Breastfeeding is a natural feeding method where a mother provides milk directly from her breasts to her infant, characterized by dynamic immunological components, optimal nutrient ratios, and bioactive enzymes. When a baby receives breast milk, the risk of diaper rash-a painful inflammation of the skin in the diaper area-drops dramatically. This article shows why, how, and what parents can do to harness that protection.
Why Breast Milk Acts Like a Skin Shield
Breast milk isn’t just food; it’s a living fluid packed with lactoferrin, a protein that binds iron and stalls bacterial growth. Studies from the American Academy of Pediatrics (2023) reported a 30% lower incidence of diaper dermatitis in exclusively breastfed infants compared with formula‑fed peers, largely because lactoferrin limits the proliferation of Staphylococcus aureus and Candida albicans.
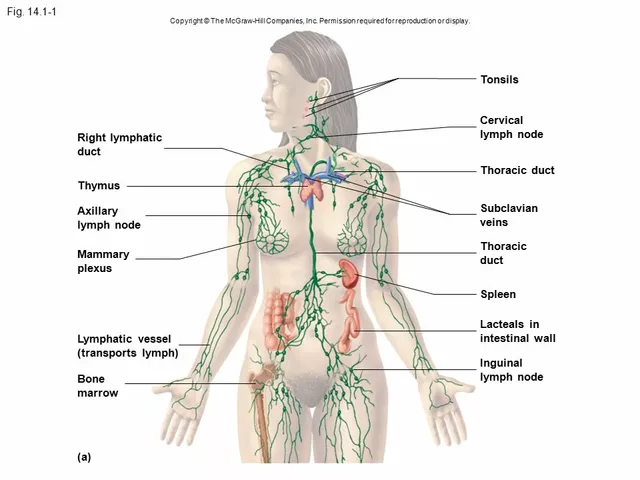
Another star player is secretory IgA, the antibody that lines the gut and skin. Secretory IgA coats the intestinal lining, preventing pathogens from crossing into the bloodstream and, indirectly, reducing the bacterial load that can migrate to the diaper area.
The infant skin microbiome also benefits. Breast milk delivers prebiotic oligosaccharides that nurture beneficial bacteria like Lactobacillus and Bifidobacterium. A balanced microbiome keeps the skin’s pH around 5.5, an environment hostile to the yeast and molds that cause rash.
Key Differences: Breastfeeding vs. Formula Feeding
| Attribute | Breastfeeding | Formula Feeding |
|---|---|---|
| Immunoglobulins (IgA) | High - natural source | Low - added in limited amounts |
| Lactoferrin | Present - antibacterial | Absent or minimal |
| Prebiotic Oligosaccharides | Rich - feeds good bacteria | Varies - often added synthetically |
| Skin pH impact | Maintains acidic pH (≈5.5) | Can be more alkaline |
| Diaper rash incidence (first 6months) | ≈15% (mild cases) | ≈30% (mild to moderate) |
These numbers aren’t miracles; they’re averages from large pediatric cohorts. Still, they illustrate that breast milk delivers a cocktail of protective agents you simply can’t replicate in a powder.
Practical Prevention Steps That Pair With Breastfeeding
- Change diapers often-ideally every 2‑3hours or immediately after a bowel movement.
- Use a soft, breathable cloth or a high‑quality disposable liner that wicks moisture away.
- Apply a thin layer of barrier cream (e.g., zinc‑oxide based) after each change. Zinc‑oxide protects by forming a moisture‑proof film.
- Avoid scented wipes; plain water and a soft cloth are safest.
- Let the skin air‑dry for a minute before putting on a new diaper.
When you combine these habits with the natural shield of breast milk, the odds of a rash hitting the severe category shrink dramatically.
Treating an Existing Rash: When Breastfeeding Helps Heal
If a rash has already appeared, keep the feeding routine unchanged-breast milk continues to supply anti‑inflammatory agents. Add these steps:
- Give the skin a break: expose the affected area to air for 10‑15minutes, 3‑4 times a day.
- Apply a thin layer of a probiotic ointment (containing Lactobacillus reuteri) to reseed the skin with friendly microbes.
