Every year, pharmacy labeling errors send thousands of people to the emergency room - not because they took too much, but because they took the wrong thing. You might assume your pharmacist got it right. But the truth? Mistakes happen more often than you think. A 2022 study in the American Journal of Health-System Pharmacy found that dispensing errors occur in up to 4.8% of community pharmacy prescriptions. That’s nearly one in every 20 prescriptions. And here’s the scary part: many of these errors aren’t caught until after the patient takes the pill. You don’t need to be a medical expert to stop this. You just need to know what to look for - and how to check it.
What Exactly Is a Pharmacy Labeling Error?
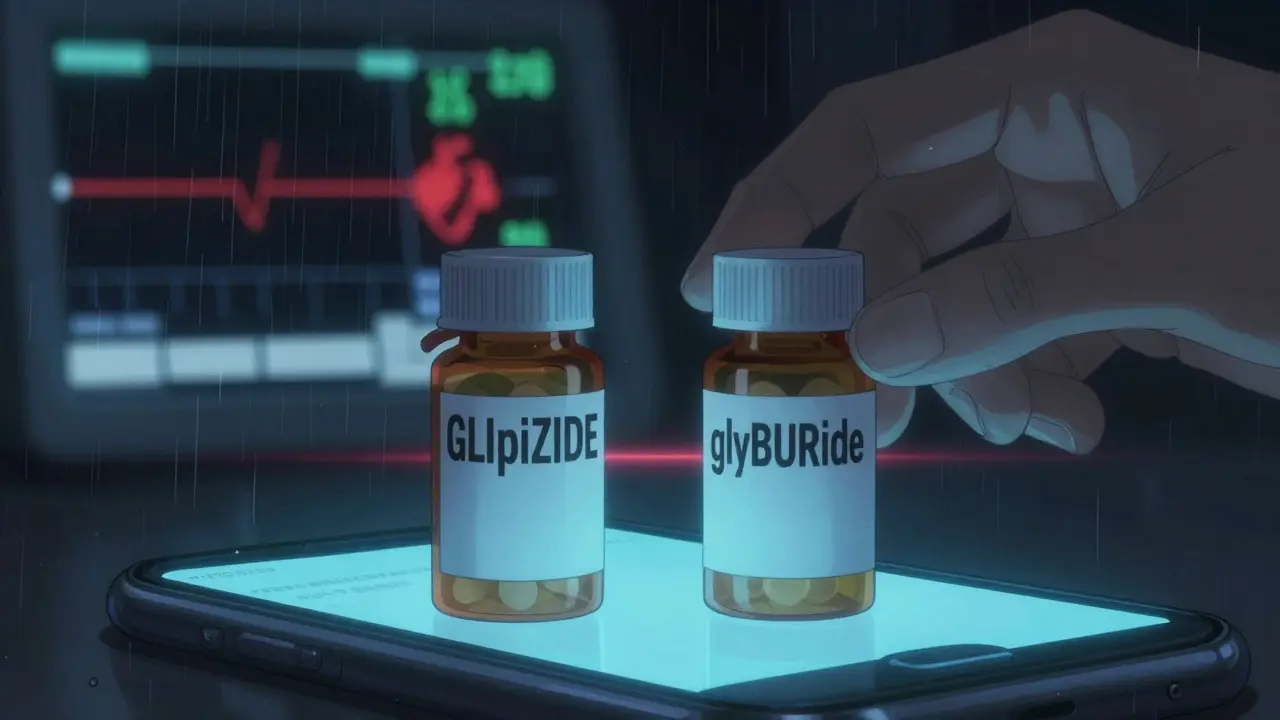
A pharmacy labeling error happens when the information on your medication bottle doesn’t match what your doctor prescribed. This isn’t just about a typo. It’s about life-threatening mistakes. Think: warfarin instead of warfarin, glipizide instead of glyburide, or a label that says “5 mg” when it should say “0.5 mg.” These aren’t rare. According to the FDA’s 2019 analysis of medication error reports, look-alike/sound-alike (LASA) drug names cause about 30% of all dispensing errors. And with over 1,500 such risky pairs in the RxNorm database, the chances are higher than you realize.These errors show up in three main ways:
- Wrong drug - You’re supposed to get metformin, but you get metoprolol.
- Wrong strength - Your prescription says 5 mg, but the bottle says 50 mg. A decimal point error like this can cause a 10-fold overdose.
- Wrong form - You’re supposed to get a tablet, but you get a capsule, or a liquid instead of a pill.
