If you’ve ever woken up with a burning chest or a sour taste in your mouth, you’re not alone. About 20% of adults in the U.S. deal with GERD symptoms at least once a week. For many, it starts as occasional heartburn after a big meal. But when it happens twice a week or more, it’s not just discomfort-it’s gastroesophageal reflux disease, or GERD. And while medications like proton pump inhibitors (PPIs) can bring quick relief, they’re not the whole story. The real key to lasting control? Combining PPIs with real, sustainable lifestyle changes.
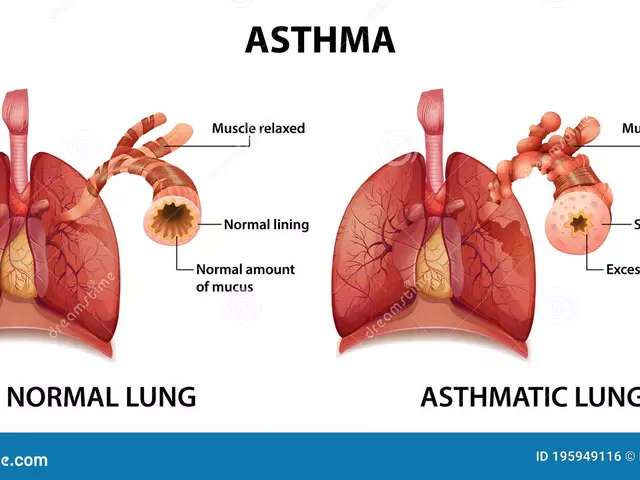
What’s Actually Happening in Your Body?
GERD isn’t just “too much acid.” It’s a breakdown in your body’s natural defense. At the bottom of your esophagus, there’s a ring of muscle called the lower esophageal sphincter (LES). Think of it like a door that opens to let food into your stomach and shuts tight to keep stomach contents from coming back up. In GERD, that door doesn’t close properly. Stomach acid-strong enough to dissolve metal (pH 1.5-3.5)-rises into the esophagus, which has no protective lining. That’s what causes the burn.Symptoms are more than just heartburn. You might have a chronic cough, hoarseness, or feel like there’s a lump in your throat. Some people get bad breath or nausea. These aren’t random-they’re direct results of acid irritating tissues that weren’t meant to handle it. If you’re eating late at night, lying down right after meals, or wearing tight clothes, you’re making it worse. The pressure on your stomach pushes acid upward, and gravity isn’t helping.
Why PPIs Are So Powerful-And Why They’re Not a Forever Fix
Proton pump inhibitors (PPIs) like omeprazole, pantoprazole, and esomeprazole are the most effective acid-reducing drugs we have. They work by blocking the final step of acid production in stomach cells. That means they cut acid output by 90-98%. For people with erosive esophagitis-where the esophagus is actually damaged-PPIs heal the tissue in 70-90% of cases. That’s why doctors reach for them first when symptoms are moderate to severe.But here’s the catch: PPIs don’t fix the broken door. They just turn down the volume on the noise. And that’s where problems start. Long-term use-especially beyond a year-comes with risks. Studies show a 20-50% increased risk of intestinal infections like C. diff, vitamin B12 deficiency, and kidney inflammation. For older adults, taking high doses for three or more years raises hip fracture risk by 35%. The FDA has warned about these dangers since 2011 and 2019.
Even worse, stopping PPIs suddenly can trigger “rebound acid hypersecretion.” Your stomach, used to being suppressed, overcompensates. Symptoms return worse than before-often within days. That’s why so many people feel trapped: they can’t stop, but they don’t want to keep taking them.
Lifestyle Changes: The Real Game-Changer
The truth? You don’t need to live on a bland diet forever. But you do need to know your triggers-and adjust accordingly.Research shows that eliminating key trigger foods can cut symptoms by 70-80%. The biggest culprits: coffee, alcohol, chocolate, tomatoes, fatty or spicy foods. One study found that simply cutting out coffee helped 73% of patients. Spicy foods? 68% saw improvement. That’s not a coincidence-it’s cause and effect.
