When your liver is damaged by cirrhosis, pressure builds up in the portal vein-the main blood vessel carrying blood from your gut to your liver. That pressure forces blood to find new paths, creating swollen, fragile veins in your esophagus or stomach. These are called varices. And when they burst, it’s not just a bleed-it’s a medical emergency. About 1 in 5 people who experience variceal bleeding die within six weeks. But here’s the good news: with the right treatment, survival rates can jump dramatically. The key? Acting fast and using the right tools: endoscopic banding, beta-blockers, and smart prevention.
What Happens When Varices Bleed?
Variceal bleeding doesn’t come with warning signs. One moment you’re fine; the next, you’re vomiting bright red blood or passing black, tarry stools. Some people feel dizzy, faint, or have a rapid heartbeat. It’s sudden, scary, and deadly if not treated immediately. This isn’t a simple stomach upset-it’s a rupture in veins that have stretched thin from years of high pressure in the liver’s blood system. The root cause? Almost always advanced liver disease, especially from alcohol, hepatitis B or C, or fatty liver disease.Endoscopic Band Ligation: The Gold Standard for Stopping the Bleed
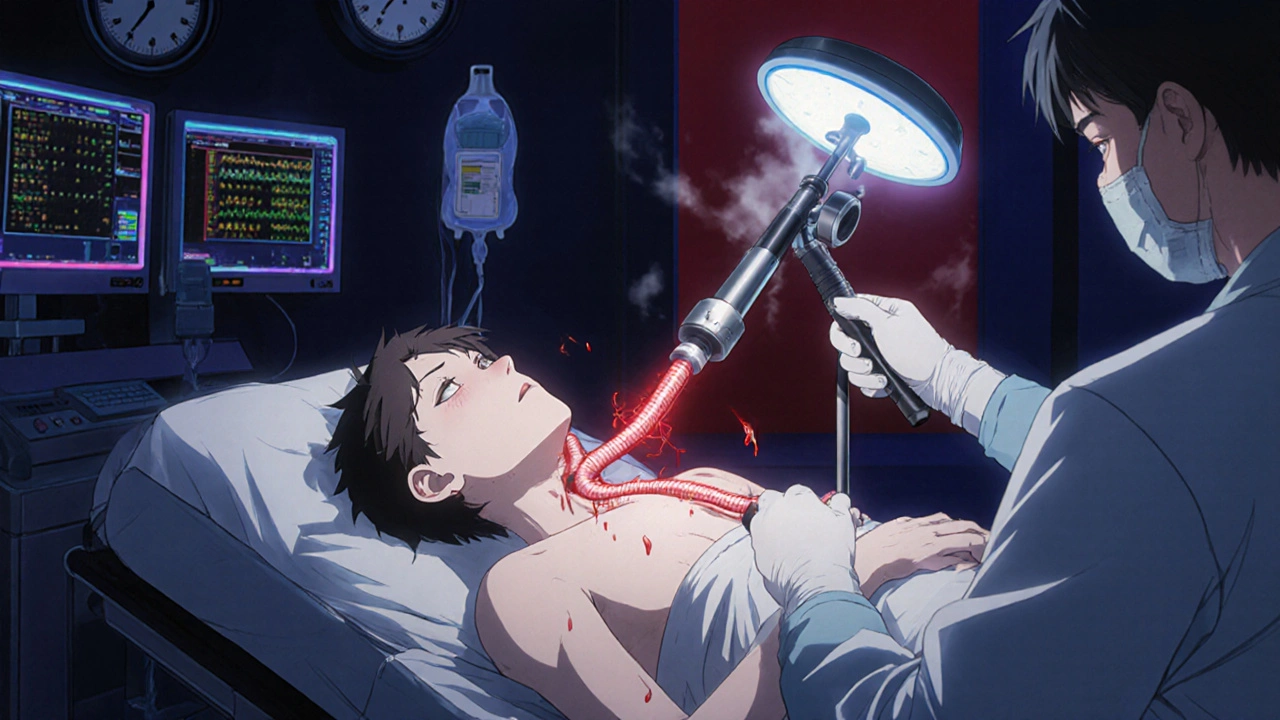
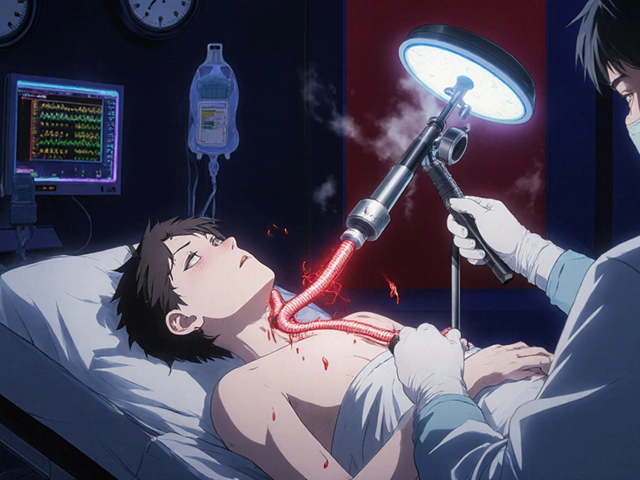
When someone arrives at the hospital with active bleeding, time is everything. The endoscopic band ligation (EBL) procedure is now the first-line treatment. It’s done with a thin, flexible camera (endoscope) inserted through the mouth. The doctor spots the swollen veins and places tiny rubber bands around them. These bands cut off blood flow, causing the varices to shrink and scar over. It’s not surgery-it’s a quick, minimally invasive procedure done under sedation. Studies show that when done within 12 hours of bleeding, banding stops the bleed in 90-95% of cases. That’s a huge improvement over older methods like injecting chemicals (sclerotherapy), which had more complications and lower success. Most patients