QT Interval Risk Calculator
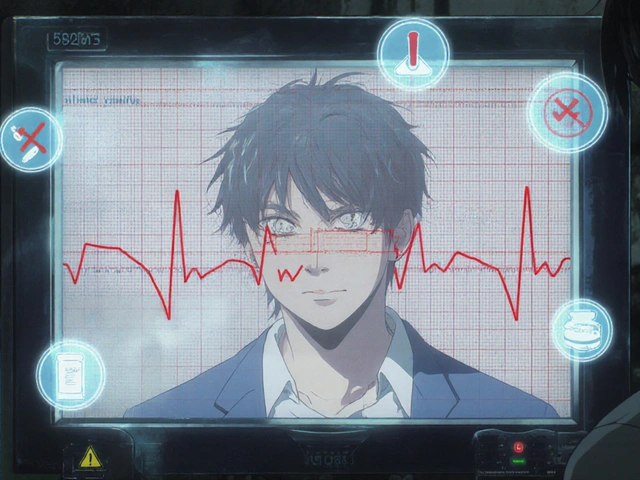
Your estimated QTc interval: ms
Risk level:
When you take an antipsychotic for schizophrenia, bipolar disorder, or severe depression, your doctor focuses on calming your mind. But there’s another system in your body that’s quietly affected-your heart. Some antipsychotics, especially when mixed with other common medications, can stretch out the heart’s electrical cycle in a way that raises the risk of a dangerous, sometimes deadly, irregular heartbeat called torsades de pointes. This isn’t theoretical. It’s happening right now in clinics and hospitals across the U.S. and Europe.
What QT Prolongation Really Means
Your heart beats because of electrical signals. After each beat, it needs time to reset-that’s called repolarization. The QT interval on an ECG measures how long that reset takes. If it’s too long-over 450 ms in men, 460 ms in women-you’re at risk. The heart’s electrical system gets unstable. It can start skipping beats, then spiral into a chaotic rhythm called torsades de pointes. That’s when the heart quivers instead of pumping. Without quick treatment, it leads to sudden cardiac death.
This isn’t new. French doctor Dessertenne first described torsades in 1966, right as antipsychotics were becoming common. Back then, doctors didn’t know. Today, we do. About 70% of antipsychotics on the market can prolong QT. And the real danger isn’t just one drug-it’s the mix.
Which Antipsychotics Are Riskiest?
Not all antipsychotics are created equal when it comes to heart risk. Some are far more likely to block the hERG potassium channel-the main culprit behind QT prolongation.
- High risk: Thioridazine (withdrawn in the U.S. but still used elsewhere), ziprasidone, haloperidol. These have IC50 values under 1 μM-meaning they block hERG at very low concentrations.
- Moderate risk: Quetiapine, risperidone, olanzapine. Commonly prescribed, but still carry measurable risk.
- Low risk: Aripiprazole, brexpiprazole, lurasidone. These have IC50 values over 10 μM. Much safer for the heart.
Here’s the problem: the most commonly prescribed antipsychotics are the moderate-risk ones. Quetiapine alone had over 24 million prescriptions in 2023. Risperidone was close behind at 18.3 million. Even though low-risk options like aripiprazole are growing (up 8.4% annually), many prescribers still default to older, cheaper drugs without checking the heart risk.
When the Risk Multiplies: Drug Combinations
Take one QT-prolonging drug? Risk goes up. Take two? Risk jumps dramatically. The effect isn’t just additive-it’s multiplicative.
Antipsychotics are often paired with other meds that also prolong QT:
- Antibiotics: Moxifloxacin, ciprofloxacin
- Anti-nausea drugs: Ondansetron, metoclopramide
- Antiarrhythmics: Sotalol, amiodarone
- Antidepressants: Citalopram, escitalopram
A 2018 JAMA Internal Medicine study found that combining an antipsychotic with an antidepressant increased torsades risk by 4.3 times. Another study showed that adding ondansetron to an antipsychotic stretched the QT interval by nearly 39 milliseconds-almost double the increase from the antipsychotic alone.
