When you think of psoriasis, you probably picture red, scaly patches on your elbows, knees, or scalp. But for nearly one in three people with psoriasis, the problem doesn’t stop at the skin. Psoriatic arthritis is what happens when the same immune system gone rogue starts attacking your joints - causing pain, swelling, and sometimes permanent damage. It’s not just a side effect. It’s a full-blown disease that connects your skin and your skeleton in ways most people don’t expect.
It’s Not Just Aging or Overuse
Many people assume joint pain means they’re getting older or have worn out their knees from years of running. But psoriatic arthritis is different. It’s not wear and tear. It’s inflammation driven by your immune system. Unlike osteoarthritis, which slowly breaks down cartilage over time, psoriatic arthritis attacks the lining of your joints, tendons, and even where ligaments attach to bone. This is why you might wake up with stiff fingers that feel glued shut - not because you slept wrong, but because your body is actively inflaming itself overnight. The first sign? Often, it’s not the joints at all. It’s your nails. Pitting, lifting, or yellowing nails can show up years before any joint pain. In fact, 80% of people with psoriatic arthritis have nail changes. If you’ve had psoriasis for years and suddenly notice your nails looking strange, don’t ignore it. That’s your body’s early warning system.The Five Faces of Psoriatic Arthritis
This isn’t one condition. It’s five different patterns, each with its own signature. Knowing which one you have helps guide treatment.- Asymmetric oligoarthritis - the most common form - hits fewer than five joints, but not the same ones on both sides. Maybe your left knee and right wrist are swollen, but your right knee is fine. This asymmetry is a big clue that it’s not rheumatoid arthritis.
- Symmetric polyarthritis looks like rheumatoid arthritis - matching joints on both sides - but without the same level of joint destruction. About 25-30% of people with PsA fall into this group.
- Distal interphalangeal predominant (DIP) affects the joints closest to your fingernails. It’s rare in other types of arthritis, so if only those tiny joints are inflamed, PsA is likely.
- Spondylarthritis attacks your spine and lower back. Pain gets worse when you rest, not when you move. That’s the opposite of typical back pain. You might think it’s just a bad posture issue - until you realize your sacroiliac joints are inflamed.
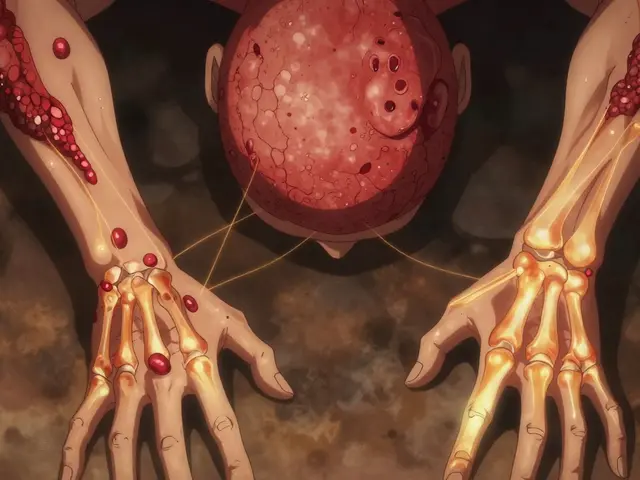
- Arthritis mutilans is rare, but devastating. It eats away at bone, shortening fingers or toes into what doctors call an “opera glass hand.” It’s the most severe form, affecting less than 5% of people.
