Stroke Risk Calculator
Your Stroke Risk Assessment
Enter your key health metrics to estimate your stroke risk level based on evidence-based factors.
Your Stroke Risk Assessment
Your Action Plan
Here are the most impactful changes you can make to reduce your stroke risk:
Every year millions of people suffer a stroke, and many of those cases could have been avoided with the right knowledge. Knowing what pushes your brain’s blood vessels over the edge helps you take action before it’s too late. This guide breaks down the key stroke risk factors, shows how they interact, and gives clear steps you can start using today.
What Is a Stroke?
Stroke is a medical emergency that occurs when blood flow to a part of the brain stops or a blood vessel bursts, causing brain cells to die. It can lead to lasting disability or death if not treated immediately. There are two main types: ischemic (caused by a clot) and hemorrhagic (caused by bleeding). Both share the same end result - brain damage - but the triggers and treatments differ.
Non‑Modifiable Risk Factors
These are factors you can’t change, but knowing them helps you gauge your baseline risk.
- Age The odds of stroke double each decade after 55.
- Gender Men have a slightly higher risk earlier in life, while women face higher risk after menopause.
- Family history If a first‑degree relative had a stroke, your risk rises by about 30%.
- Race / Ethnicity African‑American and Hispanic populations experience strokes at higher rates, often at younger ages.
Modifiable Risk Factors
These are the levers you can pull to cut your risk dramatically. The table below groups them for quick reference.
| Factor | Type | Typical Impact |
|---|---|---|
| High blood pressure The single biggest cause of both ischemic and hemorrhagic strokes | Modifiable | Reduces risk by ~40% when controlled |
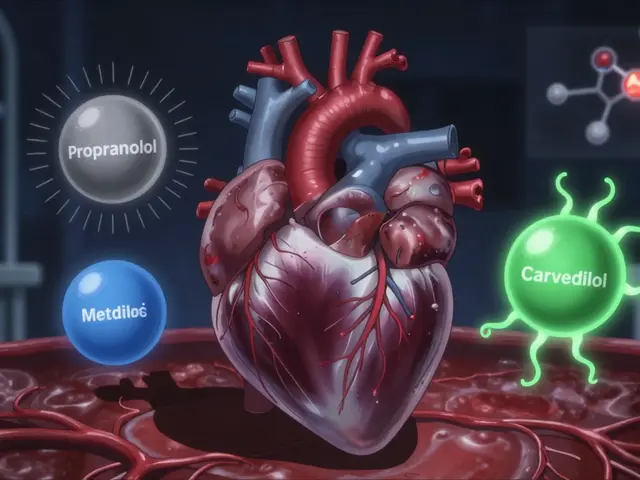
| Atrial fibrillation Irregular heart rhythm that creates clots in the atria | Modifiable (with medication) | Increases stroke risk five‑fold |
| Diabetes High blood sugar damages blood vessels over time | Modifiable (through diet, meds, exercise) | Raises risk by ~30% |
