Most people assume that generic medications are just cheaper versions of brand-name drugs - and they’re right. But here’s what most don’t realize: generic medications can trigger allergic reactions even when the brand-name version never did. That’s not a mistake. It’s not bad luck. It’s because of the invisible stuff - the fillers, dyes, and preservatives - that make up the rest of the pill.
Why Generics Can Cause Reactions When Brand Names Don’t
By law, generic drugs must contain the same active ingredient as the brand-name version. That’s the part that actually treats your condition - whether it’s high blood pressure, depression, or an infection. But the rest? The coating, the coloring, the binder that holds the pill together? Those can be completely different.
Think of it like two identical cars with different engines. One runs on premium fuel, the other on regular. Same job. Different parts inside. For most people, it doesn’t matter. But if you’re allergic to regular fuel? You’re in trouble.
According to the FDA, generic manufacturers can use up to 83% different inactive ingredients than the brand-name version. And 27% of those differences involve substances known to cause allergic reactions. Common culprits include:
- Lactose (found in 28% of oral generics)
- Gluten (in 12% of generics)
- Tartrazine (FD&C Yellow No. 5 dye, in 15% of liquid generics)
- Peanut oil (in 8% of injectable generics)
- Magnesium stearate (linked to reactions in penicillin-allergic patients)
A 2021 study in the Journal of Allergy and Clinical Immunology found that 7.3% of people with documented drug allergies had reactions specifically to generic formulations - not because of the medicine itself, but because of these hidden ingredients. One patient in California switched from brand-name sertraline (Zoloft) to a generic version and broke out in hives within 30 minutes. The brand had no dye. The generic did - tartrazine. Another patient with a peanut allergy went into anaphylaxis after taking a generic version of propofol that contained peanut oil, even though the brand version didn’t.
What Do Allergic Reactions to Generics Look Like?
Reactions can range from annoying to life-threatening. And they don’t always show up right away.
Mild reactions usually involve the skin:
- Rash (68% of cases)
- Hives (42%)
- Itching (57%)
These might seem harmless - but they’re a warning sign. The American Academy of Family Physicians found that 65% of people who have a mild reaction to a generic medication will have a worse reaction the next time they take it.
Moderate reactions involve more than one part of the body:
- Facial or lip swelling (29%)
- Wheezing or trouble breathing (31%)
- Nausea or vomiting (24%)
These symptoms mean your immune system is going into overdrive. It’s not just a rash anymore. It’s your body fighting what it thinks is a threat.
Severe reactions - anaphylaxis - happen in about 0.02% to 0.04% of generic drug doses. But when they do, they’re deadly without quick action:
- Throat tightness (87% of cases)
- Severe drop in blood pressure (systolic below 90 mmHg in 78%)
- Difficulty breathing (92%)
- Loss of consciousness
Forty-three percent of these severe reactions start within 15 minutes of taking the pill. Thirty-eight percent show up between 15 and 60 minutes. The rest? They can creep in hours later. That’s why you can’t just wait and see.
When to Call 911 or Go to the ER
If you’ve taken a generic medication and start feeling any of these, don’t wait:
- Wheezing, stridor, or breathing faster than 30 breaths per minute
- Systolic blood pressure below 90 mmHg, or a drop of more than 30% from your normal
- Swelling of the tongue, lips, or throat
- Feeling dizzy, faint, or like you’re going to pass out
- Two or more symptoms at once - like hives + vomiting + trouble breathing
This is anaphylaxis. It kills quickly. The Food Allergy Research & Education (FARE) group says 91% of medication-related anaphylaxis cases need epinephrine within 5 to 15 minutes to prevent death. If you have an epinephrine auto-injector (like an EpiPen), use it immediately. Then call 911. Even if you feel better after the shot, you still need to go to the hospital. Rebound reactions are common.
And here’s something many don’t know: epinephrine is the only treatment that works. Antihistamines like Benadryl won’t stop anaphylaxis. They might help with itching, but they won’t save your life.

When to Call Your Doctor (Even If It Feels Minor)
Not every reaction needs an ambulance. But if you get hives that last more than 6 hours, facial swelling that doesn’t go down after a few hours, or nausea/vomiting that doesn’t improve in 2 hours - call your doctor within 24 hours.
Even mild reactions should be evaluated by an allergist within 72 hours. Why? Because your body learns. The next time you take that same generic, your reaction could be worse. A 2023 study showed that patients who ignored mild reactions were three times more likely to have a severe reaction later.
And don’t assume your doctor knows about the difference between brand and generic. Most don’t. A 2023 survey found that 71% of allergy specialists now ask patients if they’ve had reactions to generics specifically - up from just 42% in 2019. You have to be the one to speak up.