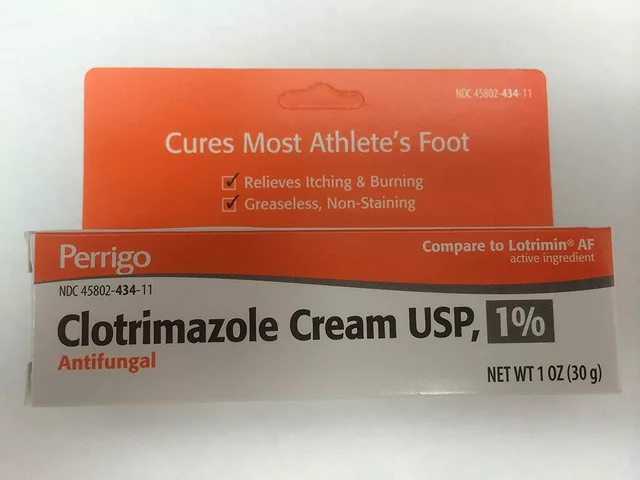
- For candidal infections, a pediatrician may prescribe a short course of an antifungal agent such as nystatin; the medication works faster when the infant’s immune defenses are already bolstered by secretory IgA.
- Continue using zinc‑oxide barrier cream, but switch to a fragrance‑free formula if irritation persists.
Most mild rashes resolve within 48hours when these measures are followed alongside regular breastfeeding.

Related Concepts You Might Explore Next
Understanding how breast milk protects the skin opens doors to other topics:
- Infant nutrition - the broader role of macro‑ and micronutrients in growth.
- Maternal diet - how a mother's intake of zinc, vitaminA, and omega‑3s influences milk composition.
- Skin barrier development - the timeline of the stratum corneum’s maturation during the first year.
- Probiotic supplements for infants - evidence on when they’re needed beyond breastfeeding.
Common Pitfalls and How to Avoid Them
Even the best‑equipped parents can slip. Here are three traps and quick fixes:
- Over‑wetting: Leaving a wet diaper on for too long creates a perfect breeding ground. Set a timer on your phone if you’re busy.
- Heavy creams: Thick ointments can trap heat, worsening inflammation. Use a pea‑sized amount.
- Introducing solid foods too early: Solids can change stool pH, indirectly affecting the diaper area. Follow WHO recommendations-start around six months.
Bottom Line
Breastfeeding delivers a built‑in anti‑rash system-lactoferrin, secretory IgA, prebiotic sugars, and a balanced microbiome-all working to keep the diaper area dry, acidic, and hostile to pathogens. Pair that natural armor with good diaper hygiene, a light barrier cream, and targeted treatment if a rash strikes, and you’ll give your baby the smoothest, most comfortable start possible.
Frequently Asked Questions
Can formula‑fed babies get the same protection as breastfed ones?
Formula can include added prebiotics and probiotics, but it lacks the live immunoglobulins and lactoferrin found in breast milk. The protective effect is therefore weaker, and studies show a higher rash rate in formula‑fed infants.
How often should I change my baby’s diaper to prevent rash?
Aim for every 2‑3hours, or immediately after a bowel movement. In hot climates or during nighttime, check the diaper at least once every 3‑4hours.
Is zinc‑oxide barrier cream safe for daily use?
Yes. Zinc‑oxide is a mineral that stays on the surface and isn’t absorbed. Apply a thin layer after each change; avoid thick layers that can trap moisture.
What role does the infant’s skin pH play in diaper rash?
A slightly acidic pH (around 5.5) discourages yeast and bacterial overgrowth. Breast milk’s prebiotic sugars help maintain this acidity, while alkalinity from urine can raise the pH and invite irritation.
When should I see a pediatrician for diaper rash?
If the rash spreads beyond the diaper area, shows signs of infection (pus, fever, extreme redness), or doesn’t improve after 48hours of home care, schedule a visit. Persistent candidal infections often need prescription antifungals.






Shawn Towner September 27, 2025
When you read about breast milk being a miracle shield, the reality is a bit more nuanced. The immunological cocktail is impressive, but it’s not a license to skimp on basic diaper hygiene. Lactoferrin and secretory IgA do help keep bacterial loads down, yet they can’t completely neutralize a soggy diaper left on all night. Parents still need to change frequently and use breathable liners. Think of breast milk as a supportive teammate, not the sole referee of skin health.
Ujjwal prakash September 29, 2025
Interesting point!!!, but let’s not forget that even with the best immunoglobulins, the diaper environment is a breeding ground-especially in warm climates!!! Proper airflow matters; a mother’s diet influences milk composition, too; the prebiotic oligossacharides are crucial for feeding good bacteria; without them, you might still see rash flare‑ups!!! So, don’t rely solely on lactoferrin; combine with good diaper practices.
