Medication Dry Mouth Risk Calculator
Your Dry Mouth Risk Assessment
Risk Assessment
Your Risk Level
Based on your current medications
Select your medications to see your risk assessment.
Almost one in three people taking prescription meds experience dry mouth - not just discomfort, but a real threat to their teeth, eating, and sleep. It’s not normal aging. It’s not just drinking too little water. It’s your medicine. If you’re constantly reaching for a bottle of water, struggling to swallow food, or waking up with a cottony throat, you’re not alone. And it’s not something you have to live with.
Why Your Medication Is Killing Your Saliva
Your saliva doesn’t just help you talk and chew. It’s your mouth’s natural defense system. It washes away food, neutralizes acids, and protects your teeth from decay. When your body stops making enough of it, everything changes. And the biggest culprit? Medications. More than 1,100 common prescriptions are known to cause dry mouth, according to the American Academy of Oral Medicine. The main reason? They block acetylcholine, a chemical your body uses to tell your salivary glands to produce saliva. This is called an anticholinergic effect. About 68% of drugs that cause dry mouth work this way. Think about common meds: antidepressants like amitriptyline, bladder drugs like oxybutynin, antihistamines like Benadryl, and even some blood pressure pills. These aren’t rare or experimental drugs - they’re everyday prescriptions. And the more you take, the worse it gets. People on three or more medications are over twice as likely to have severe dry mouth compared to those on just one.Which Medications Are the Worst Offenders?
Not all drugs affect saliva the same way. Some are far more likely to dry you out than others.- Bladder medications: Oxybutynin (Detrol) causes dry mouth in over 70% of users. Tolterodine (Detrol) is almost as bad at 62%. Solifenacin (Vesicare) is a bit better, but still hits nearly half of users.
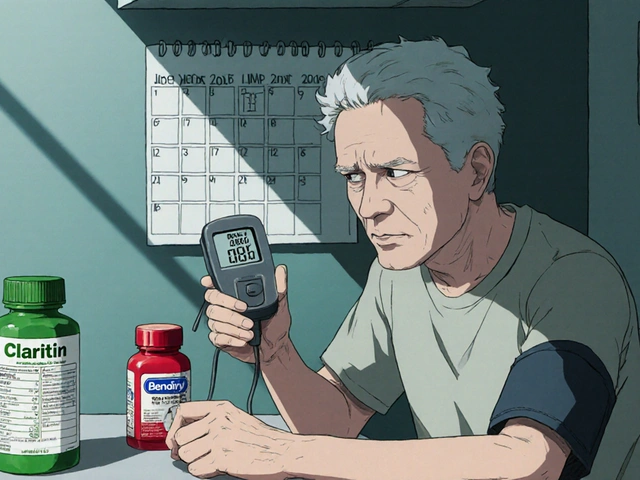
- Antihistamines: First-gen ones like diphenhydramine (Benadryl) cause dry mouth in 58% of people. Second-gen ones like loratadine (Claritin)? Only 12%.
- Antidepressants: Tricyclics like amitriptyline hit 63% of users. SSRIs like sertraline? Around 31%. Big difference.
- Antipsychotics: Haloperidol causes dry mouth in 54% of patients. Aripiprazole? Only 37%.
What Dry Mouth Actually Does to Your Mouth
Dry mouth isn’t just uncomfortable. It’s dangerous. Without saliva, bacteria run wild. Acid builds up. Your teeth start to dissolve. Studies show untreated dry mouth can increase tooth decay by 300% within just 12 months. That’s not a guess - it’s from the Cleveland Clinic’s clinical data. People with chronic dry mouth are far more likely to get:- Cavities on the roots of teeth (root caries)
- Thrush (a fungal infection)
- Cracked lips and mouth sores
- Difficulty wearing dentures
- Frequent bad breath

What No One Tells You About Managing It
You can’t just sip water all day and expect it to fix things. Water doesn’t replace saliva. It just washes over the problem. The American Dental Association recommends a four-step plan:- Review your meds with your doctor. In 42% of cases, switching to a non-drying alternative works. For example, switching from diphenhydramine to loratadine cuts dry mouth risk by 80%. Don’t stop meds yourself - talk to your prescriber.