One real case from Cleveland Clinic involved a 68-year-old woman on quetiapine 300 mg daily. She got a prescription for ciprofloxacin for a urinary infection. Within 72 hours, her QTc jumped from 448 ms to 582 ms. She had torsades. She survived-but barely. That’s not rare. Between 2010 and 2022, the FDA logged 128 cases of torsades tied to this exact kind of drug combo.
Who’s Most at Risk?
It’s not just the drugs. Your body matters too. Several factors stack the deck:
- Age over 65: Adds about 15 ms to QTc
- Female sex: Adds 13 ms-women are more vulnerable
- Low potassium (hypokalemia): Below 3.5 mmol/L? Adds 23 ms
- Low magnesium: Often overlooked, but critical for heart rhythm
- Slow heart rate (bradycardia): Under 50 bpm? Adds 18 ms
- Genetics: About 7-10% of Caucasians are poor metabolizers of CYP2D6, meaning drugs build up to dangerous levels
Put together: an elderly woman on risperidone, with low potassium, taking ondansetron for nausea? That’s a perfect storm. The FDA found 78% of torsades cases happen within 72 hours of starting the combo. That’s why early monitoring isn’t optional-it’s life-saving.
What Should Doctors Do?
The American Heart Association and American Psychiatric Association have clear guidelines:
- Get a baseline ECG before starting a moderate- or high-risk antipsychotic.
- Repeat ECG at 1 week and 4 weeks after starting.
- If you’re adding another QT-prolonging drug? Do weekly ECGs for the first month, then monthly.
- Check potassium and magnesium levels regularly-especially in high-risk patients.
- If QTc goes over 500 ms, stop the drug or adjust the combo immediately.
But here’s the gap: in community clinics, ECG compliance is below 35%. Why? Insurance denies coverage. Rural clinics don’t have ECG machines. Doctors are rushed. Patients don’t know to ask. A 2023 NAMI survey found 29% of patients stopped their antipsychotic because they were scared of heart problems-yet 61% said their doctor never explained the actual risk.

What Can Patients Do?
You’re not powerless. Here’s what you can ask for:
- "Is this antipsychotic known to affect my heart?" If your doctor says yes, ask: "Is there a safer alternative?" Aripiprazole or lurasidone might work just as well with far less heart risk.
- "Am I taking any other meds that can prolong QT?" Don’t assume your pharmacist caught it. List everything-even over-the-counter drugs like Pepto-Bismol (contains bismuth subsalicylate, which can affect QT).
- "Can I get a baseline ECG before we start?" Push for it. It’s a simple, non-invasive test.
- "Should I get my potassium and magnesium checked?" Low levels are easy to fix with diet or supplements. Fixing them cuts TdP risk by 82%.
And if you feel dizzy, faint, or notice your heart racing or skipping beats? Don’t wait. Go to the ER. Torsades doesn’t wait.
The Future: Better Tools, Better Outcomes
Change is coming. In May 2024, the FDA approved the Zio XT patch-a wearable ECG monitor designed specifically for psychiatric patients. It records continuously for up to 14 days, catching dangerous spikes that a single ECG might miss. Early studies show 98.7% accuracy in detecting QTc over 500 ms.
By January 2025, the American Psychiatric Association will release new guidelines with a risk calculator. It will weigh your age, sex, meds, electrolytes, and genetics to give you a personalized risk score. By 2026, a genetic test will identify poor metabolizers before they even start a drug.
And financially, things are shifting. Medicare is now tying 2.3% of Part D payments to whether doctors follow QT monitoring rules. Hospitals that ignore this will lose money. That’s pushing change faster than any guideline ever could.
Bottom Line
Antipsychotics save lives. But they can also hurt the heart-especially when mixed with other common drugs. The risk is real, measurable, and preventable. You don’t have to choose between mental health and heart health. You just need to ask the right questions, demand the right tests, and know your options. Low-risk antipsychotics exist. Safe combinations are possible. The tools to prevent death are here. It’s time to use them.