How to Protect Yourself
Here’s what you can do right now to avoid another reaction:
- Know your triggers. If you’ve ever had a reaction to a generic, write down exactly what you took - brand name, generic name, and the pharmacy. Note the symptoms and when they started.
- Check the inactive ingredients. The FDA has a free database with over 1,200 inactive ingredients. Ask your pharmacist to look up the exact generic you’re getting and compare it to the brand. Don’t rely on the label - most don’t list allergens clearly.
- Ask for dye-free, gluten-free, or lactose-free versions. About 38% of major generic makers now offer these. They’re not always advertised, but they exist.
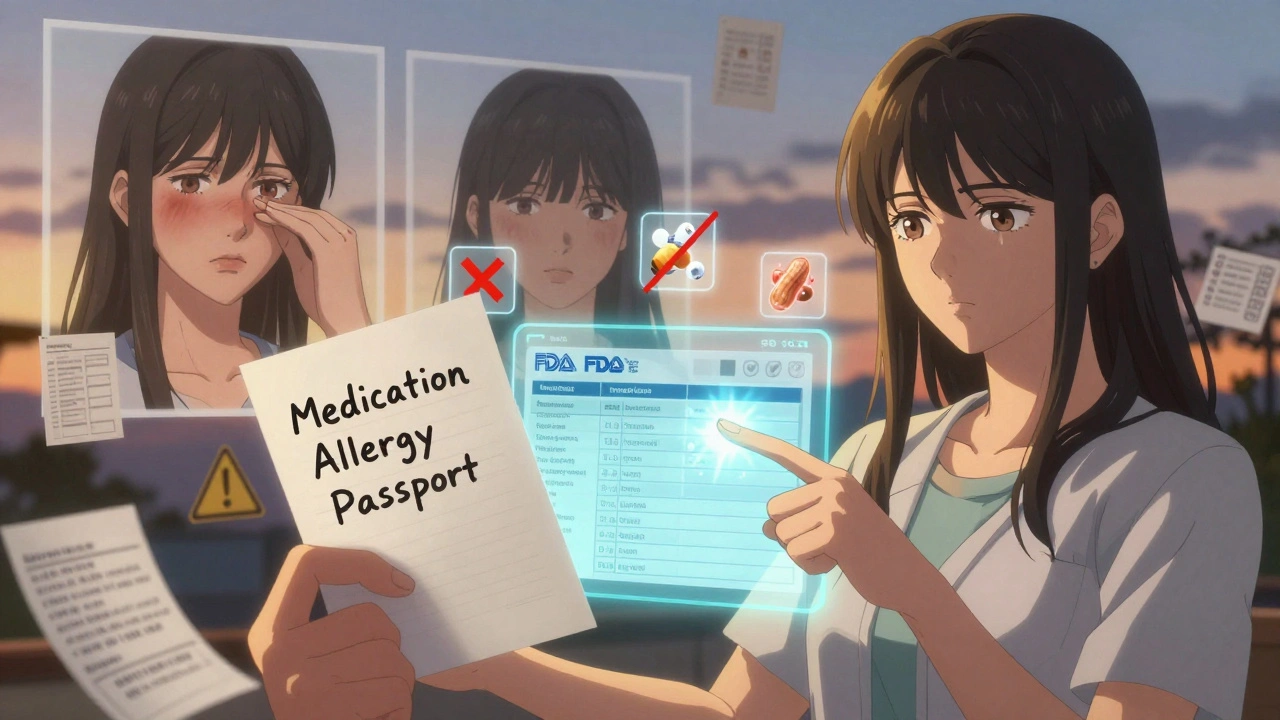
- Carry a “medication allergy passport.” This is a simple note - digital or paper - listing every ingredient you’re allergic to. A 2022 pilot study showed this reduces adverse events by 29%.
- Get tested. If you think you’re allergic to a drug, don’t just avoid it forever. Many people are mislabeled. A 2020 study found that 90% of people told they’re allergic to penicillin can safely take it after proper testing. Allergy testing costs $350-$600, but it can save you thousands in unnecessary alternative meds.
- Update your medical records. Tell every doctor, pharmacist, and hospital you visit: “I had a reaction to generic [drug name], not the brand. The culprit was [ingredient].” The American Medical Association says this cuts inappropriate drug avoidance by 37%.
What’s Changing - and What’s Not
The FDA now requires manufacturers to list problematic inactive ingredients on labels. But full compliance isn’t required until 2025. Until then, you’re still on your own.
And generics make up 90% of all prescriptions filled in the U.S. That means you’re likely to run into this issue again and again. The more you know, the safer you are.
One woman in Texas took generic amoxicillin for a sinus infection and broke out in hives. She’d taken the brand version dozens of times with no problem. Her allergist found the generic used a different form of magnesium stearate - something her immune system reacted to. She switched back to the brand. Her rash cleared in 48 hours. She now keeps a list of every generic she’s safely taken - and every one she hasn’t.
