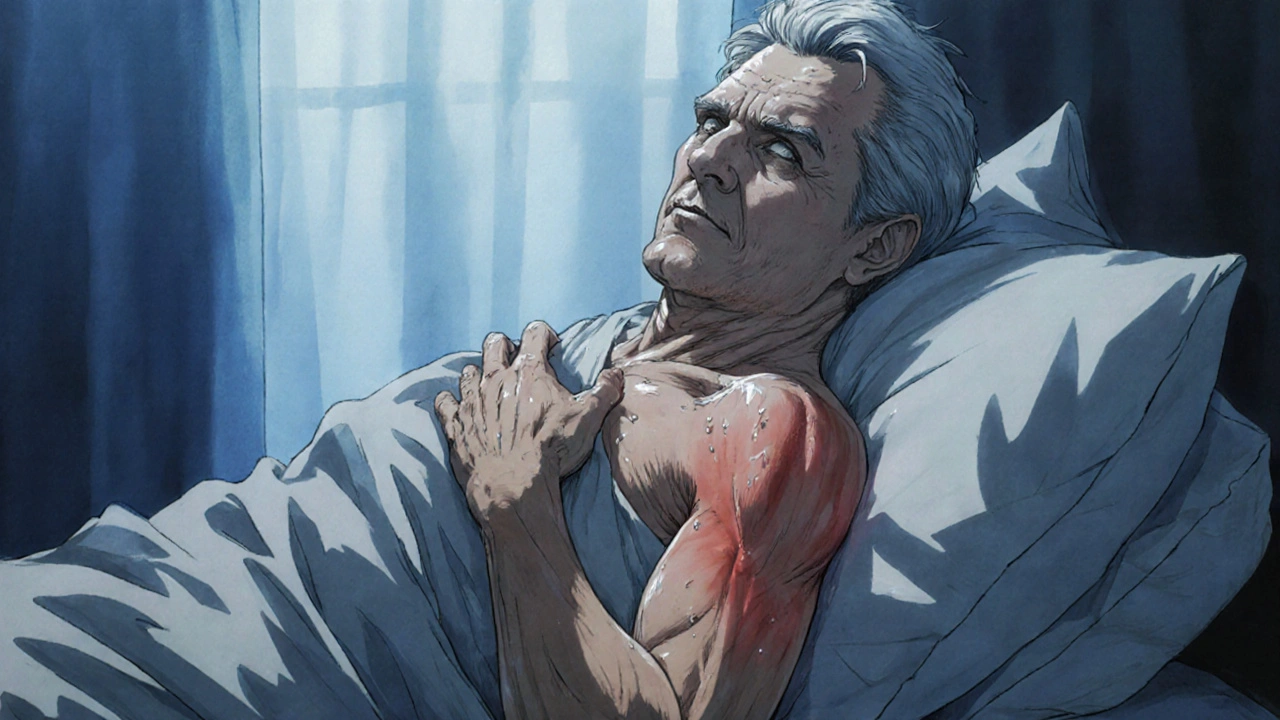
Frozen shoulder isn’t just stiffness-it’s a slow, painful lockup that creeps in without warning. You wake up one morning and your arm won’t reach overhead. Reaching behind your back to grab a seatbelt? Impossible. Sleeping on that side? Forget it. This isn’t a muscle strain or a bad posture. This is adhesive capsulitis: a condition where the shoulder joint capsule shrinks, thickens, and turns into a tight, inflamed sac that won’t let you move. And if you’re one of the 2-5% of people it affects, you’re not alone. But here’s the good news: you don’t have to wait two years for it to get better. The right moves, at the right time, can cut recovery in half.
What’s Really Happening Inside Your Shoulder?