- Use a salivary stimulant. Pilocarpine (Salagen) and cevimeline (Evoxac) are FDA-approved drugs that actually boost saliva production. In clinical trials, pilocarpine increased flow by 63% in two weeks. Cevimeline, approved in April 2023, showed 72% improvement.
- Use prescription-strength oral moisturizers. Over-the-counter sprays and gels don’t cut it. Products like Biotene Dry Mouth Oral Rinse contain enzymes that mimic natural saliva. Independent tests show they provide relief for up to 7 hours - not the 4 hours older versions offered.
- See your dentist every 3 months. Standard six-month cleanings aren’t enough. With dry mouth, you need checkups every 90 days to catch decay early.
Real People, Real Results
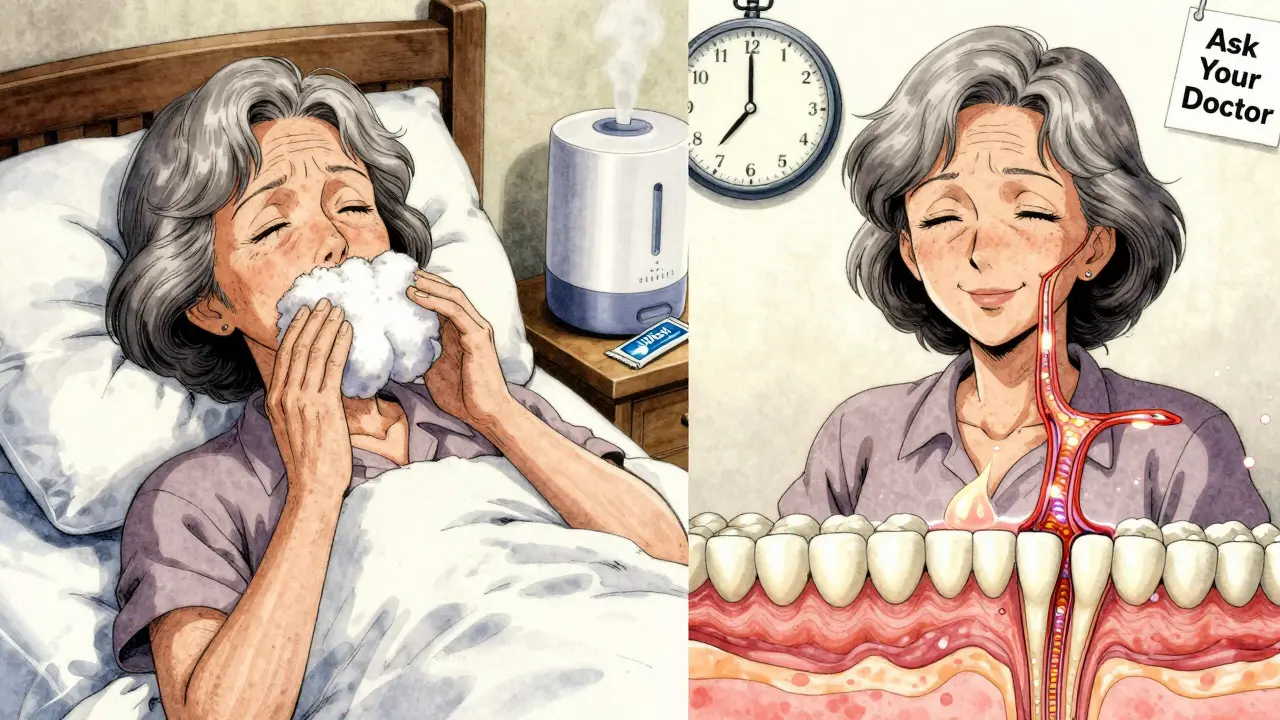
A 72-year-old woman in York, on amitriptyline for nerve pain, was waking up 3-4 times a night with a parched throat. She couldn’t eat dry toast or swallow pills without water. Her dentist found two early root cavities. After switching to a different antidepressant and starting pilocarpine, her saliva flow returned to 80% of normal within six weeks. Her cavities stopped growing. Another man, on four meds including oxybutynin and a blood pressure pill, started using Biotene’s new enzyme-based gel five times a day and rinsed with a fluoride mouthwash. Within three months, his dentist reported zero new decay - a first in five years. The key? Coordination. When dentists and doctors talk to each other, complications drop by 57%. But only 28% of primary care doctors routinely ask about dry mouth during med reviews.What You Can Do Today
You don’t need to wait for your next appointment. Start here:- Track your meds. List every pill, patch, or injection you take - including OTC ones like antihistamines or sleep aids.
