Opioid Use Disorder – What It Is and Why It Matters
Opioid use disorder (OUD) is a medical condition that shows up when your brain and body become dependent on opioid drugs. It isn’t just about occasional use; it means cravings, loss of control, and continuing use despite harm. In the U.S., millions of people face OUD, and the good news is that help exists.
Everyone who uses opioids—whether prescription painkillers or illegal heroin—has some risk of developing OUD. Factors like genetics, chronic pain, mental health issues, and a history of substance use can raise that risk. Understanding these triggers helps you spot problems early and take action before they spiral.
Common Signs and Symptoms
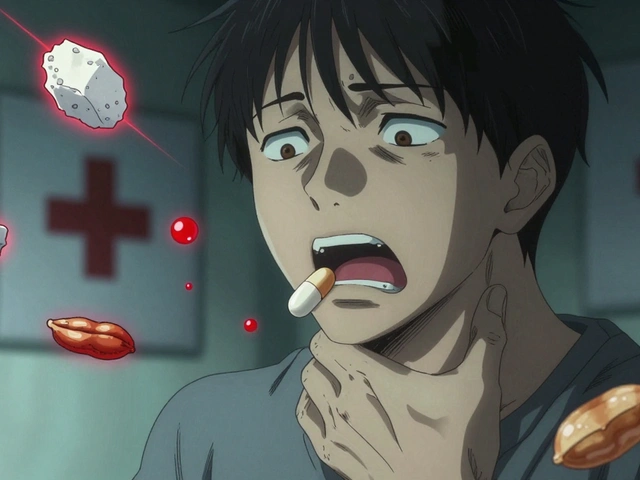
Physical signs include frequent drowsiness, pinpoint pupils, and a sudden need for higher doses to feel the same effect. You might notice withdrawal symptoms like sweating, nausea, or shaking when you miss a dose. Behavioral clues are often clearer: secretive phone calls, borrowing pills, or neglecting work and family responsibilities.
Psychological signs are just as important. Cravings that dominate your thoughts, mood swings, or using opioids to cope with stress are red flags. If you or a loved one shows several of these signs, it’s time to consider evaluation by a health professional.
Effective Treatment Options
Medication‑assisted treatment (MAT) is the gold standard for OUD. Buprenorphine, methadone, and naltrexone can reduce cravings and block the high from opioids, making it easier to focus on recovery. These meds are usually combined with counseling, because changing habits requires both brain chemistry and mindset work.
Therapy comes in many forms—cognitive‑behavioral therapy (CBT), motivational interviewing, and peer‑support groups like NA. Counseling helps you identify triggers, develop coping skills, and rebuild relationships that may have been strained by drug use.
Detox is a short‑term step that clears opioids from your system, but on its own it doesn’t prevent relapse. Most experts recommend starting MAT right after detox to keep cravings in check. Many clinics now offer telehealth appointments, so you can begin treatment from home without a long wait.
Finding a provider is easier than you think. Check your insurance portal for covered OUD programs, or visit reputable sites that list certified addiction specialists. Ask about medication options, counseling availability, and whether they provide after‑hours support.
Staying in recovery means building a new routine. Simple habits—regular exercise, a balanced diet, and consistent sleep—support brain health. Keep a list of emergency contacts, such as a trusted friend or a local hotline, for moments when cravings feel overwhelming.
If you’re reading this and see yourself in any of the signs, reach out today. A quick call to a local clinic or a trusted doctor can set the first step toward a safer, healthier life. Remember, OUD is treatable, and you don’t have to face it alone.
Prescription Opioids and Their Role in the Addiction Crisis
A deep look at how prescription opioids contribute to the addiction crisis, covering risks, statistics, regulations, alternatives, and practical steps for patients and doctors.