Atrial Fibrillation Treatment: What Works, What Doesn’t, and How to Stay Safe
When your heart beats irregularly—fast, fluttering, or skipping beats—you might be dealing with atrial fibrillation, a common heart rhythm disorder where the upper chambers of the heart beat out of sync with the lower chambers. Also known as AFib, it raises your risk of stroke, heart failure, and other complications if left untreated. This isn’t just about feeling off. It’s about protecting your heart long-term with the right mix of meds, monitoring, and lifestyle moves.
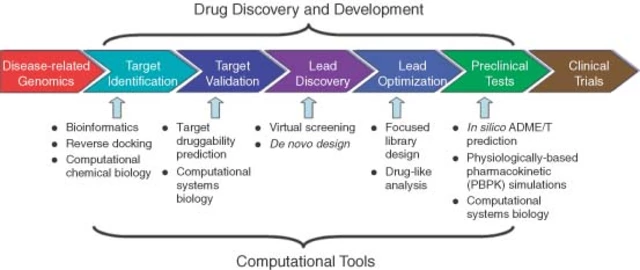
Most atrial fibrillation treatment, a strategy focused on controlling heart rate, restoring normal rhythm, and preventing blood clots starts with one of two paths: rate control or rhythm control. Rate control means using drugs like beta blockers, medications that slow the heart rate and reduce strain on the heart—think propranolol or metoprolol—to keep your pulse steady even if the rhythm stays irregular. Rhythm control tries to get your heart back into a normal beat, often with antiarrhythmic drugs or procedures like cardioversion. But here’s the catch: some of these drugs, especially when mixed with others, can cause dangerous QT prolongation, a condition where the heart’s electrical cycle stretches too long, raising the risk of sudden cardiac arrest. That’s why knowing your full med list matters—antipsychotics, certain antibiotics, or even some antidepressants can stack up and push your heart into danger.
Then there’s the silent threat: blood clots. Anticoagulants, blood thinners like warfarin or newer options like apixaban that prevent clots from forming in the heart are often the most important part of treatment. Skipping them because you feel fine is a gamble—AFib can cause clots without you ever feeling symptoms. But these drugs aren’t risk-free either. They need regular check-ins, especially if you’re on warfarin. And if you’ve had a recent switch to a generic version, you’ll want to track how your body responds—some people notice subtle changes in energy, bruising, or even dizziness that signal the dose needs tweaking.
What you won’t find in most brochures? The real-world messiness. A pill that works for one person might cause fatigue or cold hands in another. A drug that lowers your heart rate might make you too tired to walk the dog. And if you’re also taking meds for anxiety, high blood pressure, or even acid reflux, those interactions can sneak up on you. That’s why tracking your symptoms, knowing your lab numbers, and asking your doctor about every med on your list isn’t just smart—it’s lifesaving.
Below, you’ll find real posts from people who’ve walked this path. They’ve tested how generic switches affect their rhythm control, tracked long-term side effects of beta blockers, and learned which drug combos put them at risk for arrhythmias. No fluff. Just what works, what doesn’t, and how to protect yourself.
Anticoagulants for Seniors: When Stroke Prevention Outweighs Fall Risk
Anticoagulants for seniors with atrial fibrillation prevent strokes far more effectively than they increase bleeding risk from falls. Learn why stopping blood thinners after a fall is often dangerous-and what to do instead.