- Ask your doctor: "Could any of these be causing dry mouth? Is there a less drying alternative?" Be specific. Mention your symptoms.
- Buy a fluoride rinse. Use it after brushing. It helps protect enamel when saliva is low.
- Chew sugar-free gum with xylitol. It stimulates saliva naturally. Look for gum with at least 1g of xylitol per piece.
- Use a humidifier at night. Especially if you breathe through your mouth while sleeping.
- Stop sipping sugary drinks. They feed the bacteria that cause decay. Stick to water or unsweetened tea.
The Bigger Picture
Dry mouth from meds is a growing crisis. The market for dry mouth products is now worth over $1.2 billion and growing. But most patients still suffer in silence. Only 31% get proper treatment. The CDC says 76% of cases are in people over 65 - the group most likely to be on multiple meds. New research is pushing change. The NIH launched a $15.7 million project in January 2024 to find non-drying alternatives for bladder meds. Health systems are starting to pair pharmacists with dentists to catch problems early. By 2027, the ADA predicts all new medications will need a dry mouth risk warning. That’s progress. But you don’t have to wait.When to Worry
If you have dry mouth and also notice:- White patches or sores in your mouth
- Teeth feeling rough or sensitive
- Difficulty swallowing or speaking
- Constant thirst even after drinking
Can dry mouth from medication be reversed?
Yes, in many cases. If the medication causing it can be switched to a less drying alternative, saliva production often returns. Even if you can’t stop the drug, treatments like pilocarpine or cevimeline can restore up to 70% of normal saliva flow. The sooner you act, the better your chances of preventing permanent damage.
Is dry mouth a sign of something worse?
Sometimes. While most cases are caused by meds, dry mouth can also signal Sjögren’s syndrome, diabetes, or nerve damage. If your dry mouth started suddenly, isn’t linked to a new medication, or comes with joint pain, eye dryness, or fatigue, see your doctor for further testing.
Why doesn’t my doctor mention this?
Most doctors aren’t trained to link dry mouth to oral health. A 2023 survey found only 28% of primary care physicians screen for it during med reviews. They focus on the main reason you’re on the drug - not the side effects. That’s why you need to speak up. Bring it up yourself. Bring your list of meds. It’s your right to know.
Are natural remedies like aloe vera or coconut oil effective?
They might help with comfort, but they don’t fix the root cause. Aloe vera gel can soothe sore gums, and coconut oil pulling may reduce bacteria. But if your salivary glands aren’t producing saliva, no oil or herb will restart them. Prescription stimulants and enzyme-based moisturizers are the only proven methods to restore protection.
Will my insurance cover dry mouth treatments?
It depends. Most dental plans don’t cover prescription saliva stimulants like pilocarpine - only 43% do. Medical insurance might cover them if prescribed for a diagnosed condition. Over-the-counter products like Biotene are rarely covered. Ask your pharmacist about patient assistance programs - many drugmakers offer discounts.
How long does it take to see improvement?
With lifestyle changes like chewing xylitol gum and using moisturizers, you might feel better in days. But real improvement - like increased saliva production from pilocarpine or cevimeline - usually takes 2 to 4 weeks. Full protection against decay requires consistent use over 3 to 6 months. Patience and persistence matter.