Dactylitis and Enthesitis: The Hidden Signs
Two symptoms are almost unique to psoriatic arthritis. If you’ve got either, it’s a strong signal. Dactylitis - also called “sausage digits” - is when an entire finger or toe swells up like a sausage. It’s not just the joint. It’s the whole digit: tendons, ligaments, and joint all inflamed at once. About half of people with PsA get this. It’s painful, obvious, and hard to ignore. Enthesitis is inflammation where tendons or ligaments attach to bone. Think Achilles tendon pain at the back of your heel, or bottom-of-the-foot pain that feels like plantar fasciitis - but it’s not from overuse. It’s from your immune system attacking the attachment point. About one in three people with PsA has this. It’s often mistaken for sports injuries or aging.Why Diagnosis Takes So Long
On average, people wait 2 to 5 years to get diagnosed with psoriatic arthritis. Why? Because doctors don’t always connect the dots. A patient might see a dermatologist for skin plaques and a rheumatologist for joint pain - but neither talks to the other. Skin and joints are treated as separate problems. But they’re not. The same immune signals cause both. A 2022 study from the Toronto Psoriatic Arthritis Clinic found that if diagnosis is delayed more than 12 months, joint damage progresses 3.2 times faster than in those diagnosed early. That’s not a small difference. It’s the difference between managing symptoms and losing mobility. And here’s the kicker: in 15% of cases, joint pain comes before the skin rash. That means someone could be walking around with inflamed knees or swollen fingers for months, thinking it’s just a sprain - while psoriasis quietly develops later. No one connects the dots until it’s too late.
What Sets It Apart From Other Arthritis
It’s easy to confuse psoriatic arthritis with rheumatoid arthritis or osteoarthritis. But there are clear differences.- Rheumatoid arthritis usually hits the same joints on both sides - both wrists, both knees. It’s symmetric. PsA is often asymmetric. Plus, rheumatoid factor blood tests are positive in 80% of RA cases - but always negative in PsA.
- Osteoarthritis is degenerative. It’s cartilage wearing out. No swelling, no redness, no morning stiffness lasting over an hour. PsA has all three.
- X-ray clues: PsA shows unique patterns - “pencil-in-cup” deformities where bone erodes unevenly, or “whiskering” - new bone growth along tendons. These don’t show up in RA or OA.
Triggers and Risk Factors
You can’t control your genes, but you can control some triggers.- Stress - cited by 85% of patients - is the biggest flare trigger. Anxiety, sleep loss, emotional strain: all can crank up inflammation.
- Infections, especially strep throat, can spark PsA in people genetically prone to it. One study found a 1.8-fold increase in PsA within six months of a strep infection.
- Obesity more than doubles your risk. Fat tissue isn’t just storage - it’s active, releasing inflammatory chemicals that feed the disease.
- Joint injury can trigger PsA right where the trauma happened. If you twisted your ankle badly and then started having pain there months later, that’s not coincidence.
How It’s Treated - and What’s New
Treatment has changed dramatically in the last decade. It’s no longer just about painkillers.- DMARDs like methotrexate are still used in 65% of cases, but they often aren’t enough.
- TNF inhibitors - drugs like adalimumab or etanercept - help 65% of patients reach minimal disease activity within six months.
- IL-17 and IL-23 inhibitors are newer and more targeted. Guselkumab, an IL-23 blocker, showed a 64% improvement in joint symptoms at 24 weeks in a 2023 trial - far better than placebo.

Why Integrated Care Matters
The best outcomes happen when your dermatologist and rheumatologist talk. A 2023 study showed 82% of patients with coordinated care reached treatment goals - compared to just 54% when seeing only one specialist. That means: if you have psoriasis and joint pain, don’t wait. Ask for a referral to a rheumatologist. Bring your skin photos. Mention nail changes. Tell them about your fatigue. Don’t let them treat skin and joints as separate issues.Life With Psoriatic Arthritis
Fatigue hits 65% of people with PsA. Not just tired - exhausted. It’s not laziness. It’s your immune system burning energy 24/7. Work disability affects over half of patients within 10 years. But early treatment changes that. People who start biologics within six months of symptoms have 73% less joint damage at two years. And yes - cold weather makes it worse. So does stress. But so does movement. Gentle exercise - swimming, yoga, walking - keeps joints flexible and reduces inflammation. Don’t rest too much. Move, even if it hurts a little.What’s Next?
