When you’re pregnant or breastfeeding and need psychiatric medication, you’re not just managing your mental health-you’re managing two lives. That’s why getting your OB/GYN and psychiatrist on the same page isn’t just helpful-it’s essential. Too often, women are caught in the middle: their OB/GYN says one thing about medication safety, their psychiatrist says another, and no one talks to each other. The result? Unnecessary fear, medication stops that lead to relapse, or worse-hospitalization after birth.
Why Coordination Isn’t Optional
About 1 in 5 women experience depression, anxiety, or bipolar disorder during pregnancy or after giving birth. Left untreated, these conditions raise the risk of preterm birth by 40%, low birth weight by 30%, and even difficulties bonding with the baby. But the fear of harming the baby often leads women to stop their meds. And that’s where the real danger lies. The American College of Obstetricians and Gynecologists (ACOG) made this clear in their 2023 guidelines: the most dangerous medication during pregnancy is no medication when it’s needed. A 2022 study of nearly 9,000 pregnant women found that those who got coordinated care were 57% less likely to stop their antidepressants and had 37% fewer postpartum depression symptoms than those who didn’t. Coordination isn’t about one doctor deferring to the other. It’s about both working together using the same data, same goals, and same language. When they do, outcomes improve dramatically.Which Medications Are Safest During Pregnancy?
Not all psychiatric meds are created equal when you’re pregnant. The goal is to use the lowest effective dose of the safest option. For depression and anxiety, sertraline and escitalopram are first-line choices. Why? Because decades of data show they cross the placenta minimally and have the lowest risk of birth defects. Sertraline, for example, increases the absolute risk of heart defects from 1% (baseline) to just 1.5%. That’s a tiny increase-far less risky than the consequences of untreated depression. Avoid paroxetine. It’s linked to a higher risk of heart defects and is no longer recommended as a first choice. Fluoxetine is also used, but its long half-life can mean it sticks around in the baby’s system after birth, which isn’t ideal. For bipolar disorder, lithium and lamotrigine are preferred. Valproate? Absolutely not. It carries a 10.7% risk of major birth defects-nearly five times higher than average. If you’re on valproate and planning pregnancy, switching under psychiatrist supervision is critical. For anxiety, benzodiazepines like lorazepam should be avoided long-term. They can cause withdrawal in newborns. If absolutely needed, use the lowest dose for the shortest time-with weekly check-ins from your psychiatrist. The National Pregnancy Registry for Psychiatric Medications tracks over 15,000 pregnancies. Their latest data confirms: SSRIs like sertraline show no significant rise in major malformations-except for paroxetine. This isn’t guesswork. It’s science.How Pregnancy Changes How Medications Work
Your body changes dramatically during pregnancy. Blood volume increases by 40-50%. Your kidneys filter faster. Liver enzymes that break down meds become more active-especially in the third trimester. That means your usual dose might not be enough anymore. For example, sertraline clearance increases by up to 60% in late pregnancy. A woman stable on 50mg in her first trimester might need 100mg by week 32. If her OB/GYN doesn’t know this, they might assume she’s relapsing-and up the dose too late. That’s why communication matters. Your OB/GYN should know your medication, your dose, and your target blood levels. Your psychiatrist should know your pregnancy stage, your symptoms, and your lab results. Without that, you’re flying blind.What Happens After Baby Is Born?
