Metformin Safety Risk Calculator
Assess your metformin safety
Answer these questions to determine if metformin is safe for you based on current guidelines. This tool is for informational purposes only and not a substitute for professional medical advice.
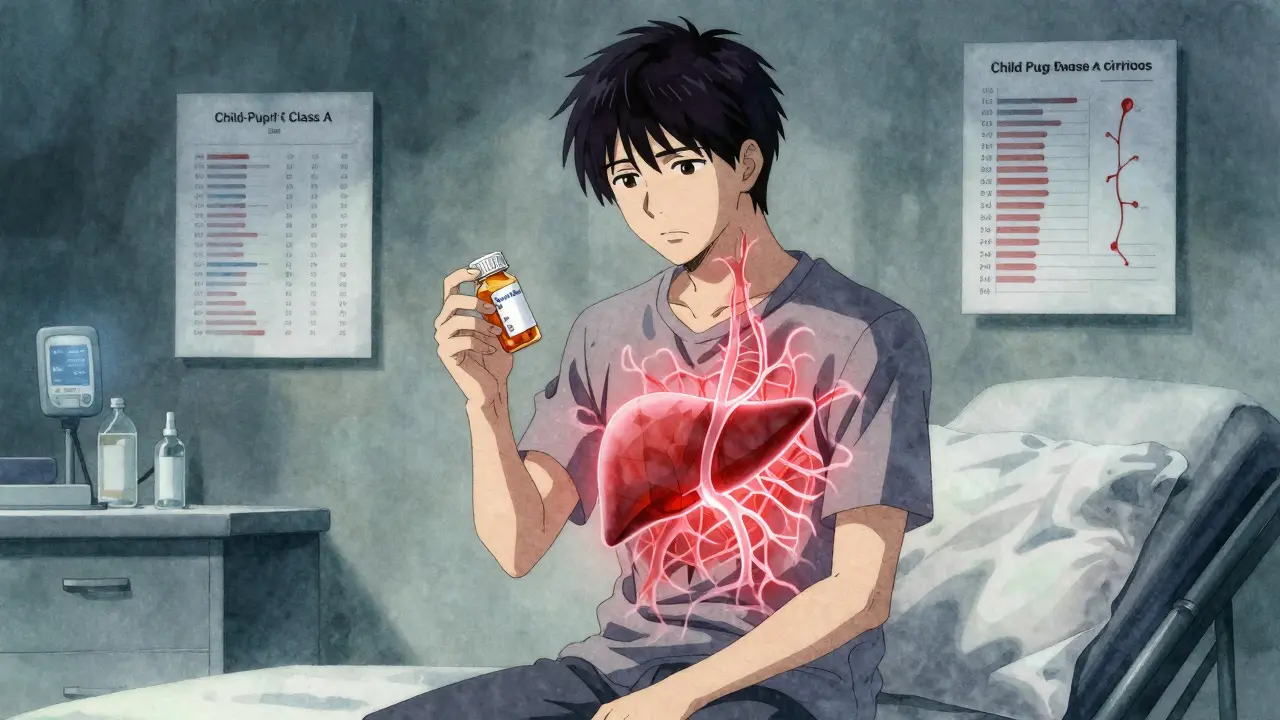
Metformin is the most common pill prescribed for type 2 diabetes worldwide. Millions take it daily. It’s cheap, effective, and has been around for decades. But if you have liver disease, your doctor might tell you to stop it. Why? Because of a rare but dangerous side effect: lactic acidosis.
What Is Lactic Acidosis, and Why Does Metformin Cause It?
Lactic acidosis happens when too much lactic acid builds up in your blood. Your body normally makes small amounts of lactate during exercise or when oxygen is low. Your liver clears it out. But if your liver is damaged, it can’t do that job well. Metformin makes this worse. It blocks a key energy pathway in your cells, which increases lactate production. At the same time, it reduces how much your liver can turn lactate back into glucose. That double hit can push lactate levels into dangerous territory.