need 3-4 sessions, spaced 1-2 weeks apart, to fully eliminate the varices. Each session costs between $1,200 and $1,800 in the U.S., but it’s far cheaper than the alternative: repeated emergency visits, ICU stays, or surgery. Some patients report throat pain or discomfort for a couple of weeks after banding. Others say it was a lifesaver-discharged in three days, back to normal. The key is doing it at a center with experience. Hospitals that perform more than 50 banding procedures a year have 15% lower rebleeding rates than low-volume centers. If you’re in a rural area, getting transferred to a major hospital quickly can make all the difference.Beta-Blockers: The Silent Shield Against Future Bleeds
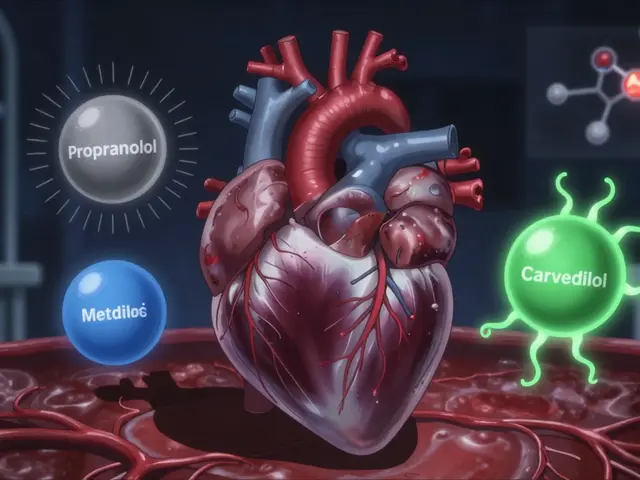
Stopping the current bleed is only half the battle. The real goal is to prevent it from happening again. That’s where non-selective beta-blockers (NSBBs) come in. These drugs-like propranolol and carvedilol-don’t just lower blood pressure. They reduce the pressure inside the portal vein by slowing the heart and decreasing blood flow to the liver. Carvedilol has become the preferred choice in recent years. A 2021 study showed it lowers portal pressure by 22%, compared to 15% with propranolol. Both cut the risk of rebleeding by about half. But they’re not for everyone. People with asthma, slow heart rates, or heart failure can’t take them. About 1 in 4 patients can’t tolerate the side effects-fatigue, dizziness, cold hands. One patient on Reddit said propranolol made him too tired to get out of bed. He switched to carvedilol and felt better, but the cost jumped to $35 a month. The goal isn’t just to take the pill-it’s to reach the right dose. Doctors use a test called HVPG (hepatic venous pressure gradient) to measure portal pressure directly. The target? A drop of at least 20% from baseline, or pressure below 12 mmHg. But studies show only 55% of patients ever reach that target dose within three months. Why? Fear of side effects, lack of follow-up, or poor access to specialists.