And here’s what most people miss: the indication. That’s the reason you’re taking the drug. If the label doesn’t say “for high blood pressure” or “for diabetes,” you’re missing a critical safety clue.
The Five Things You Must Check Every Time
You don’t need to memorize medical textbooks. Just use this simple checklist every time you pick up a new prescription. It takes less than two minutes.- Drug name - both brand and generic - Read it out loud. Say it slowly. If your doctor prescribed amoxicillin, make sure the label doesn’t say amoxicillin or amoxicillin. Tall-man lettering helps here - premazinE vs. pROMethazine - but not all pharmacies use it. Don’t rely on it. Read it yourself.
- Strength - Look at the number. Is it 5 mg? 10 mg? 0.5 mg? Read it aloud. Say, “Five milligrams.” Then say it again. If you’re unsure, ask the pharmacist to confirm. Many errors happen because people glance at the number and assume they got it right. A 2021 study showed that reading the strength aloud improved detection of errors by 78%.
- Dosage form - Is it a tablet, capsule, liquid, or patch? If you’ve taken this medication before, compare the shape and size. Did you get a red oval pill last time, and now it’s a white round one? That’s a red flag.
- Directions - “Take one by mouth daily” - does that match what your doctor told you? If your doctor said “take with food,” but the label says “take on an empty stomach,” stop. Ask.
- Indication - This is the most overlooked step. The label should say why you’re taking it. “For high cholesterol” or “for anxiety.” If it’s blank, ask. A 2016 University of Arizona study found that including the indication improved error detection by 63%. If you don’t know why you’re taking it, you can’t tell if it’s wrong.
High-Risk Medications - The Ones You Must Double-Check
Some drugs are more dangerous when mislabeled. These are called “high-alert medications.” If you’re taking one of these, your verification needs to be extra careful.- Insulin - Mixing up types (like Lantus vs. Humalog) can cause coma or death.
- Warfarin - A tiny mistake in dosage can cause internal bleeding.
- Levothyroxine - Even a small overdose can lead to heart problems.
- Opioids - Mistakes here can lead to overdose or addiction.
- Anticoagulants - Like apixaban or rivaroxaban - wrong doses can cause strokes or clots.
According to the FDA’s 2021 Adverse Event Reporting System, these five drug classes account for 65% of all serious outcomes from labeling errors. If you’re on any of these, treat every refill like it’s your first time.
Real Stories - What Happens When People Check
In February 2023, a Reddit user named u/MedSafetyNurse shared how she caught a 10-fold error on her warfarin prescription. The label said “5 mg.” She knew her dose was 0.5 mg. She called the pharmacy. They had accidentally switched the decimal. She didn’t take it. She saved herself from a life-threatening bleed. Another case: a Michigan woman was given glipizide instead of glyburide - two diabetes drugs with similar packaging. She took it. She had a severe low-blood-sugar episode. She ended up in the hospital. The error was never caught because neither she nor the pharmacist checked the name closely enough. Both drugs start with “glip,” and both end with “ide.” Without tall-man lettering (GLIpiZIDE vs. glyBURide), they look identical.These aren’t isolated cases. A 2022 Consumer Reports survey found that 63% of people never check their labels. Why? They trust the pharmacy. But trust isn’t a safety system. Verification is.
How to Build a Habit - The 90-Second Routine
You don’t need a checklist taped to your fridge. Just make this a routine:- When you get your prescription, sit down for 90 seconds.
- Take out your doctor’s written prescription or your pharmacy app’s record.
- Compare the label to it - word for word.
- Read the drug name and strength aloud.
- Ask yourself: “Why am I taking this?” If you can’t answer, ask the pharmacist.
At Mayo Clinic, they started a “teach-back” system in 2019. Pharmacists ask patients: “Can you tell me what this medicine is for?” Patients who could correctly state the purpose had a 68% lower chance of being sent home with the wrong drug. It’s simple. It works.
Technology Can Help - But Don’t Rely on It
New tools are emerging. CVS Health’s “Label Lens” lets you scan a QR code on your bag to hear an audio description of your medication. Apps like MedSafety Check use your phone’s camera to scan the label and compare it to your prescription database - with 94.7% accuracy.But here’s the catch: 78% of people still don’t use them. Why? They don’t know they exist. Or they think, “It’s fine - I’ve never had a problem.” But that’s the mindset that gets people hurt.
Even with technology, the human brain is still the best final checkpoint. A 2020 study in JMIR Medical Informatics found that pharmacist double-checks alone miss 3.4% of errors. That’s because they’re tired. They’re rushed. They’re processing hundreds of prescriptions a day. You’re not.