The clinical definition is simple: blood pH below 7.35 and lactate above 5 mmol/L. That’s not something you can feel right away. Symptoms are vague-nausea, vomiting, stomach pain, feeling weak. Many people think it’s just a stomach bug. But if you’re on metformin and your liver isn’t working well, these symptoms could be early warning signs. About 83% of people with metformin-related lactic acidosis end up with dangerously low blood pressure. Nearly half need a breathing machine.
The Old Rule: Avoid Metformin in Liver Disease
Back in 1998, regulators said: don’t use metformin if you have chronic liver disease. That rule stuck. It came from fear, not hard data. At the time, phenformin-a similar drug-had caused hundreds of deaths from lactic acidosis. When metformin came along, doctors assumed it was just as risky. But it’s not. Phenformin was broken down by the liver. Metformin? Over 90% leaves your body through your kidneys. That’s why kidney problems are a bigger red flag than liver problems.
Here’s the twist: people with liver disease often have type 2 diabetes. Studies show about 30% of people with cirrhosis also have diabetes. So if you’re one of them, you need treatment. But if metformin is off the table, what’s left? Insulin? Newer drugs? They work-but they’re more expensive, harder to use, and can cause weight gain or low blood sugar.
The New Evidence: Metformin Might Be Safe-Sometimes
In 2024, a major case report in Cureus reviewed the data and found almost nothing to support the blanket ban. Most reports of lactic acidosis in liver patients involved people who were also drinking heavily, had kidney failure, or were taking other drugs. The real risk isn’t the liver disease alone-it’s when liver disease is paired with other problems.
What about non-alcoholic fatty liver disease (NAFLD)? That’s the most common liver condition in people with diabetes. It’s not the same as cirrhosis. In fact, metformin may actually help NAFLD. It reduces fat in the liver, improves insulin sensitivity, and lowers inflammation. A 2022 study showed that patients with NAFLD and diabetes who stayed on metformin had slower disease progression than those who stopped.
The American Diabetes Association updated its 2023 guidelines to say metformin is okay for patients with stable chronic liver disease-even compensated cirrhosis (Child-Pugh Class A). That’s a big shift. It means if your liver is damaged but still working, metformin might be safe. The European Association for the Study of the Liver is preparing new guidelines for 2025 that could go even further, recommending metformin as first-line therapy for NAFLD with diabetes.

When Is Metformin Still Dangerous?
Not all liver disease is the same. If you have decompensated cirrhosis-meaning your liver is failing-you’re at high risk. That’s Child-Pugh Class B or C. Your body can’t clear lactate. Your blood pressure drops. Your organs start shutting down. In these cases, the mortality rate from lactic acidosis is 28% to 47%. No one should take metformin here.
Other red flags:
- Severe kidney problems (eGFR under 30)
- Acute illness with dehydration (like severe diarrhea or infection)
- Heart failure requiring hospitalization
- Alcohol abuse
- Recent contrast dye scan (like a CT scan with contrast)
These aren’t just warnings-they’re triggers to stop metformin immediately. Even if your liver is fine, if your kidneys are struggling or you’re dehydrated, lactate can pile up fast.
How to Use Metformin Safely With Liver Disease
If your doctor says you can stay on metformin, here’s how to do it safely:
- Get your liver function tested every 3 months. Look at ALT, AST, bilirubin, and albumin. If they’re stable, you’re probably okay.
- Check your kidney function every 6 months. eGFR above 45 is ideal. Between 30 and 45? Your dose may need lowering.
- Never skip meals. Fasting increases lactate. If you’re sick and can’t eat, stop metformin until you’re eating normally again.
- Stop metformin 48 hours before any surgery or imaging with contrast dye. Wait until you’re fully recovered and drinking fluids before restarting.
- Watch for symptoms: nausea, vomiting, unusual tiredness, muscle pain, rapid breathing. If you have them, get a lactate test right away.
Some doctors now check lactate levels every 6 months in high-risk patients, even if they feel fine. It’s not routine-but it’s smart if you have cirrhosis or NAFLD with diabetes.
What If You’re Already on Metformin and Have Liver Disease?
Don’t panic. Don’t quit cold turkey. Talk to your doctor. Ask:
- What stage is my liver disease? (Child-Pugh Class A, B, or C?)