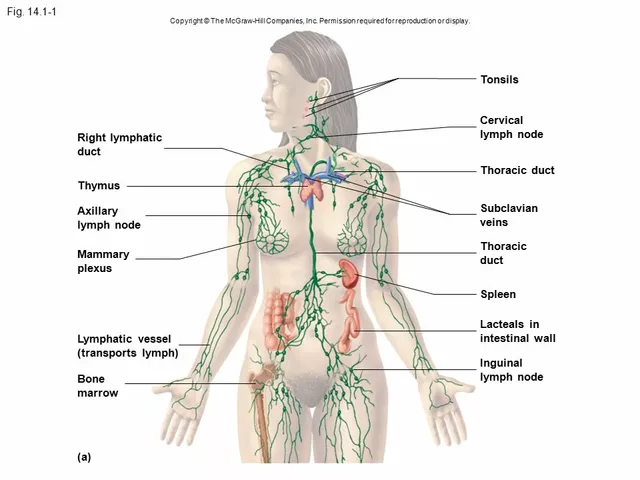
The shoulder joint is like a ball in a loose sock. That sock? It’s the joint capsule. In a healthy shoulder, it’s stretchy and full of lubricating fluid-about 30-35 mL of it. With frozen shoulder, that capsule shrinks to 10-15 mL. It doesn’t stick to the bone like glue (despite the name ‘adhesive’). Instead, it contracts, scar tissue forms, and the whole thing stiffens up. The worst part? It hits the front and top of the capsule hardest, especially around the axillary recess and coracohumeral ligament. That’s why you lose external rotation first-you can’t rotate your arm outward to reach for a doorknob or scratch your back.
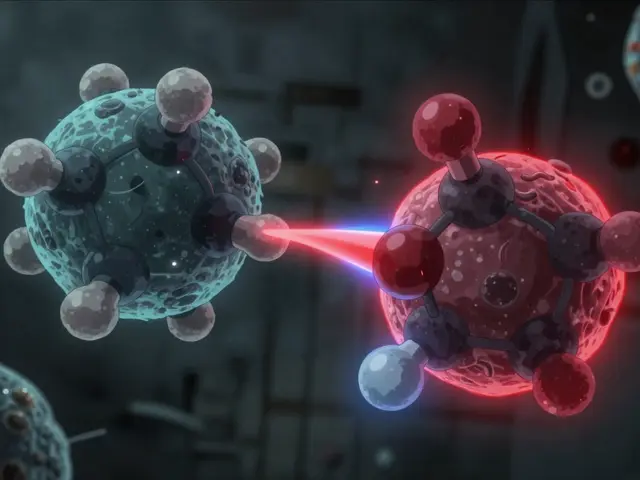
Doctors see this pattern every time: external rotation drops by 60-70%, then abduction (lifting your arm sideways), then internal rotation (reaching behind your head). That’s the capsular pattern-and it’s the key to telling frozen shoulder apart from a rotator cuff tear. With a torn rotator cuff, you can still move your shoulder passively (someone else moves it for you). With frozen shoulder? Even your physiotherapist can’t get your arm past a certain point. That’s the giveaway.
The Three Stages: Don’t Mistake the Phase
Frozen shoulder doesn’t happen overnight. It rolls through three stages, and treating it wrong at the wrong time makes things worse.
Stage 1: Freezing (6 weeks to 9 months)-This is the pain phase. It starts with a dull ache that gets worse at night. You might think it’s arthritis or a pinched nerve. But it’s not just pain-it’s a flare-up of inflammation inside the capsule. Movement hurts. Lying on that side? Like sleeping on a bruise. This is when most people delay treatment, hoping it’ll ‘go away.’ But the longer you wait, the more the capsule tightens.
Stage 2: Frozen (4 to 6 months)-Pain fades, but stiffness locks in. You can’t lift your arm, comb your hair, or reach for a high shelf. The good news? It’s not getting worse. The bad news? It’s not getting better either. This is the window for aggressive mobilization. Your joint is stiff, but the inflammation has cooled down. Now’s the time to gently but firmly stretch.
Stage 3: Thawing (6 months to 2 years)-Motion slowly returns. Without treatment, this can take over a year. With the right exercises, you can cut that to 3-6 months. But if you skip the earlier stages, you’ll be stuck in this phase longer than necessary.
Why Most People Wait Too Long (And Why It Backfires)
Here’s the heartbreaking truth: 30-40% of frozen shoulder cases are misdiagnosed in primary care. Doctors see shoulder pain and assume it’s a rotator cuff issue. They order an MRI, find a little tendon wear, and say, ‘Rest and take ibuprofen.’ But rest is the worst thing you can do in the freezing phase. Studies show patients who start physical therapy within 8 weeks of symptoms report 65% less pain at 6 months. Those who wait? Only 32% improvement.