Brian Bell November 14, 2025
Man, I had no idea my zyprexa could mess with my heart like that. My doc just handed me the script like it was aspirin. 😅
Sean Evans November 14, 2025
Typical. Doctors treat mental health like it's a separate system from the body. Wake up. Your heart isn't a bystander. If you're on quetiapine + cipro, you're playing Russian roulette with your ventricles. And don't even get me started on how lazy clinics are about ECGs. This isn't speculation-it's documented carnage. The FDA has data. Hospitals have ECG machines. People are dying because nobody gives a damn until it's too late.
Scarlett Walker November 16, 2025
Thank you for posting this. I’ve been on aripiprazole for 3 years and my cardiologist actually monitors my QT now. It’s a small thing, but knowing I’m not risking my heart makes me feel safer. You’re not alone-ask for the ECG. Ask for the labs. You deserve to be safe while healing.
Ashley Durance November 17, 2025
Of course the risk is preventable. That’s why 90% of these cases happen in patients who never had a baseline ECG. And yes, the doctor didn’t explain it. But let’s be real-most patients won’t read the 47-page FDA warning. They just want the pill to stop the voices. Blaming the doctor is easy. Fixing the system? That’s harder. And nobody’s paying for it.
Ryan Anderson November 18, 2025
Just had my first ECG after starting lurasidone. Took 10 minutes. No pain. No cost (thanks to Medicare). If your doctor says "it’s not necessary," ask them to show you the 2023 APA guidelines. I printed mine. They didn’t argue. 🫡
Anjan Patel November 20, 2025
Ohhhhh so this is why my auntie in Delhi passed away after taking risperidone and metoclopramide for her nausea? She was 72, diabetic, low potassium... and the doctor said "it’s just a pill for stomach." No ECG. No warning. Just... gone. I cried for weeks. Now I scream at every doctor I meet. Don’t let this happen to your mother. Your sister. Your brother. This is not just medicine-it’s murder by negligence.
Hrudananda Rath November 20, 2025
One must observe with detached intellectual rigor that the pharmacological landscape of antipsychotic administration in the post-industrial West has devolved into a grotesque spectacle of therapeutic negligence, wherein the commodification of psychiatric care has rendered the human cardiac rhythm a mere collateral casualty of bureaucratic inertia and pharmaceutical convenience. The hERG channel blockade is not a side effect-it is an epistemological failure of medical episteme.
Scott Saleska November 21, 2025
My mom’s on quetiapine and gets ondansetron every time she’s nauseous. I didn’t know this was dangerous. I just thought she was getting extra help. I’m going to call her doctor tomorrow and ask for a QT check. I’m not waiting for her to collapse before I act.
Eleanora Keene November 22, 2025
Hey everyone-just wanted to say you’re all doing great by learning this. Seriously. Most people just take the pill and move on. But you? You’re asking questions. You’re pushing for tests. That’s how change happens. One person at a time. Keep going. You’re not being paranoid-you’re being smart. And if your doc pushes back? Bring this post. Print it. They’ll listen. 💪
Joe Goodrow November 22, 2025
So now we’re supposed to worry about QT intervals while our soldiers are dying overseas? This is why America’s falling apart. First it’s gender clinics, now it’s heart checks for people on meds for being crazy. We used to just take the pill and shut up. Now we got 17 warnings and a blood test for every damn thing. Wake up, people.
Nathan Hsu November 24, 2025
Let me be clear: this is not just a medical issue-it is a moral crisis. The pharmaceutical industry, in its relentless pursuit of profit, has weaponized ignorance. Doctors, overburdened and underpaid, become unwitting accomplices. Patients, desperate for relief, become easy prey. And the system? It shrugs. But we-the people who read this, who care, who act-we are the antidote. Do not be silent. Do not be passive. Demand. Test. Advocate. Your life depends on it.
Don Ablett November 25, 2025
It is noteworthy that the prevalence of CYP2D6 poor metabolizer status in South Asian populations remains underdocumented in Western literature. While the cited genetic risk applies primarily to Caucasian cohorts, emerging data from Indian genomic studies suggest a higher-than-expected frequency of intermediate metabolizer phenotypes, potentially altering the risk calculus for drugs like risperidone and quetiapine in this demographic. Further population-specific pharmacokinetic modeling is warranted.