You can do the same.
Can generic medications cause allergic reactions even if the brand name didn’t?
Yes. Generic drugs must contain the same active ingredient as the brand-name version, but they can use different inactive ingredients like dyes, fillers, or preservatives. These can trigger allergic reactions in people who tolerate the brand-name version just fine. For example, tartrazine dye in a generic antidepressant or peanut oil in a generic anesthetic has caused reactions in patients who had no issues with the brand.
What are the most common allergens in generic medications?
The most common allergens in generics include lactose (found in 28% of oral generics), gluten (in 12%), tartrazine (FD&C Yellow No. 5 dye, in 15% of liquid forms), peanut oil (in 8% of injectables), and certain forms of magnesium stearate. These ingredients are not always listed prominently on packaging, making them easy to miss.
How quickly do allergic reactions to generics happen?
Reactions can start within minutes or take hours. About 43% of severe reactions begin within 15 minutes of taking the pill, 38% occur between 15 and 60 minutes, and 19% may take several hours to appear - especially with delayed hypersensitivity reactions. Never assume you’re safe just because you didn’t react right away.
Should I use an EpiPen if I have a reaction to a generic drug?
Yes - if you’re having symptoms of anaphylaxis, such as trouble breathing, throat swelling, a sudden drop in blood pressure, or dizziness. Epinephrine is the only treatment that can stop a life-threatening reaction. Antihistamines like Benadryl won’t work fast enough. Use your EpiPen immediately, then call 911. Even if you feel better, you still need emergency care because symptoms can return.
What should I do after a mild reaction to a generic medication?
Even if the reaction seems minor - like a rash or itching - contact your doctor within 24 hours. See an allergist within 72 hours. Mild reactions often get worse with future exposure. Your doctor can help identify the specific ingredient that caused the reaction and recommend safer alternatives, including dye-free or gluten-free generics.
Can I ask my pharmacist for a generic without certain ingredients?
Absolutely. About 38% of major generic manufacturers now offer versions labeled as dye-free, gluten-free, or lactose-free. You may need to ask specifically - these aren’t always advertised. Your pharmacist can check the FDA’s Inactive Ingredient Database to find a formulation that matches your needs. Don’t assume all generics are the same.
How do I know if I’m allergic to a generic or the drug itself?
If you reacted to a generic but not the brand-name version, it’s likely an inactive ingredient. Allergy testing can confirm this. Many patients are incorrectly labeled as allergic to a drug when they’re actually reacting to a filler or dye. Proper testing can safely identify whether you can still use the active ingredient - which is especially important for antibiotics like penicillin, where 90% of people labeled allergic can actually tolerate it after evaluation.
Is it safe to keep taking a generic if I had a mild reaction before?
No. Even mild reactions can become more severe with repeated exposure. The American Academy of Family Physicians found that 65% of people who had a mild reaction to a generic medication had a worse reaction the next time they took it. Avoid the specific generic formulation and talk to your doctor or pharmacist about alternatives. Don’t risk it.
What to Do Next
If you’ve ever had a reaction - even a small one - to a generic medication, write it down. Include the drug name, whether it was brand or generic, the symptoms, and how long they lasted. Keep this list with your other medical records.
Next time you fill a prescription, ask your pharmacist: “Is this generic the same as the brand in terms of inactive ingredients?” If they don’t know, ask them to check the FDA’s database. Don’t be shy. Your safety matters more than their convenience.
And if you’re on a long-term medication - especially for something like high blood pressure, depression, or asthma - consider getting tested. You might be avoiding a perfectly safe drug because of a filler you’re allergic to. That’s not just inconvenient. It’s dangerous.
You don’t have to guess. You don’t have to suffer. You just need to ask the right questions - and act before it’s too late.







Kylee Gregory December 5, 2025
It's wild how we assume 'same active ingredient' means 'same everything.' But medicine isn't just chemistry-it's a cocktail of fillers, dyes, and preservatives we never think about until our skin breaks out or our throat swells. This post nailed it. We treat generics like interchangeable widgets, but our bodies aren't factories. They're delicate ecosystems. And when you're allergic to a filler you didn't even know existed? That's not bad luck-it's systemic ignorance.
Laura Saye December 6, 2025
As someone who’s had two mild rashes from generics I didn’t even realize were different from the brand-I’m now keeping a digital 'medication passport.' I screenshot the inactive ingredients from the pharmacy’s label and save them in a folder. It’s tedious, but after the third time I thought, 'Wait, this is the same drug?' I realized I was playing Russian roulette with my immune system. If you’re on long-term meds, this is non-negotiable.
