When you're breastfeeding, every pill you take feels like it could reach your baby. You might wonder: how do medications even get into breast milk? And if they do, is it safe? The truth is, most medications pass into breast milk in tiny, harmless amounts-but not all of them. Understanding how this works can help you make confident choices without stopping breastfeeding unnecessarily.
How Medications Cross Into Breast Milk
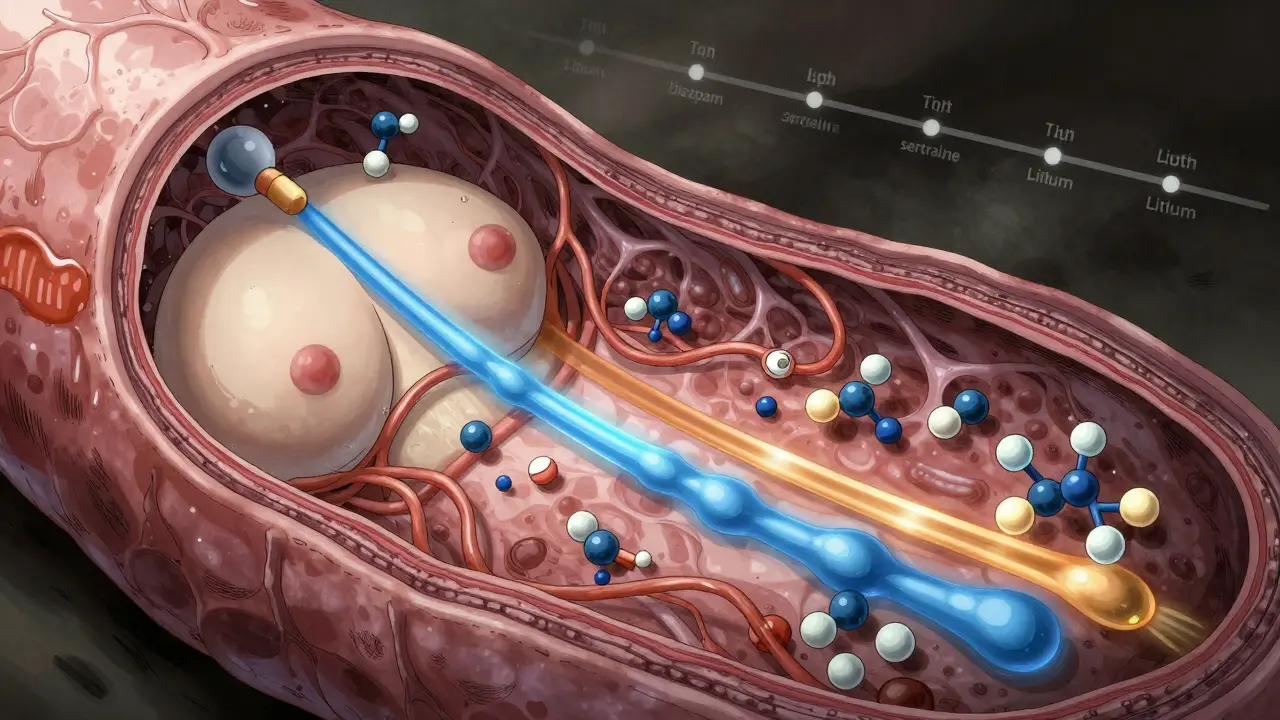
Medications don’t travel to breast milk like a delivery truck. They move naturally, following the rules of physics and biology. About 75% of drugs get into milk through passive diffusion. This means they drift from your bloodstream, where concentrations are higher, into the milk-producing cells in your breasts, where concentrations are lower. It’s like water flowing downhill-no energy needed. The rest enter through special transport systems. Some drugs, like nitrofurantoin or acyclovir, use protein carriers that normally move nutrients or waste. These are called carrier-mediated transport. A few even get actively pumped into milk, though that’s rare. What matters most isn’t just the drug itself, but its physical properties.- Molecular weight: Drugs heavier than 800 daltons (like heparin) barely make it into milk. Lighter ones-like lithium (74 daltons)-move easily.
- Lipid solubility: Fatty drugs (like diazepam) slip through cell membranes better than watery ones (like gentamicin). That’s why diazepam can reach milk levels twice as high as in your blood, while gentamicin stays below 10%.