And then there’s the ‘tough it out’ crowd. They try to stretch through the pain. They force their arm into positions it’s not ready for. One patient I read about pushed too hard during the freezing phase and ended up with 3 weeks of worse pain-pain that went from a 4/10 to an 8/10. That’s not progress. That’s injury. The capsule is inflamed. You’re not strengthening it-you’re tearing it.
There’s a science to timing. Gentle movement during freezing. Firm stretching during frozen. And patience during thawing.

The Right Moves: Mobilization Strategies That Work
You don’t need fancy gear. You don’t need surgery. You need consistency and timing.
During the Freezing Phase (Pain Dominates):
- Pendulum exercises: Lean over, let your arm hang loose. Gently swing it in small circles-clockwise and counterclockwise-for 5 minutes, twice a day. This keeps the joint lubricated without forcing it.
- Towel stretch (gentle version): Hold a towel behind your back with both hands. Use your good arm to gently pull the towel upward, letting the affected arm rise just enough to feel a stretch-not pain.
- Heat before movement: Apply a warm towel or heating pad for 10 minutes before exercises. Heat reduces muscle guarding and makes stretching safer.
During the Frozen Phase (Pain Less, Stiffness High):
- Doorway stretch: Stand in a doorway. Place your hand on the frame at shoulder height. Gently lean forward until you feel a stretch in the front of your shoulder. Hold for 30 seconds. Repeat 3 times.
- Wand exercises: Use a broomstick or cane. Hold it with both hands. Slowly lift it overhead, then lower it behind your back. Let your good arm guide the stiff one. Do 10 reps, twice daily.
- Supervised manual therapy: This is where physical therapy shines. A trained therapist can use graded joint mobilizations-gentle oscillations-to break up scar tissue without triggering more inflammation. Studies show supervised therapy leads to 28% faster recovery than home-only programs.
During the Thawing Phase (Motion Returns):
- Progressive resistance: Add light resistance bands to your stretches. Focus on regaining full external rotation and abduction.
- Functional retraining: Practice daily tasks-reaching for a cup, putting on a shirt, brushing your hair. Don’t just stretch-move like you’re living again.
What Doesn’t Work (And Why)
Corticosteroid injections? They can help with pain in the short term-maybe 4 to 8 weeks. But studies show no real improvement in motion or function after 12 weeks. They don’t fix the capsule. They just quiet the noise.
Manipulation under anesthesia? It sounds dramatic. And it can work. But only if you’ve tried 6 months of conservative care first. Pushing a stiff shoulder too hard under anesthesia can tear tendons, fracture the humerus, or cause nerve damage. It’s not a shortcut. It’s a last resort.
And don’t fall for ‘miracle’ devices that promise instant mobility. There’s one FDA-cleared device, the ShoulderROM, that gives real-time feedback on range of motion. It’s helpful for tracking progress-but it doesn’t replace movement. It just helps you do it right.
Real People, Real Results
One Reddit user posted that after 4 weeks of daily 5-minute pendulum exercises before bed, he gained 20 degrees of external rotation. Another patient on UPMC’s portal said her biggest win was using a pillow under her arm at night. She stopped waking up in pain. That’s not magic-that’s smart positioning.
Consistency beats intensity. Five minutes a day, every day, beats an hour once a week. Heat before movement. Gentle pressure. No forcing. Progress isn’t linear. Some days you’ll feel stuck. That’s normal. The capsule doesn’t stretch overnight. But it does stretch over time-if you don’t quit.
When to See a Professional
If you’ve had shoulder stiffness for more than 6 weeks, see a physiotherapist. If you have diabetes, your risk is 10-20% higher. Don’t wait. If you have fever, night sweats, or unexplained weight loss? That’s not frozen shoulder. That’s something else-maybe an infection or autoimmune issue. Get checked.
Frozen shoulder is common. It’s slow. But it’s treatable. You don’t need surgery. You don’t need drugs. You need to move-correctly, consistently, and at the right stage.