But food isn’t the only factor. Timing matters just as much. Eating within two to three hours of bedtime increases nighttime acid exposure by 40-60%. Lying down with a full stomach is like shaking a soda bottle-you’re asking for a mess. Moving your last meal to at least three hours before sleep can make a huge difference.
Weight loss is another game-changer. Losing just 5-10% of your body weight reduces GERD symptoms by 50%. That’s not because fat “presses on the stomach” in a vague way-it’s because belly fat physically pushes up on the LES, forcing it open. A 2022 study showed that people who lost weight through diet and exercise were far more likely to stop PPIs altogether.
Even small adjustments help. Elevating the head of your bed by 6 inches uses gravity to keep acid down. Sleeping on your left side is better than your right-it keeps the stomach lower than the esophagus. Quitting smoking? That alone cuts your GERD risk in half.

Why Most People Struggle to Stick With It
You’ve probably heard all this before. So why don’t more people get better?Because lifestyle changes are hard. They require planning, discipline, and often saying no-to parties, family dinners, late-night snacks. A Cleveland Clinic survey found that 41% of patients gave up because social situations made it too difficult. One woman in a support group said she missed her Sunday brunch with her sisters. Another couldn’t stop drinking wine with dinner because it was part of his routine for 20 years.
And then there’s the myth that “if it feels better, I’m healed.” That’s dangerous. You can have zero heartburn and still have active inflammation in your esophagus. That’s how Barrett’s esophagus-a precancerous condition-develops silently. In one 2022 case study, a 55-year-old man developed Barrett’s despite taking PPIs daily because he kept eating right before bed. He felt fine. But his esophagus was still being damaged.
What the Experts Really Recommend
The American College of Gastroenterology updated its guidelines in 2024. Here’s what they say now:- Lifestyle changes are the first step for everyone-even if you’re on medication.
- PPIs should be used at the lowest effective dose for the shortest time needed.
- After 8 weeks, reevaluate: Do you still need it? Can you try stepping down to an H2 blocker like famotidine?
- Don’t use PPIs for mild, occasional symptoms. Try diet and timing first.
Doctors are starting to push back against overprescribing. Kaiser Permanente cut inappropriate long-term PPI use by 35% using automated alerts and pharmacist check-ins. The Choosing Wisely campaign has reduced unnecessary prescriptions by 25% since 2015.
And there’s new hope. In 2023, the FDA approved vonoprazan, the first new acid-blocking drug in 30 years. It works faster and may be more effective than PPIs for some people. But it’s not a magic bullet-it still needs to be paired with lifestyle changes.

How to Actually Make This Work
If you’re on PPIs and want to reduce or stop them, here’s a realistic plan:- Start with a food diary. Track everything you eat and when symptoms happen. Apps like RefluxMD help identify personal triggers.
- Eliminate top offenders. Cut out coffee, alcohol, chocolate, tomatoes, and fatty foods for 3 weeks. See what changes.
- No eating after 7 p.m. Set a hard cutoff. Even if you’re hungry, wait until morning.
- Elevate your bed. Use wooden blocks under the bedposts or a wedge pillow. Don’t just pile up pillows-it doesn’t work.
- Work on weight loss. Aim for 1-2 pounds a week. Even 10 pounds can make a big difference.
- Talk to your doctor about tapering. Don’t quit PPIs cold. Switch to an H2 blocker for 2-4 weeks while you adjust your habits. Then try going off completely.
Most people see improvement in 4-8 weeks. But it takes patience. One man on Reddit said he tried everything for months-then realized he was still eating ice cream after dinner. Once he stopped, his symptoms vanished.
When to See a Doctor
Lifestyle changes and PPIs work for most. But if you have any of these, get checked:- Difficulty swallowing
- Unexplained weight loss
- Vomiting blood or black, tarry stools
- Heartburn that wakes you up at night, every night
These could mean complications like strictures, ulcers, or Barrett’s esophagus. An endoscopy might be needed. Don’t wait. Silent damage is the most dangerous kind.