Prevention: The Best Treatment Is No Bleed at All
The most effective strategy? Prevent varices from forming in the first place. If you have cirrhosis but no varices yet, screening with endoscopy every 2-3 years is critical. If small varices are found, starting carvedilol can reduce the chance of bleeding by 50%. For those with medium or large varices, banding plus beta-blockers is the standard. But prevention isn’t just medical. It’s lifestyle. Stopping alcohol completely. Managing hepatitis with antivirals. Losing weight if you have fatty liver. These steps slow liver damage-and reduce the pressure that causes varices. The American Liver Foundation reports that 78% of patients are satisfied with their care, but 42% struggle with beta-blocker side effects. That’s why patient support programs matter. Nurse navigators help coordinate appointments, explain medications, and connect people with financial aid.When Banding and Pills Aren’t Enough
Some patients are too sick for standard treatment. If you have Child-Pugh class B or C cirrhosis and are actively bleeding, your risk of death is over 50%. That’s where TIPS-transjugular intrahepatic portosystemic shunt-comes in. It’s a procedure where a metal stent is placed inside the liver to create a new channel for blood to bypass the blocked portal vein. It’s highly effective: one study showed 1-year survival jumped from 61% to 86% with TIPS. But TIPS has a big downside: it can cause hepatic encephalopathy-brain fog, confusion, even coma-because toxins that the liver normally filters now bypass it. About 30% of patients develop it. And not every hospital can do it. Only 45% of U.S. hospitals have the trained interventional radiologists needed to perform TIPS within 24 hours. For gastric varices (in the stomach, not the esophagus), banding often fails. The better option is BRTO-balloon-occluded retrograde transvenous obliteration. A 2023 study showed 30-day mortality was less than half with BRTO compared to banding alone.
What’s Changing in 2025?
New developments are making treatment more precise and accessible. In 2023, the FDA approved a long-acting form of octreotide (Sandostatin LAR) that only needs monthly shots instead of daily injections. That could help patients who struggle with adherence. The upcoming Baveno VIII guidelines in 2024 may recommend carvedilol as a standalone option for primary prevention-meaning you might not need banding at all if you’re on the right drug and your varices are small. And future tech? AI is being tested to predict which cirrhosis patients are most likely to bleed. Early results suggest it could spot high-risk patterns months before a bleed happens. If it works, we could shift from emergency response to true prevention.What You Need to Know
If you or someone you care about has cirrhosis:- Get screened for varices with an endoscopy if you haven’t already.
- If varices are found, ask about carvedilol-it’s more effective than propranolol.
- If you bleed, demand endoscopic banding within 12 hours. Don’t wait.
- Know your options: TIPS, BRTO, and new drugs are available if standard treatments fail.
- Don’t ignore side effects. Talk to your doctor. There are alternatives.
- Stop drinking. Control your weight. Take your hepatitis meds. These are not optional.
Variceal bleeding is serious-but not inevitable. With timely care, the right medications, and smart prevention, most people can live for years without another bleed. The tools exist. The knowledge exists. What matters now is using them before it’s too late.




Shubham Semwal November 28, 2025
Let me break this down for you folks who think beta-blockers are magic pills. Propranolol? Overrated. Carvedilol? Now we’re talking. I’ve seen 3 patients in my clinic last month alone who were on propranolol, barely tolerating it, and then switched-suddenly they had energy, slept better, and their HVPG dropped like it owed someone money. Stop being lazy and ask for the right drug. Also, if you’re still drinking, none of this matters. You’re just delaying the inevitable.