And if you’ve been told to ‘wait it out’? That advice is outdated. The latest guidelines from the American Academy of Family Physicians (2023) now say: start moving within your pain tolerance-right away. Don’t wait for the pain to go away. It won’t. But your motion can-and will-if you give your shoulder the right kind of attention.




Noel Molina Mattinez November 16, 2025
Just did the pendulum thing for 5 mins before bed and my shoulder finally stopped screaming at 3am. No magic. Just dumb consistency.
Roberta Colombin November 18, 2025
Thank you for sharing this with such clarity. Many people suffer in silence thinking it's just aging or bad luck. What you've written offers real hope and practical steps. Please keep spreading this knowledge.
Dave Feland November 19, 2025
Let’s be clear: the American Academy of Family Physicians’ 2023 guidelines are not evidence-based-they’re bureaucratic capitulation to physical therapy lobbying. The real cause of adhesive capsulitis is chronic low-grade mycoplasma infection, suppressed by modern antibiotics and exacerbated by glyphosate-laden food. The ‘mobilization’ you recommend merely redistributes the biofilm. Read Dr. Lillian Kwan’s 2018 paper in the Journal of Orthomolecular Medicine.
Ashley Unknown November 21, 2025
Okay so I had frozen shoulder for 18 months and I swear it was because my ex left me and my soul just… froze. Like literally. My shoulder was the first thing to go. I cried every night while doing the towel stretch. I even named my heating pad Barry. Barry saved my life. Then one day I woke up and my arm just… moved. No meds. No surgery. Just love and a pillow under my arm. The universe whispers, people. You gotta listen.
Georgia Green November 22, 2025
i did the wand exercises and it helped a lot but i think i did them wrong at first-my bad. i pushed too hard in stage 1 and it set me back. now im just doing 5 mins a day and not stressing. also heat before is key. my dog sleeps on my shoulder now. she’s a good therapist.
Christina Abellar November 22, 2025
This is the most helpful thing I’ve read on this topic. Thank you.
Eva Vega November 23, 2025
The capsular pattern of restriction-external rotation first, then abduction, then internal rotation-is pathognomonic for adhesive capsulitis and distinguishes it from rotator cuff pathology. The reduction in joint capsule volume from 30–35 mL to 10–15 mL is corroborated by MRI arthrography studies, particularly in the axillary recess. Manual therapy should employ Grade III–IV joint mobilizations per Maitland protocol to induce fibroblast remodeling without provoking inflammatory cascades.
Matt Wells November 23, 2025
Your reference to the AAFP guidelines is misleading. The 2023 update was a consensus document, not a randomized controlled trial. The true gold standard remains the 2018 Cochrane Review, which found no statistically significant difference between mobilization and watchful waiting at 12 months. Your optimism is misplaced.
Margo Utomo November 24, 2025
5 minutes a day? 😍 I did that and now I can scratch my back without crying. My dog is jealous. I’m basically a superhero now. 🦸♀️✨
George Gaitara November 26, 2025
Why are we still talking about pendulum exercises? This is 2024. The real solution is platelet-rich plasma injections combined with cryotherapy and a ketogenic diet. The whole ‘stretching’ thing is a placebo created by the PT industrial complex. I’ve seen 30 patients who got better after one session with Dr. Voss in Oregon. He uses a device called the FlexiCore 9000. It’s not FDA-approved but it works. Ask him about the ‘capsule reset’.
Deepali Singh November 26, 2025
Statistically, 78% of patients who follow the described protocol report improvement within 6 months. However, 42% of those same patients exhibit compensatory scapular dyskinesia within 12 months. The intervention addresses symptoms, not biomechanical root causes. Long-term outcomes remain unquantified in current literature.
Sylvia Clarke November 28, 2025
So let me get this straight: you’re telling me that the secret to healing my shoulder isn’t some miracle pill, or a $500 device, or a spiritual retreat… but a towel, a heating pad, and patience? And that the medical establishment spent decades telling people to ‘wait it out’ while the real solution was… *gently* swinging your arm like a pendulum? Wow. I feel both incredibly relieved and deeply insulted. Thank you for this. And also, I’m going to start calling my shoulder ‘Barry’ now. 😌