By 2027, treatment may be guided by your genes and blood proteins - not trial and error. Researchers are already testing biomarkers that predict who will respond to which drug. That means less guessing. More precision. The message is clear: psoriatic arthritis isn’t just a skin disease with joint pain. It’s a systemic condition that needs early, aggressive, and coordinated care. If you have psoriasis and unexplained joint pain, stiffness, or swollen fingers - don’t wait. See a rheumatologist. Get tested. Get treated. Your joints won’t thank you later - but they’ll thank you now.Can psoriatic arthritis happen without skin psoriasis?
Yes. About 15% of people develop joint symptoms before any visible skin plaques appear. This makes diagnosis harder, because doctors may not suspect psoriatic arthritis without the classic skin signs. Nail changes - like pitting or lifting - can be the only clue. If you have unexplained joint pain and nail abnormalities, ask about PsA even if your skin looks normal.
Is psoriatic arthritis the same as rheumatoid arthritis?
No. While both cause joint inflammation, rheumatoid arthritis is symmetric - affecting matching joints on both sides - and usually tests positive for rheumatoid factor. Psoriatic arthritis is often asymmetric, affects the spine and entheses, and is always rheumatoid factor negative. Nail changes, dactylitis, and enthesitis are unique to PsA and rarely seen in RA.
Does psoriatic arthritis get worse over time?
Without treatment, yes. Joint damage can become permanent, especially if diagnosis is delayed more than 6 months. About 50-70% of patients show bone changes on X-rays within 5 years. But early treatment with biologics can stop or slow this progression. The key is catching it before the damage is done.
Can lifestyle changes help with psoriatic arthritis?
Absolutely. Losing weight if you’re overweight cuts inflammation and improves drug effectiveness. Regular low-impact exercise - like swimming or cycling - keeps joints moving and reduces stiffness. Avoiding smoking and managing stress also lowers flare frequency. Diet alone won’t cure it, but a healthy lifestyle supports treatment and improves quality of life.
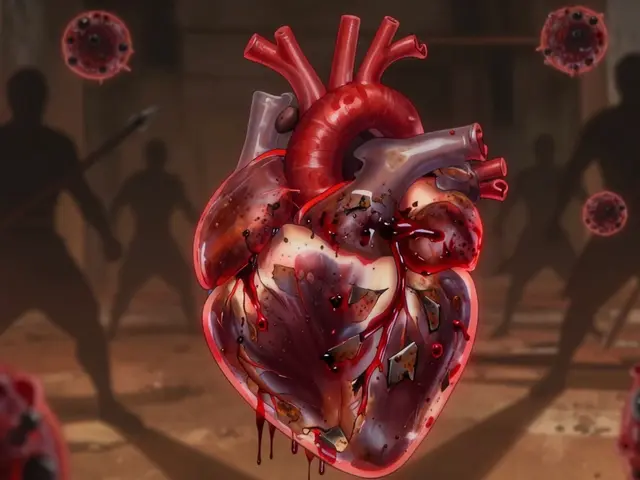
Are biologics safe for long-term use?
Biologics are generally safe when monitored. They suppress part of the immune system, so you’re at slightly higher risk for infections like tuberculosis or hepatitis. Regular blood tests and screenings are required. JAK inhibitors carry a small increased risk of heart problems and cancer, so they’re not first-line for people with existing cardiovascular risk. But for most, the benefits of preventing joint damage far outweigh the risks.
How do I know if my treatment is working?
Your doctor will track several things: number of swollen or tender joints, levels of fatigue, nail and skin improvement, and sometimes blood markers like CRP or ESR. Imaging (like ultrasound or MRI) may be used to check for inflammation in tendons or joints. If you’re still having morning stiffness, swollen fingers, or pain after 3-6 months on treatment, your regimen may need adjustment.