Breastfeeding changes the game again. Most antidepressants pass into breast milk in tiny amounts. Sertraline and escitalopram are the safest here too-they’re found in breast milk at levels below 1% of the mother’s dose. The baby’s exposure is often lower than what they’d get from a single infant dose. Lithium? That’s trickier. It concentrates in breast milk and can build up in the baby’s system. If you’re on lithium, your baby’s levels need to be monitored. Many women switch to lamotrigine or continue sertraline instead. The key? Don’t stop your meds after birth because you’re breastfeeding. The risk of relapse in the first 3 months postpartum is higher than at any other time. One study found 60% of women who stopped antidepressants after delivery had a major depressive episode within 6 months.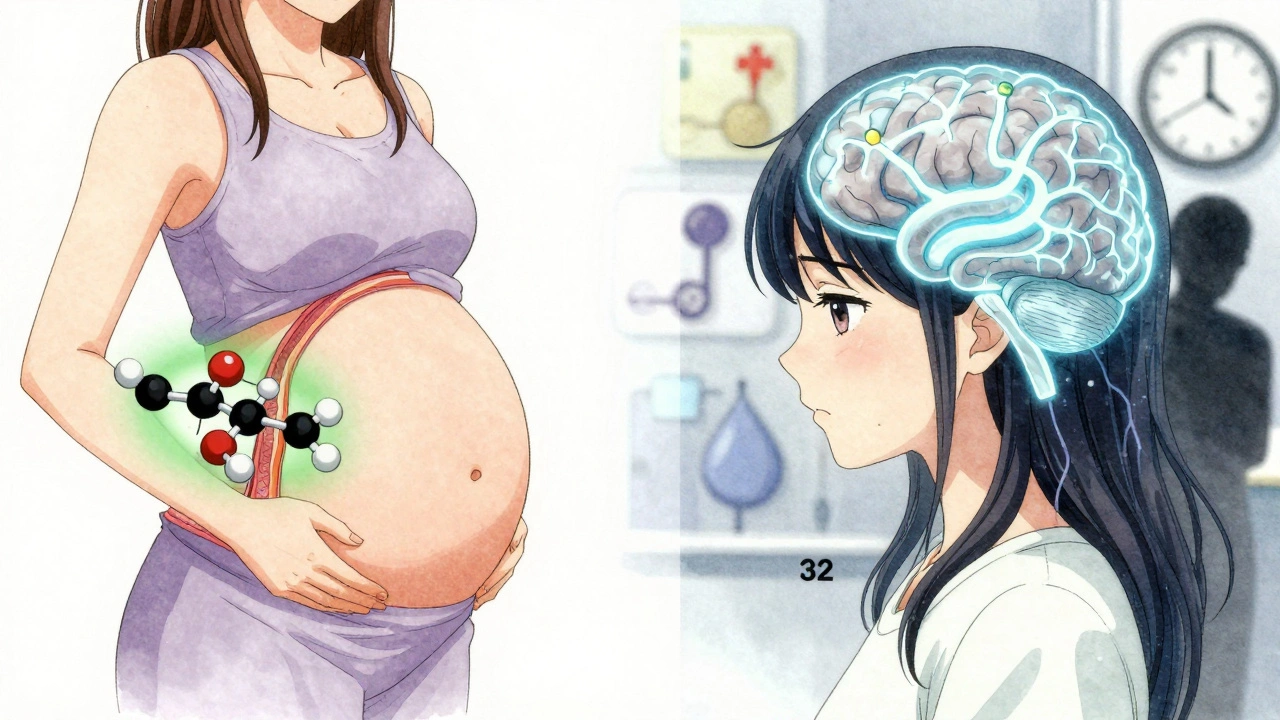
The 5-Step Coordination Protocol
Here’s what real coordination looks like, step by step:- Preconception Planning - If you’re trying to get pregnant, schedule a joint meeting with both providers at least 3-6 months ahead. This is when you adjust meds, switch from risky drugs, and set a plan. Don’t wait until you’re pregnant.
- First Trimester Check-In - By week 8-10, both providers should review your medication plan. This is when you confirm dosing, check for side effects, and document risks using tools like ACOG’s Reproductive Safety Checklist.
- Monthly Monitoring - For stable cases, check in every 4 weeks. For unstable cases (new symptoms, dose changes), weekly communication is needed. Use shared templates that include protein binding, placental transfer, and lactation risk scores.
- Third Trimester Adjustments - Around week 20, your psychiatrist should reassess your dose. Many women need increases due to faster metabolism. Your OB/GYN should alert the psychiatrist if symptoms return or if labs show changes.
- Postpartum Handoff - Within 72 hours of delivery, your psychiatrist should be notified. If you’re breastfeeding, confirm your meds are safe. If you’re not, discuss whether to continue, taper, or switch.
What to Do When Your Providers Don’t Talk
Too many women report getting conflicting advice. One provider says, “It’s safe.” The other says, “Stop it.” That’s not care-that’s chaos. If your OB/GYN and psychiatrist aren’t communicating, here’s what you can do:- Ask your OB/GYN to send a secure message to your psychiatrist using your EHR system. Most clinics now have direct messaging.
- Request a joint appointment. Some hospitals offer “warm handoff” video visits where both providers talk together in real time.
- Bring a printed summary of your meds, doses, and dates to every appointment. Include the name of your psychiatrist and their contact info.
- Use ACOG’s Reproductive Safety Checklist. It’s free, easy to use, and gives both providers a common language.
Barriers-and How to Overcome Them
Coordination isn’t always easy. Here are the big hurdles:- Electronic records don’t talk - 67% of providers say their OB/GYN and psychiatric systems don’t share data. Solution: Print and hand-carry your medication list.
- Insurance delays - 57% of patients wait over 14 days for prior authorization to see a psychiatrist. If you’re pregnant, ask for an emergency referral. Many insurers fast-track these.
- Stigma - Some OB/GYNs still think mental health isn’t their job. But ACOG says it is. If your provider resists, ask for a referral to a maternal-fetal medicine specialist-they’re trained in this.

