Antihistamine Safety Checker
Check your antihistamine safety
Select your antihistamine and job type to see if it's safe for work
Results will appear here after checking
Many people take antihistamines without thinking twice. They grab a pill for sneezing, itchy eyes, or a runny nose and head to work like normal. But what if that pill is quietly making you unsafe on the job? The truth is, not all antihistamines are created equal-and some can turn a routine workday into a serious risk.
Why Some Antihistamines Make You Unsafe
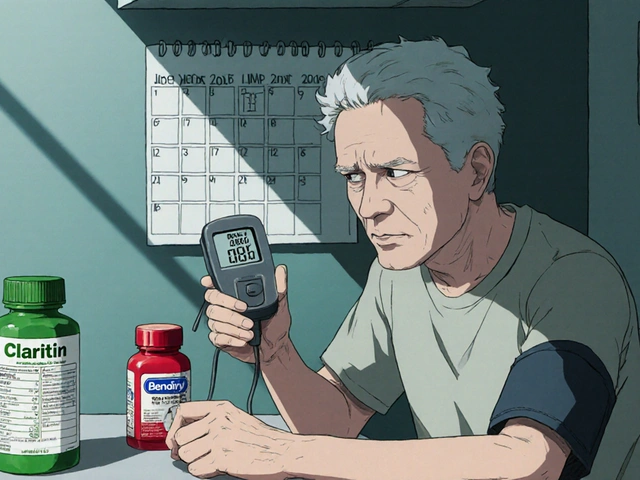
First-generation antihistamines like diphenhydramine (Benadryl), chlorpheniramine (Chlor-Trimeton), and hydroxyzine (Atarax) were developed decades ago to block histamine and relieve allergy symptoms. But they also cross the blood-brain barrier easily. That’s because they’re lipophilic-they dissolve in fat-and don’t get pushed out by the body’s natural defense system, P-glycoprotein. Once inside the brain, they interfere with histamine’s role in keeping you alert. The result? Impaired reaction time, poor coordination, and reduced attention-even if you don’t feel sleepy. Studies show these drugs can slow reaction times by 25-30% and increase lane drifting in driving simulations by up to 50%. That’s not just dangerous behind the wheel. It’s equally risky for someone operating heavy machinery, working at heights, or handling hazardous materials. A truck driver on Reddit once failed a roadside cognitive test after taking Benadryl. He didn’t feel drowsy. But his brain wasn’t working right. That’s the hidden danger: you don’t always know when you’re impaired.The Difference Between Generations
Second-generation antihistamines-like loratadine (Claritin), cetirizine (Zyrtec), and fexofenadine (Allegra)-were designed to fix this problem. They’re built to stay out of the brain. Their chemical structure makes them more likely to bind with P-glycoprotein transporters, which pump them back out before they can affect your central nervous system. The data speaks for itself. In clinical trials, second-generation antihistamines perform almost identically to placebo. No significant drop in reaction time. No increase in errors. One study even tested bilastine, a newer option, at double the normal dose-and still found no measurable impairment in driving tests. Compare that to first-generation drugs, where impairment is consistent and well-documented. The numbers don’t lie. On Healthgrades, 78% of Allegra users report no drowsiness. Only 12% of Benadryl users say the same. That’s not a small difference-it’s a life-or-death gap.Who’s at Risk?
This isn’t just about drivers. Workers in construction, manufacturing, healthcare, aviation, and emergency services are all exposed. Pilots are banned from using first-generation antihistamines by the FAA. The Department of Transportation requires employers in transportation industries to include antihistamine use in safety protocols. And it’s not just because of crashes. Falls are a major concern too. The CDC says more than one in four older adults fall each year. First-generation antihistamines contribute to that. Dizziness, poor balance, slowed reflexes-they all raise the risk of fractures, especially for workers on ladders, scaffolding, or factory floors. One nurse working night shifts switched from diphenhydramine to loratadine and noticed immediate improvement in her alertness during procedures. She still takes it at night, but only because she doesn’t need to be sharp then. Even office workers aren’t immune. Poor concentration affects productivity. Mistakes in data entry, missed deadlines, miscommunication-all can stem from subtle cognitive impairment. Dr. G.G. Kay of Georgetown University called it a hidden cost: “Sedating antihistamines lead to losses in worker productivity and student learning.”