| High cholesterol Leads to plaque buildup and arterial narrowing | Modifiable | Associated with 20‑30% higher risk |
| Smoking Damages vessel walls and promotes clot formation | Modifiable | Current smokers have double the risk |
| Obesity Body‑mass index (BMI) ≥ 30 often co‑exists with hypertension and diabetes | Modifiable | Each 5‑unit BMI increase adds ~15% risk |
| Physical inactivity Lack of exercise worsens blood pressure and lipid profiles | Modifiable | Active people cut risk by up to 30% |
| Unhealthy diet High salt, low fruit/veg intake fuels hypertension and cholesterol spikes | Modifiable | Dietary changes can lower blood pressure by 5‑10 mmHg |
| Excessive alcohol Heavy drinking raises BP and can cause atrial fibrillation | Modifiable | More than 2 drinks/day roughly doubles risk |
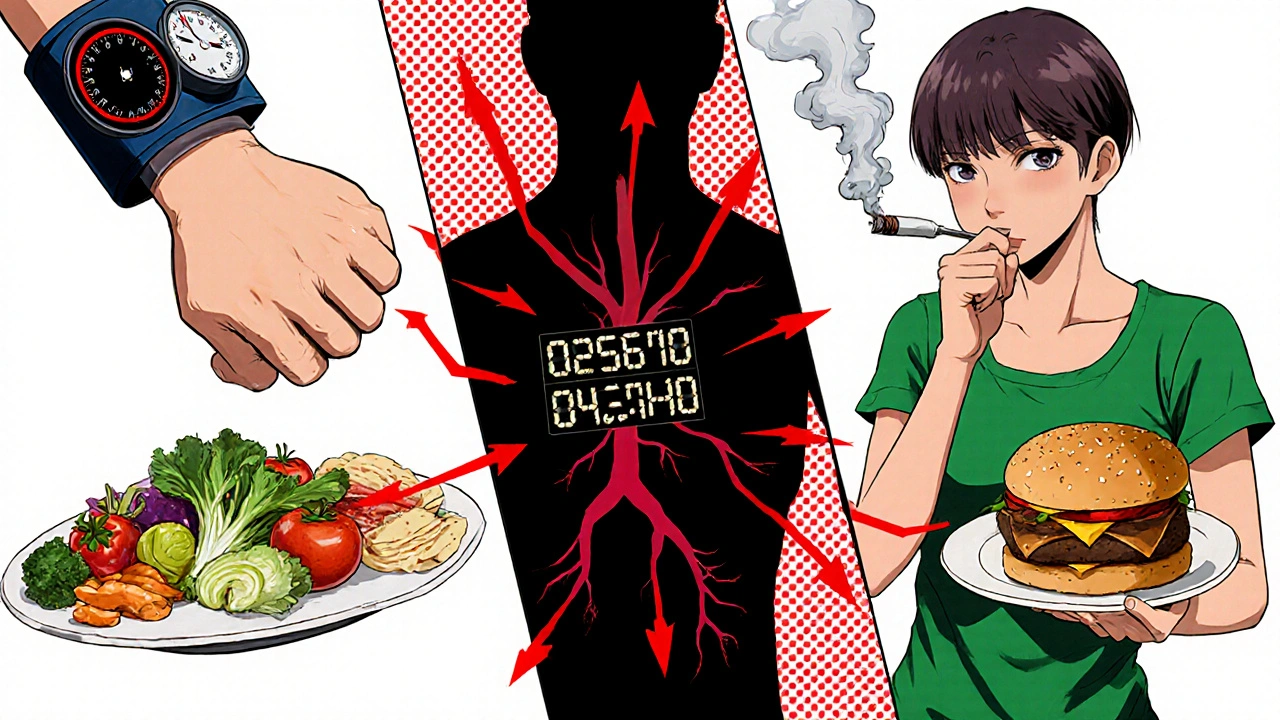
How Risk Factors Interact
Risk isn’t just a sum of individual numbers; the factors often amplify each other. For example, a smoker with high blood pressure is far more likely to suffer a stroke than someone who only has one of those conditions. Tools like the CHA₂DS₂‑VASc score (used for atrial fibrillation) or the Framingham Stroke Risk Profile combine age, blood pressure, diabetes, smoking, and other data to give a personalized percentage.
Assess Your Personal Stroke Risk - A Quick Checklist
- Note your age and gender.
- Measure blood pressure at least twice a year.
- Ask your doctor about heart rhythm - especially if you feel palpitations.
- Check fasting glucose or A1C for diabetes.
- Get a lipid panel to see cholesterol levels.
- Record smoking status and average alcohol intake.
- Calculate BMI (weight ÷ height²) and assess waist circumference.
- Review your diet - look for excess salt, processed foods, and low fruit/veg.
- Track weekly physical activity - aim for at least 150 minutes of moderate exercise.
If you tick more than a few boxes, it’s time to talk to your GP about a formal risk assessment.

Prevention Strategies That Work
Here’s a practical action plan based on the strongest evidence.
- Control blood pressure. Keep it under 130/80 mmHg. Lifestyle changes plus medication when needed are key.
- Treat atrial fibrillation. Anticoagulants (e.g., warfarin, DOACs) cut clot risk dramatically.
