a non‑hormonal method while you complete the antifungal course.
I’m on warfarin; can I still use the pill?
It’s possible, but it requires close monitoring of your INR (blood clotting measure). Many clinicians prefer a progestin‑only pill or a copper IUD for patients on warfarin to avoid any added clot‑forming influence from estrogen.






Jessica Hakizimana September 21, 2025
Great overview! I love how you broke down the enzyme inducers versus inhibitors in simple terms. It really helps anyone juggling multiple meds to see the big picture. Remember to keep a backup method handy when you start any new prescription – it’s a tiny inconvenience for big peace of mind. Also, sharing your full med list with your doctor can prevent a lot of surprise interactions. If you ever feel unsure, a quick chat with your pharmacist can clear things up fast. Keep spreading this useful info!
peter derks September 29, 2025
Spot on! This is exactly the kind of practical guide patients need. When I coach athletes, I always emphasize the backup barrier method whenever they’re on enzyme‑inducing meds. It’s not just about pregnancy prevention, but also about maintaining hormonal stability for performance. Thanks for laying it out so clearly – I’ll definitely reference this in my next session.
Sarah DeMaranville October 7, 2025
Interesting but overstated.
Edward Leger October 14, 2025
When we consider the balance of CYP3A4 activity, it becomes a dance between induction and inhibition. The subtleties of how each drug shifts that equilibrium are often underappreciated. A deeper look reveals that even modest inducers can cumulatively lower hormone levels over time. Conversely, potent inhibitors may tip the scale toward thrombotic risk. Therefore, personalized monitoring is essential, especially for patients with underlying risk factors. The pharmacy’s role in spotting these nuances cannot be overstated.
Keyla Garcia October 22, 2025
Wow, this really hit home! 😱 I’ve been juggling a flaky IUD and a bunch of supplements, and I never thought St. John’s‑Wort could be a silent sabotage. Your table makes it crystal clear – no more guessing. 🎭 I’m definitely switching to a copper IUD for that extra peace of mind, and I’ll tell all my friends to double‑check their herbal stash. Thanks for the drama‑free facts! 💃
Ismaeel Ishaaq October 29, 2025
First off, kudos for pulling together such a comprehensive list – it’s a lifesaver for anyone trying to navigate the maze of drug‑drug interactions. The way enzyme inducers like rifampin and carbamazepine lean on CYP3A4 is like turning up the volume on a speaker; you end up hearing the silence of reduced hormone levels, which is a scary thought for anyone relying on the pill. On the flip side, strong inhibitors such as ketoconazole slam the brakes, causing estrogen to pile up, and that’s a recipe for clotting nightmares – especially for women who already have risk factors like smoking or a family history of thrombosis. One point that really stands out is the emphasis on backup contraception: the extra barrier method is not just a suggestion but a critical safety net during any transition period. I’ve seen patients who shrugged off the “just a short course” disclaimer, only to face an unexpected pregnancy months later; the stakes are simply too high to gamble. And let’s not overlook the “natural” culprits – St. John’s‑Wort, ginkgo, and even high‑dose vitamin C have been shown in vitro to tweak enzyme activity, meaning we can’t afford to be complacent about supplements. The table you provided is gold – it translates dense pharmacology into a quick‑look reference that any clinician can use on the fly. For those on anticoagulants like warfarin, the interplay with estrogen is a double‑edge sword; monitoring INR becomes non‑negotiable, and many providers wisely pivot to progestin‑only pills or copper IUDs to sidestep added clot risk. Likewise, patients on HRT need a serious conversation about stacking estrogen sources – the hormonal “stack” can easily overshoot safe thresholds. In practice, I always ask patients to bring every pill bottle and supplement container to my office; a thorough med review catches hidden inducers before they cause trouble. Lastly, the reminder that short‑term, non‑inducing antibiotics (amoxicillin, doxycycline) are generally safe is a comforting note amid all the cautions. All in all, this guide is a must‑read for both patients and prescribers alike, and I’ll be sharing it with my entire network.
Jesse Goodman November 6, 2025
Solid info, concise and clear. 👍 Keep a backup method when you start any inducer – it’s simple but effective.
Antara Kumar November 14, 2025
While the science is sound, I find it unnecessary to alarm patients about every herbal supplement. Many of these “interactions” are based on limited in‑vitro data and don’t translate to real‑world risk. Over‑emphasizing can lead to unnecessary anxiety and medication discontinuation.
John Barton November 21, 2025
Oh, sure, because we all have time to read pharmacology textbooks before popping a pill. 🙄 If the drug label says “enzyme inducer,” just use a condom. No need for all this drama.
Achint Patel November 29, 2025
Just to add, the timing of when you stop the inducer matters. Enzyme levels don’t normalize overnight; give it at least a full menstrual cycle before assuming the pill is back to full strength. This avoids a false sense of security.
Lilly Merrill December 6, 2025
Thanks for the balanced approach. It’s helpful to see both the medical perspective and practical tips for everyday life. I’ll definitely share this with friends who are on the pill and juggling other meds.
Charlie Martin December 14, 2025
Good summary, especially the quick reference table.