- Protein binding: If a drug sticks tightly to proteins in your blood (like warfarin, which binds 99% of the time), it can’t float freely into milk. That’s why even strong blood thinners rarely affect babies.
- pKa and ion trapping: Drugs that are weak bases (like amitriptyline) get trapped in milk because breast milk is slightly more acidic than blood. This can make milk concentrations 2 to 5 times higher than in your bloodstream.
Timing Matters: When You Take the Pill
It’s not just what you take-it’s when. Taking your medication right after breastfeeding gives your body time to clear most of it before the next feed. For most drugs, waiting 3 to 4 hours cuts infant exposure by 30-50%. That’s a simple trick that makes a real difference. For drugs with long half-lives-like diazepam, which can stay in a baby’s system for up to 100 hours-timing isn’t enough. If you’re on more than 10 mg a day, your doctor might suggest checking your baby’s blood levels. Signs to watch for: excessive sleepiness, trouble feeding, or unusual fussiness. If those show up, it’s not always the drug-but it’s worth checking.What’s Safe? What’s Not?
Most medications are safe. In fact, 87% of commonly prescribed drugs fall into the “usually compatible” category according to the American Academy of Pediatrics. You don’t need to stop breastfeeding for antibiotics like amoxicillin, pain relievers like ibuprofen, or antidepressants like sertraline. Here’s what the data shows:| Medication | Infant Exposure (% of Maternal Dose) | Typical Risk Level |
|---|---|---|
| Amoxicillin | 1.5% | Safe |
| Gentamicin | 0.1% | Safe |
| Sertraline (Zoloft) | 1-2% | Safe |
| Diazepam | 7.3% | Use with caution |
| Lithium | Up to 10% | Monitor closely |
| Radioactive iodine-131 | Not applicable | Absolute contraindication |
Why So Many Moms Quit-And Why They Don’t Need To
About 42% of U.S. mothers stop breastfeeding before six months. Medication worries are the third most common reason, behind low milk supply and nipple pain. But here’s the catch: studies show 15-30% of those moms stop because they were told a drug was unsafe-when it wasn’t. Take antidepressants. Sertraline is the most prescribed in breastfeeding women, with over 3 prescriptions per 100 mothers each month. Infant exposure is low-1-2% of the mom’s dose-and no major health risks have been proven. Yet, some mothers still stop because they’re scared. The same goes for painkillers. Ibuprofen and acetaminophen are safe, even at high doses. You don’t need to avoid them after a C-section or dental work. But if you’re given a prescription for codeine, that’s different. Codeine turns into morphine in your body, and some people metabolize it too quickly, leading to dangerous levels in breast milk. That’s why it’s no longer recommended.Special Cases: Birth Control, Nuclear Medicine, and More