Why People Keep Taking the Risky Ones
If the dangers are so clear, why do so many still use Benadryl or similar drugs? First, they’re cheap and easy to find. You don’t need a prescription. Second, people don’t feel sleepy right away-or sometimes at all. That creates a false sense of safety. A 2022 FDA analysis found that 43% of first-generation antihistamine labels don’t clearly warn about timing or cumulative effects. Many users think, “I took it last night, I’m fine now.” But these drugs have long half-lives-up to 30 hours. Impairment can linger into the next day. Another problem? Mixing them with alcohol or other sedatives. The FDA label on diphenhydramine explicitly warns about this. But people don’t always read labels. Combine even a small amount of alcohol with a first-generation antihistamine, and impairment multiplies. It’s like driving drunk without realizing it.What You Can Do
If you’re taking an antihistamine and your job requires focus, coordination, or quick decision-making, here’s what to do:- Check the label. If it says “may cause drowsiness” or warns against operating machinery, it’s a first-generation drug. Avoid it during work hours.
- Switch to second-generation. Loratadine, cetirizine, and fexofenadine are widely available over the counter. They work just as well for allergies-with far less risk.
- Test it first. If you’ve never taken a new antihistamine, try it at home on a day off. See how you feel after 4, 8, and 12 hours. Don’t assume you’ll react the same as someone else.
- Time it right. If you must take a sedating antihistamine, take it at bedtime. Wait at least 18-24 hours before returning to safety-sensitive tasks. The National Sleep Foundation recommends 24 hours for truck drivers and pilots.
- Talk to your doctor. Don’t just rely on pharmacy advice. Ask: “Is this the safest option for my job?”

Employers and the Changing Landscape
Companies are starting to wake up. As of 2023, 41% of Fortune 500 companies include specific guidance on antihistamines in their occupational health policies. The American Nurses Association found that 73% of nurses now use only non-sedating options. That’s a cultural shift-and it’s spreading. Regulators are catching up too. The FDA updated labeling requirements in March 2023 to make warnings clearer. The European Medicines Agency issued safety alerts for transport workers in 2019. NIOSH launched a 2024 initiative to create workplace guidelines for antihistamine use. The message is becoming unavoidable: if your job puts others at risk, you shouldn’t be taking drugs that dull your mind-even if they’re legal and sold next to cough drops.What’s Next?
The future is moving toward clear separation. First-generation antihistamines will likely be restricted from safety-sensitive roles. Newer options like bilastine, with strong P-glycoprotein affinity and minimal CNS effects, are gaining traction. The American College of Occupational and Environmental Medicine estimates that 23 million American workers regularly use antihistamines. If even half of them switch to safer alternatives, the impact on workplace injuries and accidents could be dramatic. This isn’t about banning medication. It’s about choosing the right tool for the job. You wouldn’t use a hammer to screw in a lightbulb. Why use a drug that makes you drowsy when one that doesn’t is just as effective? Your allergies don’t have to cost you your safety-or someone else’s.Do all antihistamines make you drowsy?
No. Only first-generation antihistamines like diphenhydramine and chlorpheniramine commonly cause drowsiness because they enter the brain. Second-generation antihistamines like loratadine, cetirizine, and fexofenadine are designed to stay out of the central nervous system and typically don’t cause drowsiness. Studies show their performance impact is no different from a placebo.
Can I drive after taking Benadryl if I don’t feel sleepy?
No. Many people who have crashed while using first-generation antihistamines report they didn’t feel sleepy-but their reaction times and coordination were still impaired. The brain’s ability to process information slows down even when you don’t feel tired. Driving under the influence of these drugs is illegal in most states and contributes to an estimated 100,000 crashes per year in the U.S. alone.