- Manage diabetes. Aim for A1C < 7%, combine diet, exercise, and prescribed drugs.
- Lower cholesterol. Statins are proven to reduce stroke by ~20% in high‑risk patients.
- Quit smoking. Use nicotine replacement, counseling, or prescription meds.
- Lose weight. Even a 5‑% drop in body weight improves BP and insulin sensitivity.
- Exercise regularly. Walking, cycling, or swimming for at least 30 minutes most days.
- Eat a heart‑healthy diet. The DASH or Mediterranean patterns-rich in fruits, vegetables, whole grains, nuts, and fish-lower risk.
- Limit alcohol. No more than one drink per day for women, two for men.
These steps don’t guarantee you’ll never have a stroke, but they shrink the odds dramatically.
When to Seek Immediate Help
If you notice the FAST signs-Face drooping, Arm weakness, Speech trouble, Time to call emergency-call 999 right away. Quick treatment can restore blood flow and reduce permanent damage.
Key Takeaways
- Age, gender, family history, and ethnicity set your baseline risk.
- High blood pressure, atrial fibrillation, diabetes, high cholesterol, smoking, obesity, inactivity, poor diet, and excess alcohol are the main modifiable risks.
- Controlling blood pressure and quitting smoking give the biggest reduction in risk.
- Use a checklist or ask your doctor for a personalized risk score.
- Act fast if you see FAST symptoms-every minute counts.
Can a single risk factor cause a stroke?
Rarely. Strokes usually result from a combination of factors. However, uncontrolled high blood pressure alone can be enough to trigger a bleed or clot.
How often should I get my blood pressure checked?
At least once a year if you’re under 40 and healthy. If you have any risk factors, aim for every 3‑6 months or follow your doctor’s advice.
Is atrial fibrillation always symptomatic?
No. Up to one‑third of people with atrial fibrillation feel no symptoms, which is why routine checks are important, especially after age 65.
Can diet alone lower my stroke risk?
A healthy diet greatly reduces risk, but combine it with blood‑pressure control, exercise, and smoking cessation for the biggest effect.
What is the best way to track my progress?
Keep a simple journal: record blood pressure readings, weight, exercise minutes, and diet notes. Review it with your GP every few months.





Don Goodman-Wilson October 22, 2025
Oh great, another checklist that tells you how to avoid a stroke-like we’re all just waiting for a miracle cure.
Newsflash: if you’re over fifty and still think you’re invincible, you’re basically begging for trouble.
Maybe try actually measuring that blood pressure instead of bragging about your ‘American hustle’.
And please, stop pretending that cutting back on salty chips will miraculously erase decades of genetic risk.
Bottom line: you can either keep ignoring the facts or finally start caring about your own health.
Sarah Riley November 2, 2025
The pathophysiological nexus between hypertension and endothelial dysfunction mandates stringent systolic targets.
Empirical data corroborate that incremental reductions in mean arterial pressure translate to proportional decrements in cerebrovascular event probability.
Tammy Sinz November 12, 2025
I totally get how overwhelming it feels to stare at a page packed with risk factor tables and wonder where to even begin.
First, isolate the modifiable variables-blood pressure, diabetes, cholesterol, smoking, obesity, and physical inactivity-because those are the levers you actually control.
Next, conduct a baseline assessment: take two separate blood pressure readings a week apart and log them in a spreadsheet.
If your systolic consistently hovers above 130 mmHg, initiate lifestyle interventions immediately and schedule an antihypertensive work‑up with your physician.
For glucose, aim for an A1C under 7%; if you’re above that, diet modification paired with metformin or other agents can curb microvascular damage.
Statin therapy should be considered whenever LDL exceeds 130 mg/dL, especially if you have concurrent hypertension.
Smoking cessation is non‑negotiable-utilize nicotine replacement, behavioral counseling, or varenicline, because each cigarette roughly doubles your stroke risk.
Weight reduction, even a modest 5 % loss, normalizes insulin sensitivity and alleviates pressure on arterial walls.