Not all drugs are created equal. Some have unique risks. Birth control pills with estrogen: If your pill contains more than 50 mcg of ethinyl estradiol, it can slash your milk supply by 40-60% in just three days. That’s why progestin-only pills are the go-to for breastfeeding moms. Nuclear medicine: Tests like VQ scans use radioactive tracers. Tc-99m MAA requires you to stop breastfeeding for 12-24 hours. But FDG-PET scans? You can keep nursing. Less than 0.002% of the dose ends up in milk. Bromocriptine: This drug shuts down milk production. It’s used to stop lactation after loss or adoption. If you’re trying to breastfeed, avoid it.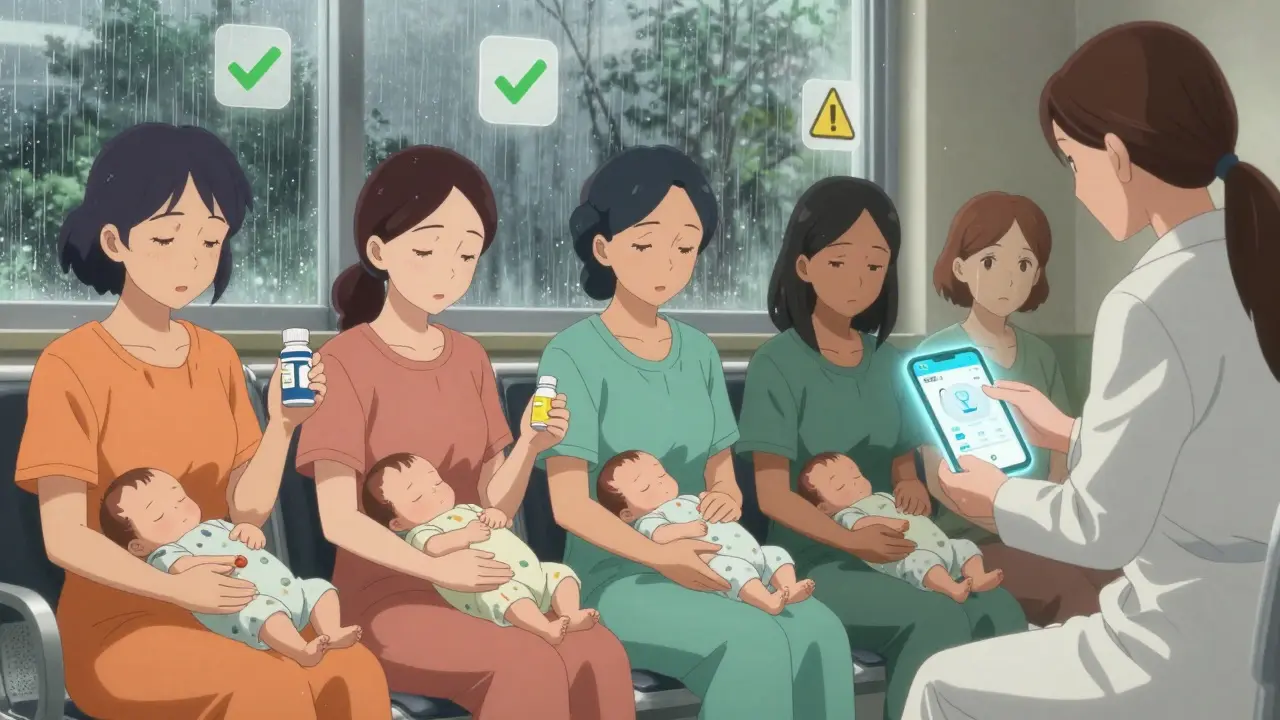
What You Should Do
You don’t need to guess. Here’s what works:- Always tell your doctor you’re breastfeeding-before they write any prescription.
- Use trusted resources like the InfantRisk Center’s LactMed app (updated 2023) or the CDC’s breastfeeding guidelines.
- For SSRIs or other psych meds, monitor your baby for irritability or poor feeding. If you see it, check levels at 2 weeks postpartum.
- Don’t stop breastfeeding because of a medication unless a specialist says so. Less than 2% of drugs truly require it.
- Take meds right after a feed, wait 3-4 hours, then nurse again.
What’s Changing in 2025
The FDA now requires all new drugs to include breastfeeding data on their labels. That’s a big step forward. And research is accelerating. The NIH-funded MOMS study, wrapping up in 2025, will set clear safety thresholds for 50 priority medications-giving doctors and moms hard numbers, not just opinions. The bottom line? Breastfeeding while on medication isn’t a gamble. It’s a science. And the science says: you can usually do both.Can I take painkillers while breastfeeding?
Yes. Ibuprofen and acetaminophen are safe at standard doses. They transfer minimally into breast milk and have no known effects on infants. Avoid codeine and tramadol, as they can convert to morphine in your body and pose a risk to your baby.
Is sertraline safe for breastfeeding mothers?
Yes. Sertraline is one of the safest antidepressants for breastfeeding. Infant exposure is only 1-2% of the mother’s dose, and studies show no significant side effects in babies. It’s the most commonly prescribed antidepressant for nursing mothers.
Do antibiotics affect my baby’s gut?
Some antibiotics, like amoxicillin, may cause mild loose stools or fussiness in babies, but this is rare and usually temporary. The benefits of treating infection far outweigh the small risk. Probiotics can help if your baby develops mild digestive upset.
Can I breastfeed after a CT scan with contrast?
Yes. Iodinated contrast agents used in CT scans do not transfer into breast milk in any meaningful amount. Major organizations like the ACR and AAP say you can breastfeed normally after the scan. No pumping and dumping is needed.