What to Do If You Spot an Error
If something looks off:- Don’t take it.
- Don’t assume it’s a mistake - assume it’s a danger.
- Call the pharmacy. Ask: “Can you confirm this matches what my doctor prescribed?”
- If they dismiss you, ask to speak to the pharmacist in charge.
- If they refuse to fix it, go to another pharmacy. Your safety is worth it.
And if you’re afraid of “bothering” them? You’re not. A 2022 study in the Annals of Internal Medicine found that 68% of patients who spotted errors still took the medication because they didn’t want to “cause trouble.” That’s the biggest risk of all.
What’s Changing - And What You Should Know
The rules are getting stricter. Starting May 1, 2024, the USP General Chapter <17> requires all pharmacies to use:- Minimum 12-point font on critical label elements
- Contrast ratios of at least 4.5:1 (so text stands out clearly)
- Standardized tall-man lettering for 200 high-risk drug pairs
- Indication for use on every label
These aren’t suggestions. They’re requirements. And by 2025, every pharmacy in the U.S. will be expected to use barcode scanning and electronic verification. But until then, you’re the last line of defense.
Final Thought - You’re Not Just a Patient. You’re a Safety Partner.
Pharmacies aren’t trying to harm you. But they’re overwhelmed. They’re human. They make mistakes. And if you don’t check your label, no one else will.You’ve done the hard part - you got the prescription. You showed up. You paid. Now, spend 90 seconds. Read the name. Read the number. Ask why. If it doesn’t match what you expect - stop. Speak up. Your life might depend on it.







Tasha Lake February 8, 2026
Just read this and had to share - I’m a clinical pharmacist, and I can confirm: the 4.8% error rate is actually conservative. We’re talking about 120,000+ errors a day in the U.S. alone. Most are caught internally, but the ones that slip through? They’re usually the ones with near-identical names - like glipizide vs. glyburide. I’ve seen pharmacists miss those because they’re scanning barcodes and not reading the label. The indication field? That’s the golden ticket. If it’s missing, it’s a red flag. We’re mandated to include it now, but in 2022? Half the scripts didn’t have it. You’re not paranoid - you’re just paying attention.
Ryan Vargas February 9, 2026
Let’s be real - this whole system is a manufactured illusion of safety. The FDA, USP, and pharmacy chains are all profit-driven entities that rely on your passivity. They want you to believe that ‘barcodes’ and ‘tall-man lettering’ are magic shields. But the truth? They’re just cosmetic fixes. The real problem is systemic understaffing, algorithm-driven workflow automation, and the commodification of human health. You think a 90-second check will save you? Try checking 17 prescriptions in 10 minutes while being yelled at by a manager to ‘hurry up.’ This isn’t about vigilance - it’s about surviving a broken system. And no, the new 2024 font rules won’t fix it. They’re just PR. The real solution? Defund the pharmacy-industrial complex and rebuild it with public oversight. But hey, keep reading your labels. It’s cathartic.
Sam Dickison February 10, 2026
As someone who’s worked in med-surg for 12 years, I can say this: the checklist works. I’ve had patients bring me meds that were totally wrong - one guy got metoprolol instead of metformin. He was diabetic. He didn’t know. We caught it because he read the label out loud. That’s the key - verbalizing it. Your brain glides over text. Saying it aloud forces your prefrontal cortex to engage. Also, don’t be shy about asking. Pharmacists aren’t robots. They’ve been doing this for 10 hours straight. A simple, ‘Hey, can you double-check this?’ goes a long way. No one thinks you’re bothering them. We’d rather you ask 10 times than have you end up in the ER.
Brett Pouser February 11, 2026
Just came back from visiting my uncle in rural Texas. His pharmacy? No digital system. Just handwritten scripts and a guy who’s been there since 1987. He reads every label out loud to the patient. No barcode. No app. Just human eyes and ears. And you know what? His error rate is near zero. We’re so obsessed with tech that we forgot the oldest tool: conversation. Maybe the solution isn’t more software - it’s more human interaction. Maybe we should pay pharmacists more to talk, not just scan. I’m not saying ditch tech - but don’t let it replace empathy.