Incorporate at least 150 minutes of moderate aerobic activity per week; the evidence shows a 30 % risk reduction in active cohorts.
Adopt a DASH or Mediterranean diet rich in potassium, magnesium, and omega‑3 fatty acids, which synergistically lower both blood pressure and lipid panels.
Limit alcohol intake to no more than one drink per day for women and two for men, as excessive consumption precipitates both hypertension and atrial fibrillation.
Regularly screen for atrial fibrillation, especially after age 65, using either a pulse check or wearable ECG device.
If atrial fibrillation is confirmed, anticoagulation with a DOAC or warfarin is essential to mitigate thromboembolic risk.
Track all these metrics in a simple journal or digital app; review the data with your healthcare provider every three to six months.
By systematically tackling each modifiable factor, you transform a daunting statistic into a manageable, actionable plan.
Christa Wilson November 23, 2025
You've got this! 🎉
Every little change adds up, so celebrate the wins-like choosing a salad over fries.
Remember, consistency beats perfection, and your brain will thank you.
Stay positive and keep moving forward! 😊
John Connolly December 3, 2025
The guide does an excellent job outlining the primary culprits behind cerebrovascular incidents.
From a clinical perspective, tight control of systolic blood pressure remains the cornerstone of primary prevention.
I recommend scheduling quarterly check‑ups to monitor BP, lipid profile, and glucose levels, adjusting therapy as needed.
In addition, enrolling in a structured cardiac rehab or community fitness program can provide accountability.
Implementing these steps not only lowers stroke risk but also improves overall cardiovascular health.
Sajeev Menon December 13, 2025
Hey frinds, great post-really covers all the bases.
I would add that regular yoga can help lower stress, which indirectly keeps blood pressure in check.
Don’t forget to check your waist circumference; it’s a quick indicator of visceral fat.
Stay safe and keep sharing such informativ stuff!
Emma Parker December 24, 2025
Lol, I’m not a doctor but I tried the DASH diet and actually felt more energetic after a week.
Also, my cousin’s boyfriend swears by intermittent fasting for blood pressure-maybe give it a shot?
Anyway, hope you’re not too scared of the numbers, just take it one step at a time!
Joe Waldron January 3, 2026
The article correctly emphasizes that hypertension is the single most important modifiable risk factor, and for that reason, it deserves primary focus.
Moreover, the interplay between diabetes, dyslipidemia, and sedentary lifestyle creates a synergistic effect, amplifying stroke probability beyond the simple sum of individual risks.
Patients should aim for a systolic pressure below 130 mmHg, an LDL cholesterol under 100 mg/dL, and at least 150 minutes of moderate‑intensity aerobic activity per week.
Regular monitoring-whether via home cuff, glucometer, or lipid panel-provides actionable data, enabling timely therapeutic adjustments.
Finally, clinicians must educate patients on the FAST mnemonic, because early recognition dramatically improves outcomes.
Wade Grindle January 14, 2026
Interesting read; the balance between non‑modifiable and modifiable factors is well presented.
I appreciate the practical checklist-it makes self‑assessment feel less daunting.
Overall, a solid resource for anyone looking to proactively manage stroke risk.
Benedict Posadas January 24, 2026
Wow, this guide is lit! 🔥
Start small-swap soda for water, walk 10 mins extra each day, and you’ll see change fast. 😊
Don’t let the big numbers scare you; every healthy habit stacks up, like Lego bricks! 😎
Keep it up, you got this! 💪
Sameer Khan February 3, 2026
From a philosophical standpoint, the delineation between deterministic genetic predispositions and contingent lifestyle choices underscores the agency inherent in human health.
The exposition adeptly integrates epidemiological evidence with clinical praxis, fostering a holistic risk stratification paradigm.
In particular, the emphasis on the CHA₂DS₂‑VASc and Framingham scores illustrates the utility of quantitative models in guiding therapeutic decision‑making.
Nevertheless, one must remain cognizant of the socio‑economic determinants that modulate access to preventive interventions.
Thus, while individual comportment is paramount, systemic support structures are essential to actualize the envisioned reduction in cerebrovascular morbidity.