Sam HardcastleJIV November 30, 2025
One cannot help but reflect upon the existential weight carried by the human liver-a silent organ, burdened by the sins of excess, yet expected to perform with unwavering fidelity. The medical intervention described herein, while technologically sophisticated, remains but a palliative gesture against the cosmic indifference of cellular decay. Banding, beta-blockers, TIPS-these are merely the rituals of a civilization that refuses to accept mortality as an inherent condition.
Mira Adam November 30, 2025
Ugh, another ‘just stop drinking’ lecture. Like that’s the only cause of cirrhosis. What about the 30-year-old who never touched alcohol but got fatty liver from soda and pizza? Or the person with hepatitis C who got it from a blood transfusion in 1987? You people act like it’s a moral failure. It’s not. It’s biology. And if you’re blaming patients, you’re part of the problem.
Miriam Lohrum December 1, 2025
It’s strange how we treat the body like a machine that can be fixed with tools, when really it’s a living system shaped by decades of choices, trauma, and luck. Banding stops the bleed, but it doesn’t heal the wound that led to it. The real question isn’t how to stop the bleeding-it’s why we let it get this far in the first place. Prevention isn’t just medical. It’s societal. It’s about access, education, and dignity.
archana das December 1, 2025
My uncle in Delhi had cirrhosis. He didn’t drink. He had hepatitis B since he was a kid. No one told him to get checked. No one had money for endoscopy. He bled out at home. I wish someone had told us about carvedilol. It’s not expensive here-under $5 a month. But no one knew. This info needs to reach villages, not just big hospitals. Education saves lives more than banding ever could.
Sue Haskett December 3, 2025
Wait-so you’re telling me that if you have cirrhosis, you need to get an endoscopy every 2–3 years? And if you’re high-risk, you need beta-blockers? And if you bleed, you need banding within 12 hours? And if that fails, TIPS? And if you have gastric varices, BRTO? And if you can’t afford it, there are nurse navigators? And if you’re still drinking, you’re just… wasting everyone’s time? Okay. I’m writing this down. And I’m printing it. And I’m putting it on my fridge. Because if I don’t, I’ll forget. And then I’ll die. And then my family will cry. And then… nothing changes. So I’m doing this. For me. For them. For everyone.
Jauregui Goudy December 5, 2025
Y’ALL. LISTEN. I had this friend-29, gym rat, never drank, got NAFLD from stress-eating donuts. Got diagnosed with cirrhosis. Didn’t believe it. Thought it was ‘just bloating.’ Then he vomited blood on his way to work. 12 hours later, banding. Three days later, home. Now he’s on carvedilol, takes his meds like a boss, and runs marathons. I’m telling you-this isn’t doom and gloom. This is a second chance. And if you’re reading this? You’re one step away from saving your own life. Don’t wait for the next bleed. Start today. Your liver will thank you. 💪❤️
Jonah Thunderbolt December 7, 2025
Wow. Just… wow. Another ‘medical miracle’ article written by someone who’s never met a patient who actually lives in the real world. Carvedilol? $35/month? Try $120 with insurance. TIPS? Only available at 45% of hospitals? That’s not healthcare-that’s a lottery. And AI predicting bleeds? Cute. Meanwhile, people are choosing between rent and their beta-blockers. You’re not saving lives-you’re selling hope to people who can’t afford it. 🤡
Rebecca Price December 9, 2025
Interesting. I appreciate the clinical detail. But let’s be honest-the real barrier isn’t the lack of knowledge. It’s the lack of compassion. The patient who can’t afford carvedilol? The one too ashamed to say they still drink? The one whose doctor dismissed their fatigue as ‘just stress’? We treat the liver like a broken pipe. But it’s part of a person. A person who’s scared. Who’s tired. Who’s been failed by the system. Maybe the real ‘gold standard’ isn’t banding. It’s listening.