Stephanie Bodde December 7, 2025
You’re not alone!! 🙌 I had hives from a generic sertraline and thought I was just 'stressed.' Turns out it was tartrazine. My pharmacist didn’t even know to check. Now I always ask: 'Is this dye-free?' and they look at me like I’m asking for unicorn tears. But I don’t care-I’d rather pay extra than end up in the ER. You’ve got this!! 💪
James Moore December 9, 2025
Let me tell you something, folks-this isn’t about 'allergies,' this is about corporate greed masquerading as cost-saving. The FDA lets these companies swap in cheap fillers like they’re trading LEGO bricks, and then they slap a 'bioequivalent' sticker on it like it’s a badge of honor. We’re not just patients-we’re lab rats in a system that values profit over personhood. And don’t get me started on how 90% of prescriptions are generics now-this is a public health crisis being buried under bureaucratic jargon. Wake up, America! We’re being poisoned by paperwork.
Krishan Patel December 10, 2025
It is a well-documented fact that the United States Food and Drug Administration permits the substitution of inactive ingredients in generic pharmaceuticals without requiring prior patient consent. This constitutes a violation of the principle of informed consent under medical ethics. Moreover, the prevalence of lactose and gluten in oral formulations is not merely a statistical anomaly-it is a systemic failure of regulatory oversight. One must question the integrity of a system that permits allergenic excipients to be concealed under the guise of cost-efficiency.
Michael Dioso December 11, 2025
lol so now we’re supposed to be afraid of every generic? My grandma’s been on generic metoprolol for 15 years and she’s still gardening at 82. You’re telling me a dye in a pill is more dangerous than processed sugar or vaping? Chill. Most people are fine. If you’re allergic to everything, maybe stop taking pills altogether.
Rupa DasGupta December 12, 2025
OMG I had a reaction to a generic amoxicillin and my mom said I was 'overreacting' 😭 I cried for 3 hours. Now I only take brand name and I’m not sorry. My skin is clearer and my anxiety is down. Who cares if it costs $20 more? I’m not dying for a $5 savings. 💔
Lynette Myles December 13, 2025
They’re adding peanut oil to injectables? And we’re not talking about this on CNN? This is why I don’t trust the FDA. They’re all bought off by Big Pharma. I bet they knew this was happening for years. This isn’t an accident-it’s a cover-up.
Mark Ziegenbein December 14, 2025
It's fascinating how the modern medical-industrial complex has reduced human health to a cost-per-dose algorithm. We’ve forgotten that the body is not a machine with interchangeable parts. The inactive ingredients-those invisible, unregulated, unremarked-upon additives-are the silent architects of our physiological betrayal. And yet we’re told to 'just take the generic' like it’s a coupon for wellness. The tragedy isn’t the reaction-it’s that we’ve stopped asking why we’re being treated like commodities.
Chris Brown December 16, 2025
It’s irresponsible to scare people into thinking every generic is a ticking time bomb. If you’re allergic to tartrazine or lactose, you should have been tested years ago. This isn’t a systemic failure-it’s a personal failure of medical diligence. Stop blaming the system and start taking responsibility for your own health. The FDA isn’t your babysitter.
Juliet Morgan December 18, 2025
Thank you for writing this. I had a mild rash after switching to a generic and thought it was just dry skin. I didn’t connect it until I read this. I’m seeing an allergist next week. You’re right-we have to speak up. My doctor didn’t even know to ask. I’m gonna print this out and hand it to him. 💙
aditya dixit December 19, 2025
Interesting. In India, we don’t have this problem as much because most generics are made by the same manufacturers as the brand names. The difference is often just the packaging and branding. Still, I’ve seen people react to colorants in liquid antibiotics-especially kids. Maybe the real issue isn’t generics-it’s inconsistent labeling across markets.
Annie Grajewski December 21, 2025
so like… if i’m allergic to the dye in a generic pill… does that mean i’m allergic to the color yellow? like… am i gonna break out if i see a banana? 🤔
Norene Fulwiler December 22, 2025
My sister is from Ghana and she told me that in her village, people use traditional herbal remedies because they don’t trust pills at all. I used to think that was just 'backwards.' Now I get it. When you don’t know what’s in the pill, and no one tells you… why would you trust it? This post made me rethink everything.
Lucy Kavanagh December 22, 2025
Wait… so the government is letting companies put peanut oil in medicine? And you’re telling me this is legal? I’ve been taking generic propofol for years… I think I’m being targeted. This is a covert bioweapon. They want us to be afraid of our own bodies. They’re using fillers to make us dependent on expensive brands. It’s all a psyop. I’ve been documenting every pill I’ve taken since 2018. I have 17 binders. I’ll send you the files. We need to expose this.