Real Stories, Real Outcomes
One woman in New York stopped sertraline after her OB/GYN told her it was “risky.” She developed severe postpartum depression, couldn’t care for her newborn, and ended up hospitalized. Her psychiatrist later said: “She was stable for 2 years before pregnancy. There was no reason to stop.” Another woman in California kept her sertraline dose, had weekly check-ins with both providers, and breastfed without issue. Her baby’s blood levels were checked at 2 weeks-undetectable. She returned to work at 12 weeks, feeling like herself for the first time in years. The difference? Coordination.What’s Changing Now
The system is improving. In 2023, Epic Systems launched a Perinatal Mental Health Module that automatically alerts psychiatrists when an OB/GYN prescribes antidepressants. Over 1,200 hospitals now use it. The FDA updated medication labels in early 2024 to include coordination notes. Sertraline’s label now says: “Coordination with obstetric provider recommended for dose adjustment beginning at 20 weeks.” That’s huge-it means even the drug makers are pushing for teamwork. By 2025, ACOG will roll out AI tools that predict which women are most likely to relapse based on genetics, past episodes, and stress levels. This isn’t sci-fi-it’s coming fast.What You Can Do Today
If you’re pregnant or planning to be:- Don’t wait until you’re in crisis to get help.
- Ask your OB/GYN: “Do you work with a psychiatrist for medication management during pregnancy?”
- If you’re already on meds, don’t stop. Talk to both providers now.
- Get a copy of your medication list and bring it to every appointment.
- Use ACOG’s Reproductive Safety Checklist-it’s simple, free, and gives you control.







Audrey Crothers December 11, 2025
OMG this is SO needed 😭 I stopped my sertraline during my first pregnancy bc my OB said 'better safe than sorry'-turned into a postpartum nightmare. I didn’t sleep for 3 weeks, cried every day, felt like I was failing my baby. This post? Pure gold. I wish I’d had it then.
Adam Everitt December 12, 2025
hmm… interesting. so we’re now treating pregnancy like a pharmacokinetic lab experiment? i mean, sure, science says sertraline is ‘safe’… but is it really? what about epigenetic effects? no one talks about that. just sayin’.
wendy b December 14, 2025
Let me be perfectly clear: the pharmaceutical-industrial complex has weaponized maternal guilt to sell SSRIs. The ‘1 in 5 women’ statistic? Manufactured. The ‘57% less likely to stop meds’? Sponsored by Big Pharma. ACOG’s guidelines? A corporate policy document masquerading as medicine. Don’t be fooled.
Real mothers don’t need pills. They need community. They need rest. They need to be held. Not dosed.
Reshma Sinha December 16, 2025
THIS IS THE FUTURE OF MATERNAL MENTAL HEALTH CARE! 🚀 We’re talking integrated care pathways, pharmacogenomic alignment, and longitudinal perinatal psychosocial risk stratification! If your OB/GYN isn’t synced with your psychiatrist via EHR interoperability protocols, you’re operating in a legacy system. Time to advocate for a care coordination dashboard-preferably with real-time lactation risk scoring! #PerinatalPrecisionMedicine
Lawrence Armstrong December 16, 2025
Just wanted to add-my wife was on 75mg sertraline pre-pregnancy. By week 30, she was crashing. OB didn’t know about the metabolism shift. Psychiatrist finally stepped in after she cried for 2 hours straight during a visit. We printed the ACOG checklist, handed it to both docs, and boom-dose bumped to 125mg. She’s been stable since. No drama. Just science.
Also, her baby’s blood levels at 2 weeks? Undetectable. Zero issues. 🤝
Donna Anderson December 16, 2025
thank you thank you thank you!! i was so scared to tell my ob i was on meds bc she looked at me like i was crazy. then i brought the checklist and she was like ‘ohhhhh we do this all the time!’ 😭 i cried in the parking lot. you’re right-coordination isn’t optional, it’s survival.
Nathan Fatal December 18, 2025
There’s a deeper truth here that no one’s naming: our healthcare system treats mental health as an afterthought-until it’s too late. The fact that a woman has to beg her OB and psychiatrist to talk to each other is a systemic failure. This isn’t about meds or dosing-it’s about dignity. A pregnant woman shouldn’t have to become a medical case manager just to stay alive. We’ve built a system that expects mothers to fix broken infrastructure with their own emotional labor. That’s not care. That’s exploitation.
And yes, sertraline is safer than paroxetine. But the real victory isn’t in choosing the least toxic drug-it’s in building a system where no one ever has to choose at all.
Stacy Foster December 18, 2025
Wait… so you’re telling me the FDA and ACOG are now pushing psychiatric meds during pregnancy because they’re getting paid off by Big Pharma? And the ‘AI tools coming in 2025’? That’s not innovation-that’s surveillance. They’re tracking your hormones, your genetics, your mood swings… all to keep you medicated. This isn’t healthcare. It’s a control mechanism. Don’t be the next test subject.