Beta Blocker Long-Term: What Happens When You Take Them for Years
When you take a beta blocker long-term, a class of medications that slow your heart rate and lower blood pressure by blocking adrenaline. Also known as beta-adrenergic blocking agents, they’re commonly prescribed for high blood pressure, heart rhythm issues, and after a heart attack. Many people stay on them for years—sometimes for life—because they work. But what does that actually do to your body over time?
One of the biggest concerns with beta blocker long-term use is whether your heart becomes dependent on them. It’s not addiction like with opioids, but your body does adapt. If you suddenly stop, your heart can go into overdrive—fast, irregular beats, spikes in blood pressure, even chest pain. That’s why doctors never tell you to quit cold turkey. Tapering off slowly is non-negotiable. This isn’t just a precaution; it’s backed by real cases of rebound hypertension and heart events after abrupt withdrawal.
Then there’s the side effects that creep in over time. Fatigue? Common. Cold hands and feet? That’s from reduced blood flow to the extremities. Some people notice their exercise tolerance drops—not because they’re out of shape, but because the beta blocker is holding back their heart’s natural response to exertion. And while they protect the heart, they can also mask low blood sugar symptoms in diabetics. That’s dangerous if you don’t know what to look for. Weight gain? It happens. Not always, but enough that people on long-term therapy should track their weight and activity levels closely.
Not everyone handles them the same. Older adults often need lower doses because their bodies process these drugs slower. People with asthma or COPD have to be extra careful—some beta blockers can tighten airways. And if you’re on other meds, like calcium channel blockers or certain antidepressants, the combo can slow your heart too much. That’s why regular check-ins with your doctor aren’t optional. Blood pressure checks, heart rate monitoring, and occasional blood tests help catch problems before they become serious.
What you won’t find in most drug labels is how many people stop taking beta blockers because of side effects. Studies show up to 30% discontinue within the first year—not because the drug failed, but because the trade-offs felt too high. But for others, especially those with heart failure or after a heart attack, staying on beta blockers long-term cuts the risk of death by nearly half. That’s not a small win.
There’s also the question of alternatives. If you’ve been on a beta blocker for five years and feel fine, should you keep going? Or could a different medication, lifestyle changes, or even a device like a pacemaker do the job better now? It’s not about whether beta blockers work—it’s whether they’re still the best choice for you right now.
Below, you’ll find real stories and data from people who’ve lived with these drugs for years. You’ll see what worked, what didn’t, and what to ask your doctor before making any changes. This isn’t theory. It’s what happens when medicine meets real life.
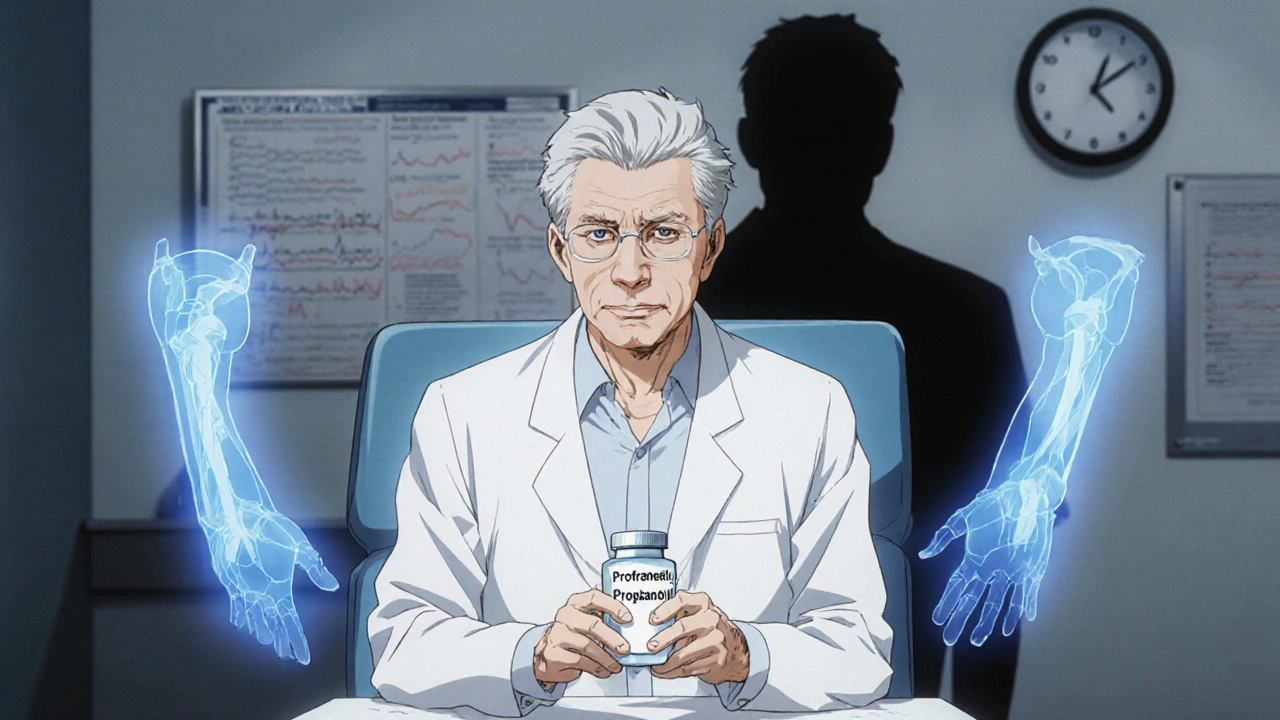
The Long-Term Effects of Propranolol: What to Expect After Months or Years of Use
Propranolol can be effective for years, but long-term use brings side effects like fatigue, weight gain, cold extremities, and mood changes. Learn what to expect, how to manage risks, and when to consider alternatives.