Diane Helene Lalande October 1, 2025
I totally agree that breast milk offers a protective edge, but the fundamentals still apply. Changing diapers every few hours, using a thin zinc‑oxide layer, and letting the skin air‑dry are simple steps that work hand‑in‑hand with the milk’s antibodies. Keep the routine consistent and you’ll see fewer red patches.
Edwin Levita October 3, 2025
Let us pause and consider the theatricality of the "breast milk miracle" narrative that permeates many parenting forums. While lactoferrin and secretory IgA are indeed marvels of evolutionary chemistry, they are not omnipotent guardians against the relentless onslaught of moisture and friction that defines the diaper micro‑environment. The statistical reduction in rash incidence, cited as roughly fifteen percent versus thirty percent, is compelling yet still leaves a substantial fraction of breastfed infants vulnerable. This suggests that the protective effect is probabilistic, not deterministic, and must be bolstered by diligent hygiene practices.
First, the frequency of diaper changes remains paramount; a wet diaper is a fertile medium for Candida and Staphylococcus, irrespective of the infant’s diet. Second, barrier creams, particularly those based on zinc‑oxide, form a physical shield that prevents irritants from contacting the skin-a function that no component of breast milk can replicate once the skin is already compromised. Third, the pH balance of the diaper area is a dynamic variable; the acidic milieu fostered by prebiotic oligosaccharides can be quickly overridden by alkaline urine, especially in older infants.
Moreover, the maternal diet influences milk composition. Adequate maternal intake of zinc, vitamin A, and omega‑3 fatty acids can augment the concentration of anti‑inflammatory agents, but such nutritional optimization is often overlooked amidst the rush of new parenthood. The literature also points to the gut‑skin axis: a healthy intestinal microbiome, nourished by breast milk’s oligosaccharides, can modulate systemic immunity, yet this is a delayed effect that does not substitute for immediate topical care.
In practice, a synergistic regimen-exclusive breastfeeding paired with vigilant diaper hygiene, judicious use of barrier creams, and periodic skin air‑exposure-offers the most robust defense. Parents who abandon any one of these pillars risk seeing the rash reappear, sometimes more aggressively. So, while we celebrate the virtues of breast milk, let us not romanticize it to the point of neglecting the basics.
Xander Laframboise October 6, 2025
All that drama aside, the data doesn’t lie: the numbers still favor breastmilk, but the article glosses over the fact that many formula brands now include added lactoferrin and probiotics, narrowing the gap considerably. You can achieve similar outcomes with the right formula, especially when combined with strict diaper hygiene. So, the "miracle" tag is a bit exaggerated.
Jason Petersen October 8, 2025
From an analytical standpoint the study cited shows correlation not causation. Other variables like socioeconomic status and access to quality diapers could skew results. Data should be interpreted with caution.
Melissa Gerard October 10, 2025
Breastfeeding is overrated 😂
Cindy Knox October 13, 2025
While I respect the enthusiasm, it’s important to remember that every baby’s skin is unique. Some infants thrive solely on breastfeeding and rarely see rash, while others may still need extra barrier creams despite the milk’s benefits. Balancing scientific insight with personal experience creates the best care plan.
beverly judge October 15, 2025
For those looking for practical steps, consider setting a timer on your phone to remind you of diaper checks, especially during nighttime. Choosing fragrance‑free wipes and applying a pea‑sized amount of zinc‑oxide cream can prevent over‑moisture buildup. Also, ensure the baby’s diaper fits snugly but not too tight, as friction can exacerbate irritation.
Capt Jack Sparrow October 17, 2025
Exactly, and to add, the microbiome angle is fascinating. The prebiotic oligosaccharides in breast milk feed beneficial bacteria, which in turn produce short‑chain fatty acids that help maintain skin pH. That’s a biochemical cascade you don’t get from most formulas.
Manju priya October 20, 2025
Dear parents, remember that consistency is key. Embrace the routine of frequent diaper changes, gentle cleansing, and the natural protection breast milk provides. Your dedication will foster healthier skin and a happier infant.
Jesse Groenendaal October 22, 2025
While motivation is admirable, let’s not ignore that some infants simply have sensitive skin regardless of feeding method. In such cases, a pediatrician’s guidance and prescription‑strength treatments may be necessary. Over‑relying on anecdotal encouragement can delay proper medical care.