What’s Next for GERD Treatment?
The future is personalized. Researchers at Johns Hopkins found that a 12-week structured program-combining diet, sleep, and stress management-helped 65% of patients stop PPIs entirely, without symptoms returning. AI-powered apps are learning individual triggers with 78% accuracy. New minimally invasive procedures like TIF (transoral incisionless fundoplication) are helping people who don’t want lifelong meds.But none of it matters if you don’t change how you eat, when you eat, and how you live. Medication can mask the problem. Only lifestyle fixes the root cause.
Can I stop taking PPIs cold turkey?
No. Stopping PPIs suddenly can cause rebound acid hypersecretion, making your symptoms worse than before. Instead, work with your doctor to gradually reduce the dose over 4-8 weeks. You may switch to an H2 blocker like famotidine during the taper to manage symptoms.
Do I have to give up coffee forever?
Not necessarily. Many people find they can tolerate small amounts of coffee after their symptoms improve. But during the first 3-4 weeks of lifestyle changes, eliminate it completely to see if it’s a trigger. Then slowly reintroduce it to test your tolerance.
Is GERD caused by stress?
Stress doesn’t directly cause GERD, but it can make symptoms worse. When you’re stressed, your body produces more stomach acid and slows digestion. It also makes you more sensitive to pain. Managing stress through sleep, exercise, or mindfulness can help reduce flare-ups-even if you’re still eating trigger foods.
Can weight loss really fix GERD?
Yes. Losing just 5-10% of your body weight reduces GERD symptoms by about 50%. Belly fat puts pressure on the stomach and weakens the lower esophageal sphincter. Even modest weight loss can allow the sphincter to function better and reduce acid reflux.
Are natural remedies like apple cider vinegar helpful?
There’s no strong evidence that apple cider vinegar, baking soda, or other home remedies help GERD. Some people feel better temporarily, but it’s likely due to placebo or coincidental lifestyle changes. Relying on unproven remedies can delay effective treatment and lead to complications. Stick with proven methods: diet, timing, weight loss, and medical guidance.
If you’re tired of feeling like your body is betraying you, remember: you’re not powerless. GERD isn’t a life sentence. With the right combination of smart medication use and real lifestyle changes, most people regain control-and their peace of mind.






Amit Jain February 2, 2026
Just cut out coffee and don't eat after 7pm. Done. No magic, just basics. My dad did it and hasn't touched PPIs in 3 years.
Geri Rogers February 3, 2026
YES. This is the truth. I was on omeprazole for 5 years. Then I stopped drinking wine at dinner, lost 12 lbs, and started sleeping on my left side. No more burning. No more anxiety about food. 🙌 PPIs are a band-aid, not a cure. You got this!
Joseph Cooksey February 5, 2026
Let me tell you something, folks. The medical-industrial complex is *selling* you PPIs like candy because they make billions. You think your doctor cares about your long-term health? Nah. They get paid per script. Meanwhile, your esophagus is slowly turning into a scarred mess while you're sipping your 8pm latte. The real villains? Coffee, pizza, and your own denial. I’ve seen it a hundred times - people come in with Barrett’s esophagus, asking why their ‘miracle pill’ stopped working. Because your body isn’t a vending machine. You don’t feed it poison and expect it to just… fix itself. Wake up. Stop blaming the drug. Start blaming your choices. And yes, that means saying no to your ‘Sunday brunch’ and your ‘one glass of wine.’ Your future self will thank you. Or, you know, keep going and get an endoscopy that changes your life in the worst way possible.