What if I need a medication that’s not safe?
If a medication is truly unsafe, your doctor can often switch you to a safer alternative. Rarely, you may need to pause breastfeeding temporarily while taking the drug. In those cases, pump and discard milk to maintain supply, then resume once the drug clears. Always consult a lactation specialist or pharmacist before stopping.
Does pumping and dumping help reduce baby’s exposure?
Only if you’re doing it to avoid feeding during peak drug levels. Pumping and dumping doesn’t speed up drug clearance from your body-it just removes milk that’s already made. Timing your doses after feeds is far more effective than pumping.
Are herbal supplements safe while breastfeeding?
Many herbal supplements haven’t been studied in breastfeeding women. Some, like sage or peppermint in large amounts, can reduce milk supply. Others may contain unregulated ingredients. Always check with a provider before using them.
How do I know if my baby is reacting to a drug in my milk?
Watch for changes: unusual sleepiness, poor feeding, irritability, rash, or diarrhea. If you notice any, note the timing-did it start after you began a new medication? Talk to your pediatrician. In most cases, it’s not the drug-but it’s worth checking.





Randolph Rickman December 16, 2025
Just wanted to say this post is a game-changer. I was ready to quit breastfeeding after my doc prescribed me amoxicillin, but now I know it's basically harmless. My baby's fine, I'm sleeping better, and I didn't have to pump and dump like some mythic ritual. Thank you for the science, not the fear.
Also, timing meds after a feed? Genius. I started doing that and my toddler stopped waking up at 3am like he was being poisoned. It's not magic, it's just biology working right.
Mike Smith December 17, 2025
As a pediatric nurse and a breastfeeding mother, I cannot stress enough how vital this information is. Too many women are unnecessarily weaning due to misinformation. The data on sertraline is particularly reassuring-infant exposure under 2% with no documented clinical effects in over 15 years of monitoring. This isn't just safe; it's standard of care.
Always consult LactMed. Never rely on Google. And if your provider says 'avoid breastfeeding' without citing a source, ask them to show you the evidence. Most of the time, they can't.
Aditya Kumar December 18, 2025
lol
Colleen Bigelow December 19, 2025
They’re lying. Big Pharma doesn’t want you to know this. They put toxins in everything-your meds, your baby’s formula, even the air you breathe. That ‘safe’ sertraline? It’s just a slow-acting poison disguised as help. They’ve been doing this since the 1980s. The FDA? Bought and paid for. They’ll tell you it’s ‘1-2%’ but they won’t tell you what that 1-2% does to a developing brain over years. You think your baby’s fine now? Wait until they’re 12 and can’t focus in school. Then ask yourself-was it worth it?
And don’t get me started on glyphosate in the milk supply. You’re all just sheep.
STOP. BREASTFEEDING. NOW.
Billy Poling December 20, 2025
While I appreciate the thoroughness of this article, I must respectfully point out that the statistical framing of infant exposure percentages, while mathematically accurate, may inadvertently minimize the potential for cumulative bioaccumulation in neonates with immature hepatic and renal clearance mechanisms. The assumption that 1-2% of maternal dose equates to clinical insignificance presumes a homogeneous population of healthy term infants, which does not account for preterm neonates, infants with metabolic disorders, or those with polymorphisms in cytochrome P450 enzymes. Furthermore, the reliance on LactMed, while commendable, is predicated upon a database that is inherently retrospective and observational, lacking controlled longitudinal studies. One must also consider the potential for epigenetic modulation by low-dose xenobiotics during critical windows of neurodevelopment, which may not manifest until adolescence. Therefore, while the general conclusion may be statistically valid, the clinical application demands a far more nuanced, individualized risk-benefit analysis that accounts for genetic, environmental, and developmental variables beyond the scope of this summary.
Elizabeth Bauman December 22, 2025
Okay, but let’s be real-why is it that every single time a woman tries to breastfeed while on meds, the medical community says ‘it’s fine’ but then when she has a baby with a rash or a sleep issue, they blame her diet, her stress, her ‘vibes’? I’ve seen this too many times. The science says ‘safe,’ but the system still makes moms feel guilty. That’s not science. That’s gaslighting.