astrid cook January 26, 2026
This is why people are dying from simple prescriptions. No one tells you this stuff until your teeth are dust. I had to get a full mouth reconstruction at 58 because my doctor never asked about my meds. Now I’m on a $12k payment plan. And they wonder why healthcare costs are insane.
Someone needs to sue Big Pharma for this. It’s not a side effect-it’s a betrayal.
Kirstin Santiago January 28, 2026
I appreciate how detailed this is. My mom’s on oxybutynin and didn’t realize her constant sore throat and cavities were from the pill. We switched her to mirabegron last month-her dentist actually noticed the difference in just 6 weeks. Saliva looks like it’s coming back. Small wins matter.
Also, xylitol gum is a game changer. I keep a pack in my purse now. No more sticky mouth after lunch.
Kathy McDaniel January 30, 2026
OMG I thought I was just getting old 😅 I’ve been sipping water all day since my anxiety med started and never connected it to my tooth pain. Just bought Biotene rinse and some xylitol gum-fingers crossed this helps. Thanks for the real talk, this post saved me from a dental nightmare.
Patrick Merrell January 31, 2026
They’re hiding this on purpose. You think it’s an accident that 1100+ drugs cause dry mouth? No. It’s profit. Saliva stimulants cost pennies. But they sell you $30 sprays and $200/month prescriptions instead. The FDA’s in bed with pharma. Wake up.
And don’t get me started on how dentists are paid to ignore this. They want you coming back for crowns, not preventing them.
Murphy Game February 2, 2026
Of course they don’t warn you. You think your doctor cares about your teeth? They care about your insurance code. I’ve been on 5 meds for 4 years. My dentist found 8 cavities in one visit. He said, "You’re on something that kills saliva, right?" I said, "How did you know?" He said, "I see it every Tuesday."
They don’t train doctors to ask. They train them to write scripts. You’re on your own.
John O'Brien February 3, 2026
Bro this is real. My aunt was on amitriptyline for 8 years and never told her dentist. Got a root canal on every molar. Now she’s on Celexa and using pilocarpine. Her teeth are actually white again. Stop suffering in silence. Talk to your prescriber. Bring this article. If they blow you off, find a new doctor.
Also-fluoride rinse after brushing. Non-negotiable.
Andrew Clausen February 3, 2026
Incorrect. The ADA does not recommend "reviewing meds with your doctor" as a primary intervention for dry mouth. That’s a misrepresentation of their guidelines. The ADA emphasizes oral hygiene, saliva substitutes, and behavioral modifications-not medication substitution, which is outside dental scope.
Also, pilocarpine has significant side effects: sweating, nausea, blurred vision. It’s not a magic bullet. This post oversimplifies a complex pharmacological issue.
Anjula Jyala February 3, 2026
Anticholinergic burden is the real issue here. Polypharmacy in elderly populations creates cumulative cholinergic suppression. Salivary acinar cells express M3 receptors-blockade = hyposecretion. You need to assess CYP450 interactions too. Most patients are on CYP2D6 substrates which amplify anticholinergic effects.
Non-pharmacological interventions are adjunctive. Only cholinergic agonists like cevimeline directly target receptor upregulation. Xylitol gum is placebo level for true xerostomia.
Robin Van Emous February 5, 2026
Thank you for writing this with so much care. I’m from a rural area and my grandma didn’t know her dry mouth was from her blood pressure pill. We took her to a pharmacist who helped her switch. Now she’s eating apples again. No more nighttime coughing.
It’s scary how little we’re taught about this. But people like you-sharing real info, not ads-make a difference. Please keep doing this.
astrid cook February 5, 2026
Robin Van Emous just said "she’s eating apples again" like that’s some miracle. You think a grandma eating fruit fixes systemic drug-induced organ suppression? No. It’s a bandaid. The system is broken. We’re just lucky she didn’t lose all her teeth before someone cared enough to ask.
And don’t pat yourself on the back for being "nice." Fix the system. Not the symptoms.