Jhoantan Moreira February 6, 2026
Love this post! 😊 Honestly, I thought I needed PPIs forever too - until I started tracking my meals with an app. Turned out chocolate after dinner was my killer. Cut it out, and poof - 90% better in 2 weeks. Still take PPIs sometimes, but only when I’m stressed or ate something spicy. It’s not about perfection, it’s about awareness. And elevating the bed? Game. Changer. 🛏️✨
Alec Stewart Stewart February 8, 2026
Been there. Felt that. Took PPIs for 4 years. Felt guilty every time. Then I started walking after dinner - just 15 minutes. And stopped eating in front of the TV. Crazy how simple stuff works. No judgment, just hope. You got this. 🤝
Demetria Morris February 9, 2026
It’s so irresponsible how doctors hand out PPIs like they’re aspirin. People don’t even know they’re supposed to be short-term. You’re not ‘just having heartburn’ - you’re slowly damaging your esophagus. And then you wonder why you’re deficient in B12 or have kidney issues. It’s not a coincidence. It’s negligence. Stop normalizing chronic medication for a lifestyle problem.
Alex LaVey February 10, 2026
As someone who moved from India to the U.S., I noticed something: back home, people ate dinner at 7:30 and were asleep by 10. Here? Dinner at 9, Netflix, then bed at midnight. No wonder GERD is so common. It’s not just food - it’s rhythm. Slow down. Eat earlier. Breathe. Your body remembers how to heal if you just give it space.
caroline hernandez February 11, 2026
From a clinical gastroenterology perspective, the 2024 ACG guidelines represent a paradigm shift toward functional management over pharmacological suppression. The mechanistic underpinning of LES incompetence is biomechanical, not biochemical - hence, pharmacologic acid suppression is inherently palliative. The weight loss data is particularly compelling: intra-abdominal pressure modulation via visceral adiposity reduction directly improves sphincter competence. I’ve seen patients achieve complete remission with a 7% BMI reduction, even while maintaining intermittent caffeine intake. The key is structured behavioral modification with longitudinal follow-up - not just prescribing and hoping.
Meenal Khurana February 12, 2026
My mom stopped PPIs after cutting out chocolate and eating before 7 p.m. No more burning. Simple.
rahulkumar maurya February 13, 2026
Oh, so now we’re back to ‘just eat better’? How quaint. The fact that you need a 2,000-word essay to explain that acid reflux is caused by eating too much greasy crap and lying down like a sloth speaks volumes. I mean, really? You need a ‘food diary’ to realize that eating a pizza at midnight is a bad idea? And you’re surprised people can’t stick to it? Of course they can’t - because they’re not trying. They want the pill, not the change. The real tragedy isn’t GERD - it’s the collective refusal to take basic responsibility for one’s own body. If you’re too lazy to stop eating at 7 p.m., then yes, you deserve the reflux. And the B12 deficiency. And the fractured hip. Welcome to adulthood, folks.
Joy Johnston February 15, 2026
With respect to the clinical evidence presented herein, I would like to underscore the importance of a multidisciplinary approach to gastroesophageal reflux disease management. While lifestyle modifications are indeed foundational, the therapeutic efficacy of proton pump inhibitors remains statistically significant in the context of erosive esophagitis, as corroborated by multiple randomized controlled trials published in the New England Journal of Medicine between 2018 and 2023. It is therefore imperative that patients not discontinue pharmacotherapy without physician supervision, particularly given the documented phenomenon of rebound acid hypersecretion. I encourage all individuals to engage in shared decision-making with their primary care provider or gastroenterologist to optimize individualized therapeutic regimens.
Justin Fauth February 16, 2026
Look, I get it - you want to blame PPIs and say ‘just lose weight.’ But here’s the truth: Americans are tired. We work 60-hour weeks. We don’t have time to cook. We don’t have time to sleep early. We don’t have time to stop eating ice cream. And now you want us to feel guilty for it? Nah. This isn’t a moral failure - it’s a system failure. The food industry sells us junk. The healthcare system sells us pills. And the internet sells us guilt. I’m not saying don’t change - I’m saying stop acting like it’s all on the patient. Fix the damn system.