And yes, I took sertraline. My baby was fine. But I still had to beg my pediatrician to believe me when I said ‘no, he’s not colicky-he’s just sleepy.’ They didn’t even ask if I was on meds. That’s the real problem.
Dylan Smith December 23, 2025
So I took ibuprofen after my c section and my baby got super fussy for like 2 days and I thought it was the meds but then I realized I was just sleep deprived and my milk was low and I felt like a failure and now I'm scared to take anything ever again even though I know it's probably fine I just need someone to tell me it's okay to not be perfect
also why does everyone say 'it's safe' like that's enough when I'm scared of hurting my kid
Ron Williams December 24, 2025
Coming from a dad whose partner breastfed while on meds for postpartum anxiety-this post saved our sanity. We didn’t know any of this. We thought we had to choose between mental health and feeding our kid. Turns out, we didn’t. We just needed someone to lay it out plainly.
Also, the part about timing meds after a feed? We started doing that and our baby slept longer stretches. No magic, just smart timing. We’re still breastfeeding at 14 months. And yeah, we still take meds. No shame.
Also, if you’re reading this and you’re scared-you’re not alone. We were too. But you don’t have to suffer in silence.
Kitty Price December 25, 2025
Thank you for this!! 🙏
Just took sertraline for 8 months while nursing my second. Baby is now 2 and thriving. No issues. I wish I’d had this post when I started. So many moms are told to stop when they don’t need to. You’re not broken for needing help. You’re brave for trying to do it all.
Also-pumping and dumping is a myth. Just time your meds after a feed and chill. Your baby will be fine. 💪🍼
Kim Hines December 26, 2025
I took lithium for bipolar during breastfeeding. My kid’s fine. But I had weekly blood tests for 6 months. And I pumped and dumped for the first 4 hours after each dose. It wasn’t easy. But I didn’t stop. And I didn’t regret it. This post got it right. It’s not about fear. It’s about management.
Joanna Ebizie December 26, 2025
Ugh. You people are so naive. You think it’s ‘safe’ because some doctor said so? I’ve seen babies turn purple from meds in breast milk. You think your kid’s fine now? Wait till they’re 5 and have autism. Then come back here and tell me it was worth it. You’re playing Russian roulette with your child’s brain and calling it ‘science.’
SHAMSHEER SHAIKH December 26, 2025
As a medical researcher from India, I must commend the depth of this article. The pharmacokinetic principles outlined-passive diffusion, carrier-mediated transport, ion trapping-are accurately described and clinically relevant. In our own study at AIIMS, we observed that even with high maternal serum levels of amoxicillin, infant plasma concentrations remained below 0.5 mcg/mL, well below the MIC for common pathogens. Furthermore, the emphasis on timing and the avoidance of estrogen-containing contraceptives aligns with WHO guidelines from 2022. However, I would add that in populations with high rates of G6PD deficiency (common in South Asia), certain drugs like sulfonamides require extra caution, even if they are generally considered safe. This is a vital resource for global lactation support.
James Rayner December 28, 2025
It’s strange, isn’t it? We’re told to trust science, but when it comes to our bodies and our babies, we’re made to feel like we’re breaking a sacred rule if we take anything. We’re taught to be pure, to be perfect, to be self-sacrificing-but no one tells us that healing ourselves is part of being a good mother. Maybe the real danger isn’t the drug in the milk… maybe it’s the guilt we carry for needing help.
I took sertraline. My baby smiled at 6 weeks. He’s now a happy 3-year-old who loves pancakes and dinosaurs. I didn’t choose between being a mom and being well. I chose to be both. And I don’t regret it. Not even a little.
Souhardya Paul December 29, 2025
Just wanted to add something practical: if you're on a med that's not on LactMed, ask your pharmacist to run a literature search. Most hospital pharmacies have access to UpToDate and Micromedex-they’ll give you a 2-paragraph summary in 10 minutes. I’ve done this for my patients on gabapentin, tramadol, and even CBD oil (yes, really). It’s not magic, it’s just asking the right person. And if your doctor doesn’t know, that’s okay-just say ‘I need to know if this is safe for breastfeeding, can we look it up together?’ You’re not being difficult. You’re being responsible.