- Are my kidneys working well?
- Do I have other risk factors like alcohol use or heart failure?
- Has my diabetes been stable on metformin?
If your liver is mildly affected and everything else is stable, you’re likely fine. Many people with NAFLD have been on metformin for years without issue. The real danger isn’t the drug-it’s the fear of it. Studies like the UKPDS followed patients for 10 years and found zero cases of lactic acidosis in those taking metformin. The COSMIC trial with over 7,000 patients also found no cases.
The data doesn’t support a blanket ban. It supports smart, individualized care.

What Are the Alternatives?
If metformin isn’t safe for you, here are your options:
- Insulin: Works well, but can cause weight gain and low blood sugar.
- GLP-1 agonists (like semaglutide): Help with weight loss and liver fat reduction. Expensive, but very effective.
- SGLT2 inhibitors (like empagliflozin): Lower blood sugar and protect the heart and kidneys. May also reduce liver fat.
- DPP-4 inhibitors (like sitagliptin): Neutral for weight, low risk of low sugar. Safe in liver disease.
None of these are perfect. But they’re options. The goal isn’t just to lower blood sugar-it’s to protect your liver, heart, and kidneys too.
The Bottom Line
Metformin isn’t automatically dangerous if you have liver disease. The old rule is outdated. The real risk is in advanced liver failure-not fatty liver or mild cirrhosis. If you’re on metformin and have liver disease, get your liver and kidney function checked regularly. If you feel unwell, get your lactate tested. Don’t stop your medication without talking to your doctor.
The future of diabetes care in liver disease isn’t about avoiding metformin. It’s about using it wisely. And that starts with knowing your numbers-not your fears.
Can I take metformin if I have fatty liver disease?
Yes, if your liver disease is mild or moderate (like NAFLD without cirrhosis), metformin is generally safe and may even help reduce liver fat. Studies show it improves insulin sensitivity and lowers inflammation in the liver. Always confirm with your doctor that your liver function is stable and your kidneys are working well.
Is lactic acidosis common with metformin?
No, it’s very rare. About 3 to 10 cases happen per 100,000 people taking metformin each year. Most cases occur when other risk factors are present-like kidney failure, severe infection, or alcohol abuse. In healthy people with normal liver and kidney function, the risk is nearly zero.
Why was metformin banned in liver disease if the risk is low?
It was a precaution based on the history of phenformin, a similar drug that caused many deaths. Metformin was assumed to be the same, even though it works differently. Over time, evidence showed the risk was much lower, but guidelines changed slowly. New data from 2023-2024 is finally leading to updated recommendations.
What should I do if I feel sick while taking metformin?
If you have nausea, vomiting, stomach pain, or feel unusually weak or short of breath, stop taking metformin and get medical help immediately. These could be early signs of lactic acidosis. A simple blood test for lactate and pH can confirm it. Don’t wait-it’s treatable if caught early.
Can I restart metformin after a hospital stay?
Only after you’re fully recovered, eating normally, and your kidney and liver function have been checked. If you had dehydration, infection, or contrast dye, wait at least 48 hours after you’re back to normal. Your doctor should check your eGFR and liver enzymes before restarting. Never restart on your own.
Are there new forms of metformin that are safer for the liver?
Extended-release metformin releases the drug more slowly, which may lower peak lactate levels. Some early data from the MET-REVERSE trial suggests it might be safer in mild liver disease, but more research is needed. It’s not a magic fix-but it’s a step forward.
What’s Next?
If you have diabetes and liver disease, your treatment plan should be personal. Don’t assume metformin is off-limits. Don’t assume it’s safe without checking. Ask for your liver and kidney numbers. Know your Child-Pugh class if you have cirrhosis. Track your symptoms. And if you’re unsure-get a second opinion from an endocrinologist or hepatologist.
The goal isn’t to avoid all risk. It’s to manage it. Metformin saves lives. But only if it’s used the right way.