How long does drowsiness last after taking a sedating antihistamine?
Peak impairment usually occurs 2-4 hours after taking the drug, but effects can last up to 18 hours due to long half-lives (15-30 hours for drugs like diphenhydramine). Some users report next-day grogginess, even after taking it at night. For safety-sensitive jobs, experts recommend waiting at least 24 hours before returning to duty.
Are second-generation antihistamines safe for all jobs?
Yes, for nearly all roles. Second-generation antihistamines like loratadine and fexofenadine have minimal to no effect on cognitive or psychomotor performance. They’re the preferred choice for truck drivers, pilots, nurses, construction workers, and anyone whose job requires alertness. Studies show they’re as effective as first-generation drugs for allergy relief-with far fewer risks.
Can antihistamines interact with alcohol or other medications?
Yes, and dangerously so. First-generation antihistamines can multiply the effects of alcohol, sleeping pills, painkillers, and muscle relaxants. This combination can lead to severe drowsiness, slowed breathing, or even loss of consciousness. The FDA requires warning labels about these interactions-but many people ignore them. Never mix sedating antihistamines with other depressants.
Is it safe to take antihistamines every day for allergies?
It’s safe to take second-generation antihistamines daily if needed. They’re approved for long-term use and don’t build up in your system the way first-generation ones do. First-generation antihistamines aren’t recommended for daily use because of cumulative side effects: drowsiness, confusion, dry mouth, and increased fall risk. Talk to your doctor about long-term allergy management options.
Why do some doctors still prescribe sedating antihistamines?
Some doctors prescribe them because they’re cheap, familiar, or used to treat insomnia (since drowsiness is a side effect). But awareness is growing. Many now recommend second-generation options first, especially for patients in safety-sensitive jobs. If your doctor prescribes Benadryl for allergies and you work in transportation, construction, or healthcare, ask if a non-sedating alternative is available.
Are there workplace policies about antihistamine use?
Yes. The FAA bans first-generation antihistamines for pilots. The Department of Transportation requires employers in transportation to include them in safety protocols. Many companies now have occupational health policies that either restrict or strongly discourage their use for safety-sensitive roles. Some even provide free access to non-sedating alternatives through workplace clinics.






Todd Nickel January 1, 2026
It's wild how we've normalized this. I used to take Benadryl every night just to sleep, then realized I was zoning out during morning meetings. Not sleepy, just... slow. Like my brain was running on 3G while everyone else had 5G. The studies are clear - it's not about feeling drowsy, it's about your prefrontal cortex getting muted. I switched to loratadine last year. No more accidental typos in reports, no more missing subtle cues in Zoom calls. It’s not glamorous, but it’s the difference between showing up and actually being present.
And honestly? If your job doesn’t have a policy on this, it’s not because it’s not a risk - it’s because nobody’s measured the cost yet. Productivity loss, error rates, near-misses - all invisible until someone gets hurt.
Also, the 30-hour half-life thing? That’s the silent killer. You take it Friday night, feel fine Saturday, show up Sunday morning - and your reaction time is still garbage. No one talks about that.
Stop thinking of it as a pill. Think of it as a cognitive impairment device with a sneeze emoji on the bottle.
Austin Mac-Anabraba January 3, 2026
Let’s be brutally honest - this isn’t about safety. It’s about corporate liability. Companies don’t care if you’re impaired. They care if you get sued. The fact that 41% of Fortune 500 have policies now? That’s not enlightenment. That’s legal departments finally realizing how easy it is to get nailed in court for a worker who took a $5 allergy pill and crashed a forklift.
The real tragedy? The FDA knew this in the 80s. They didn’t ban these drugs because Big Pharma lobbied harder than they lobbied for opioid reform. The same people who sold you Vicodin are now selling you Benadryl as a ‘sleep aid’ and calling it ‘OTC wellness.’
And you? You’re just the disposable cog who thinks you’re being smart because you ‘don’t feel anything.’