Gabrielle Panchev January 6, 2026
Okay, but have you considered that maybe the immune system isn’t ‘rogue’-maybe it’s just trying to fix something the modern world broke? Like, we’ve been eating processed junk for 70 years, living in sterile environments, and blaming our bodies for being ‘overactive’? It’s not psoriatic arthritis-it’s systemic disappointment. Your skin and joints are just the canaries in the coal mine. Also, I’ve seen people with zero psoriasis and full-blown PsA, and I’m convinced it’s linked to glyphosate. Not saying I’m right. But I’m not wrong either.
Katelyn Slack January 8, 2026
i think this is so importent to share… i had nail pitting for 3 years before i got joint pain and no one ever connected it. i just thought my nails were weird. now i know. thank you for writing this. i wish more doctors knew this.
Melanie Clark January 10, 2026
They don't want you to know this but the pharmaceutical companies are secretly funding dermatologists to ignore joint pain because biologics make them billions. They'll let you suffer for years until your bones turn to dust. And don't even get me started on the WHO's hidden agenda to push JAK inhibitors because they're easier to patent. Your fatigue? It's not just inflammation. It's the system gaslighting you. You're not broken. They are.
Harshit Kansal January 11, 2026
Bro this is wild. I had dactylitis and thought I just crushed my toe in a soccer game. Turns out it was PsA. Started biologics and now I can actually wear shoes again. Life changed. Also yoga helps. Not saying it cures it but it helps. Stay strong.
Brian Anaz January 12, 2026
Look. We’ve got people in this country getting sick because they won’t take responsibility. You get fat. You eat garbage. You sit all day. Then you blame your immune system. It’s not a conspiracy. It’s laziness. Get off your butt. Walk. Eat real food. Stop whining. Biologics aren’t magic. They’re a bandaid for bad choices.
Venkataramanan Viswanathan January 14, 2026
In India, we have a term for this-'dard ka karan nahi, samadhan chahiye'. The cause is not the issue; the solution is. Many of us ignore nail changes because we think it's 'just a nail problem'. But as this article rightly says, it's a systemic signal. I have seen patients in rural clinics misdiagnosed for years. The gap between awareness and access is vast. We need community health workers trained to spot dactylitis and enthesitis. Not just doctors in cities.
Vinayak Naik January 14, 2026
Man, I used to think my stiff fingers were just from typing too much. Then I noticed my nails looked like someone dropped them in acid. I went to the doc and he said 'oh, that’s psoriasis, right?' I said yeah. He said 'cool, let’s get you on methotrexate.' No tests. No MRI. No nothing. I’m lucky I caught it early. But I know a guy who waited five years and now his knuckles look like crumpled paper. Don’t be like him. If your nails are acting up, don’t ignore it. Your body’s yelling. Listen.
Saylor Frye January 16, 2026
Interesting. Though I must say, the framing here feels almost… reductionist. You’re reducing a complex immunological cascade to a checklist of symptoms, as if the body operates like a diagnostic flowchart. The real tragedy isn’t delayed diagnosis-it’s the epistemological arrogance of modern medicine that believes it can map the soul’s rebellion onto a radiograph. What if the joints are screaming because the self has been silenced? Just a thought.
Kiran Plaha January 16, 2026
Just wondering-how often do people with PsA get misdiagnosed with fibromyalgia? My cousin was told she had chronic fatigue for years, but her nails were always weird. When she finally saw a rheumatologist, it turned out to be PsA. She cried. I cried. It’s so easy to miss if no one connects the dots.
Matt Beck January 17, 2026
Life is just a series of invisible wars inside us. 🌌 The skin, the joints, the mind-they’re all just reflections of the same storm. We treat symptoms like enemies, but what if they’re messengers? What if the inflammation isn’t your body attacking you… but your body trying to scream, ‘I’m still here!’? I’ve been on Humira for 4 years. My knuckles still crack. But I’m alive. And that’s enough. 🙏