Terri Gladden January 5, 2026
I took metformin for 3 years and my liver enzymes went through the roof. My doctor said it was fine, but then I ended up in the ER with acidosis. They said I was lucky to be alive. Now I’m on insulin and I feel like a zombie, but at least I’m not dying. #MetforminKills
Jennifer Glass January 6, 2026
It’s fascinating how medical guidelines evolve based on fear rather than data. The phenformin panic from the 90s created a legacy of caution that’s still haunting us. Metformin’s pharmacokinetics are so different-it’s almost ironic that we treat liver disease as the red flag when kidneys are the real gatekeepers. The data from UKPDS and COSMIC should’ve changed this decades ago.
Joseph Snow January 8, 2026
Let’s be real-this is Big Pharma pushing metformin because it’s cheap. They don’t care about your liver. They care about profits. Look at how fast the guidelines changed right after the patent expired on newer drugs. Coincidence? I think not. They’re quietly erasing the old warnings so you keep buying it. Read the fine print in those ‘2023 updates’-they’re full of loopholes.
John Wilmerding January 8, 2026
Thank you for this exceptionally clear and evidence-based breakdown. As a clinical pharmacist, I’ve seen too many patients abruptly discontinued on metformin due to outdated protocols, only to suffer worse glycemic control and increased cardiovascular risk. The key is risk stratification: Child-Pugh A with stable eGFR >45? Metformin is not just safe-it’s preferred. Regular monitoring of LFTs and renal function, avoidance of concurrent nephrotoxins, and patient education on symptom recognition are non-negotiable. This is precision medicine in action.
Peyton Feuer January 9, 2026
i read this whole thing and honestly felt better about my meds. i’ve got fatty liver and was scared to death of metformin. my doc said i’m good to stay on it as long as my labs don’t spike. i check my numbers every 3 months and i’ve never felt better. i stopped worrying and started living. thanks for the clarity.
Siobhan Goggin January 10, 2026
The shift in guidelines reflects the maturity of our medical understanding. It’s no longer about blanket prohibitions but about individualized risk assessment. This is how medicine should work-guided by data, not dogma. I hope more clinicians adopt this approach, especially in primary care where fear often overrides evidence.
Vikram Sujay January 11, 2026
The philosophical underpinning of this issue lies in the tension between precautionary principle and evidence-based practice. The historical prohibition against metformin in liver disease was a manifestation of the former-prioritizing the avoidance of rare harm over the certainty of widespread benefit. The emerging consensus, however, aligns with the latter: a calculus of probabilities, where the net benefit of continued therapy outweighs the statistically marginal risk in stable disease. This evolution is not merely clinical-it is epistemological.
Jay Tejada January 12, 2026
so like... you’re telling me the whole time i’ve been scared to take metformin because of my fatty liver, it was basically a myth? lol. my doctor said no, my mom said no, my aunt said no. turns out everyone was just scared of the word ‘acidosis’. i’m gonna keep taking it and maybe even start eating more veggies. thanks for the laugh and the facts.
Shanna Sung January 14, 2026
They’re lying. Metformin causes cancer. The liver thing is just a cover. They don’t want you to know it also messes with your mitochondria long term. Google ‘metformin mitochondrial damage’ and see what they don’t want you to see. Your doctor’s just paid by the pharma companies. I’ve been off it for 2 years and my energy is back. Don’t trust the system.
Allen Ye January 14, 2026
The cultural dimension of this medical paradigm shift is profound. In Western biomedicine, we have historically treated disease as a binary condition-either you have it or you don’t, either you take the drug or you don’t. But the reality of metabolic disease, particularly in the context of non-alcoholic fatty liver disease, is inherently systemic and probabilistic. The move toward nuanced, stage-specific prescribing reflects a broader cultural maturation: away from absolutism, toward contextual intelligence. This isn’t just about liver enzymes-it’s about how we conceptualize health itself.
mark etang January 15, 2026
This is an exemplary model of clinical guidance. The integration of epidemiological data, pharmacokinetic principles, and risk stratification into actionable clinical pathways exemplifies the highest standard of evidence-based medicine. I commend the authors for their meticulous synthesis and urge all healthcare providers to adopt this framework immediately. Patient outcomes will improve significantly.