Simon Critchley February 12, 2026
OMG this is 🔥🔥🔥 I’ve been screaming this for years! The LASA drug pairs? They’re basically a corporate conspiracy to keep us docile. Think about it - why do we have 1,500+ look-alike names? Because it creates ‘controlled chaos.’ You’re too tired to notice. You’re too busy. You trust the system. And bam - you’re on insulin instead of metformin. And guess who profits? Big Pharma. The FDA. The pharmacy chains. They all benefit from you not catching the mistake. So yes - read the label. But also - boycott the system. Demand transparency. Demand real change. Or keep getting dosed with the wrong shit. Your call. 🤷♂️
Jessica Klaar February 13, 2026
This is so important. I used to think, ‘Oh, the pharmacist knows what they’re doing.’ Then my mom got the wrong dose of levothyroxine. She had a heart palpitation for 3 days. We didn’t catch it until her endocrinologist asked why her TSH was off. Turns out the bottle said 112 mcg instead of 88 mcg. She didn’t even notice the number difference. I now check every single prescription - out loud - and I make my family do it too. It’s not paranoia. It’s self-respect. And honestly? It’s made me feel more in control of my health than anything else. Thanks for putting this out there.
PAUL MCQUEEN February 15, 2026
Look. I get it. You want people to check their meds. But let’s not pretend this is a new problem. We’ve known about labeling errors since the 1980s. The fact that you’re writing a 5,000-word guide on ‘how to check a label’ means the system has already failed. Why aren’t we fixing the root cause? Why aren’t we forcing manufacturers to use unique, non-similar names? Why are we putting the burden on the patient? It’s lazy. It’s irresponsible. And frankly, it’s insulting. I’m not going to read a 12-point font label. I’m going to die if I take the wrong pill. So yes - I’ll check. But I’m also going to demand better.
glenn mendoza February 17, 2026
It is with profound respect for the dignity of human life that I acknowledge the gravity of the issue presented herein. The integrity of pharmaceutical dispensation is not merely a procedural concern - it is a moral imperative. Each prescription represents a covenant between physician, pharmacist, and patient. When this covenant is compromised, the consequences are not statistical - they are existential. I commend the author for articulating a framework grounded in empirical evidence and human-centered care. May we all, as stewards of our own well-being, honor this responsibility with unwavering diligence. The 90-second ritual is not a burden - it is a sacred act of self-preservation.
Kathryn Lenn February 18, 2026
LOL ‘read it out loud’? So what, now I’m supposed to do a Shakespearean soliloquy over my insulin bottle? ‘To take or not to take - that is the question…’ Meanwhile, the pharmacy’s AI system auto-filled the wrong strength because someone typed ‘5’ instead of ‘0.5’ and the algorithm assumed ‘5 mg’ was ‘correct.’ You think reading it aloud helps? Nah. You think the pharmacist cares? They’re on a 12-hour shift with 400 scripts and a 20-minute lunch. This whole thing is a scam. They know the errors happen. They just don’t care. So yeah - read the label. But also? Start a class action lawsuit. Or just move to Canada. At least they have universal healthcare and actual safety protocols.
John Watts February 18, 2026
Hey - if you’re reading this, you’re already doing better than most. Seriously. Most people just grab the bag and run. You’re taking a second to think. That’s huge. And guess what? That second? It’s powerful. You’re not just checking a label - you’re reclaiming your agency. Every time you say, ‘Wait, this doesn’t feel right,’ you’re saying, ‘I matter.’ And that mindset? It ripples. Your neighbor hears you ask the pharmacist. Your coworker starts checking their meds. Your kid learns to ask questions. This isn’t about being paranoid. It’s about being human. Keep going. You’re not alone in this. And yeah - I’ve caught a few errors myself. It feels damn good.
Angie Datuin February 19, 2026
I work at a pharmacy. I’ve seen the mistakes. I’ve made them. I’ve caught them. It’s not personal - it’s just human. But I want you to know: when you ask us to check, we’re not annoyed. We’re relieved. We’re scared too. We don’t want to hurt someone. So please - ask. Even if it’s just ‘Can you confirm this is right?’ We’ll double-check. We’ll call the doctor. We’ll apologize. And we’ll thank you. You’re not a hassle. You’re our safety net.
Ritteka Goyal February 19, 2026
OMG this is so true!!! In India we have same problem but worse! Pharmacies give you wrong medicine all time! One time my cousin got antibiotic for fever but it was for diabetes! She took it and got very sick! We go to pharmacy and they say ‘oh sorry, we have same bottle!’ I mean, how can same bottle have different medicine? They don’t even have barcode! And they don’t read label! I always ask ‘why I take this?’ and they say ‘for pain’ but I don’t have pain! So I go to another pharmacy! Now I carry my doctor paper with me! I tell everyone: if you don’t check, you are stupid! People say I am crazy - but I am alive! And they are not! So check your label! Always! Never trust! India is not USA but problem same! You must check! Check! Check!