Wake up. You’re not a patient. You’re a risk vector.
Phoebe McKenzie January 3, 2026
HOW DARE YOU TELL PEOPLE TO TAKE PILLS JUST BECAUSE THEY’RE ‘SAFER’?!
You think this is about allergies? NO. This is about the pharmaceutical-industrial complex gaslighting us into thinking we can chemically optimize our way out of being human. You want to be ‘alert’? Go drink coffee. Go meditate. Go sleep better. Don’t hand your brain over to Big Pharma’s new ‘non-drowsy’ monoculture.
And who says ‘second-gen’ is safe? Did you read the fine print? Cetirizine causes liver enzyme changes in 1 in 2000. Loratadine? Linked to QT prolongation in rare cases. You think your ‘safe’ pill isn’t quietly wrecking your heart? I’ve seen it. I’ve seen the charts.
They want you to think this is a choice. It’s not. It’s a trap. And you’re falling for it.
Wake up. They’re not fixing your allergies. They’re fixing your compliance.
gerard najera January 4, 2026
First-gen = brain fog. Second-gen = clear head. Pick the latter. Done.
Stephen Gikuma January 5, 2026
They’re pushing this ‘non-drowsy’ stuff because they want you working while they steal your soul. You think the FDA gives a damn? Nah. They’re owned by the same guys who made you buy fluoride in your water and glyphosate in your bread. Benadryl’s been around since 1946. It’s American. It’s patriotic. It’s what your grandpa used.
Now they want you to take some fancy new ‘fexofenadine’ from some lab in Switzerland that’s probably made by Chinese bots?
Wake up. This isn’t science. It’s cultural erasure. They want you docile, quiet, and obedient - not with Benadryl’s sleepy haze, but with their ‘optimal’ chemical regime. You’re being reprogrammed.
And if you take it? You’re part of the problem.
Bobby Collins January 6, 2026
okay but what if you just don't believe in science? like, i mean, i took benadryl for 10 years and i'm still alive and i got promoted so??
maybe my body just doesn't care? maybe the studies are fake? maybe the government is lying to scare us so we buy their expensive pills??
also i heard zyrtec is made from lab rats and i'm not taking that. nope. not happening. i'm sticking with my $3 bottle from walmart. it's got history. it's got soul. 🤷♀️
Layla Anna January 7, 2026
omg i’m so glad someone finally said this 😭
i’m a nurse and i used to take diphenhydramine because it was cheap and my roommate said it worked… then one night i almost dropped a vial of chemo because i couldn’t focus. i didn’t feel sleepy, but my hands were shaking. i cried for an hour after.
i switched to loratadine and my whole life changed. i sleep better, i’m calmer, i don’t zone out during handoffs.
please, if you’re reading this and you’re a nurse, a driver, a teacher, a parent who works - just try it. for one week. you won’t regret it. ❤️
you’re not weak for needing help. you’re brave for choosing safety.
Heather Josey January 9, 2026
This is one of the most important public health messages I’ve seen in years. The normalization of cognitive impairment under the guise of ‘just a little drowsiness’ is a quiet epidemic. We measure workplace injuries, but we don’t measure the invisible cost: the missed diagnosis, the misread chart, the delayed response, the unreported near-miss.
Employers have a duty of care. Employees have a right to be safe. And pharmacists? They need to stop just handing out Benadryl like candy and start asking, ‘What do you do for work?’
I’ve started including antihistamine safety in my employee wellness talks. The response has been overwhelming. People feel seen. They didn’t realize they weren’t alone.
This isn’t about pills. It’s about dignity. About competence. About showing up as your full self - not a half-functioning version drugged into compliance.
Donna Peplinskie January 10, 2026
I’m from Canada, and honestly, I think we’re ahead of you guys here. Our pharmacists are trained to ask about job duties before dispensing any sedating antihistamine. It’s standard practice. We don’t treat health like a supermarket aisle.
My cousin, a construction foreman, used to take Benadryl for his pollen allergies - until he nearly fell off a 20-foot ladder. He didn’t even remember falling. Just woke up in the ER.
Now he takes fexofenadine. Says he feels like he’s ‘back in his own skin.’
It’s not about being ‘perfect.’ It’s about being responsible. And if you’re working in a high-risk job? You owe it to your team to be sharp. Not just legally - morally.
Also, I love that you mentioned bilastine. It’s not available here yet, but I’m lobbying for it. It’s a game-changer.
Olukayode Oguntulu January 11, 2026
Ah, the neoliberal pharmacopeia rears its head once more. You see, the commodification of cognitive optimization under the guise of ‘allergy management’ is merely a symptom of late-stage biopolitical control. The first-generation antihistamines, with their crude lipophilic architecture, were never intended to be therapeutic - they were designed as sociotechnical dampeners, a means of regulating the proletariat’s alertness to maintain productivity thresholds within the capitalist apparatus.
Meanwhile, the second-generation agents, with their P-glycoprotein affinity, represent the aestheticization of safety - a performative gesture of corporate benevolence, masking the deeper epistemic violence of pharmaceutical hegemony.
And yet, the subject, seduced by the illusion of agency, chooses the ‘non-drowsy’ option as if it were a moral victory - when in fact, they are merely internalizing the regime’s preferred mode of compliance.
True liberation lies not in switching pills, but in dismantling the very infrastructure that renders sleeplessness a pathology and rest a luxury.
jaspreet sandhu January 13, 2026
Everyone talks about Benadryl like it’s the devil, but what about the other side? I’ve seen people take Zyrtec and still get drowsy. I work in a warehouse. My buddy took loratadine, thought he was fine, fell asleep on the forklift. They fired him. So now what? You think all these ‘safe’ drugs are magic? No. They’re just different kinds of traps.
People think because it’s called ‘non-drowsy’ it means zero effect. That’s not how biology works. Everyone’s body is different. Some people metabolize fast. Some slow. Some are just naturally sensitive.
And you know what? Maybe you don’t need pills at all. Maybe you just need to stop living in a dusty city and move to the mountains. But no, that’s too hard. So you take a pill instead.
Stop pretending there’s a perfect solution. There isn’t. Just be careful. Always.
Alex Warden January 14, 2026
Let’s cut the BS. This isn’t about safety - it’s about control. They want you to take their expensive pills so you can’t complain when you’re overworked. Benadryl is cheap, American, and gets the job done. You think the government cares if you’re a little slow? Nah. They care if you show up. And if you’re too lazy to handle your allergies without a prescription, maybe you shouldn’t be working a job that matters.
Also, why are we letting foreigners tell us what to take? Bilastine? That’s some EU nonsense. Stick with what works. If you can’t handle a little drowsiness, maybe you’re in the wrong job.
And for the love of God, stop calling this ‘public health.’ It’s just another way to make you feel guilty for being human.
LIZETH DE PACHECO January 14, 2026
I just want to say thank you for writing this. I’m a single mom working two jobs - one as a 911 dispatcher, one as a home health aide. I used to take Benadryl because I was exhausted and thought it would help me sleep. But I’d wake up foggy, miss calls, freeze during emergencies.
I switched to cetirizine. I still take it at night. But now? I’m present. I’m sharp. I’m alive.
This isn’t just about allergies. It’s about being able to show up for the people who need you. And you deserve that.
You’re not weak for needing help. You’re strong for choosing to be safe.
Keep going. You’re doing better than you think.
Todd Nickel January 15, 2026
That’s the thing nobody says - it’s not just about the drug. It’s about the culture that lets us ignore our own impairment. We’ve turned ‘pushing through’ into a virtue. We wear exhaustion like a badge. We call sleepiness ‘weakness.’
But the truth? The most courageous thing you can do is say: ‘I need to be clear-headed to do this job right.’
That’s not weakness. That’s leadership.
And if your boss doesn’t get that? Maybe they’re the one who needs to change - not you.