Anaphylaxis: Causes, Symptoms, and What to Do in an Emergency
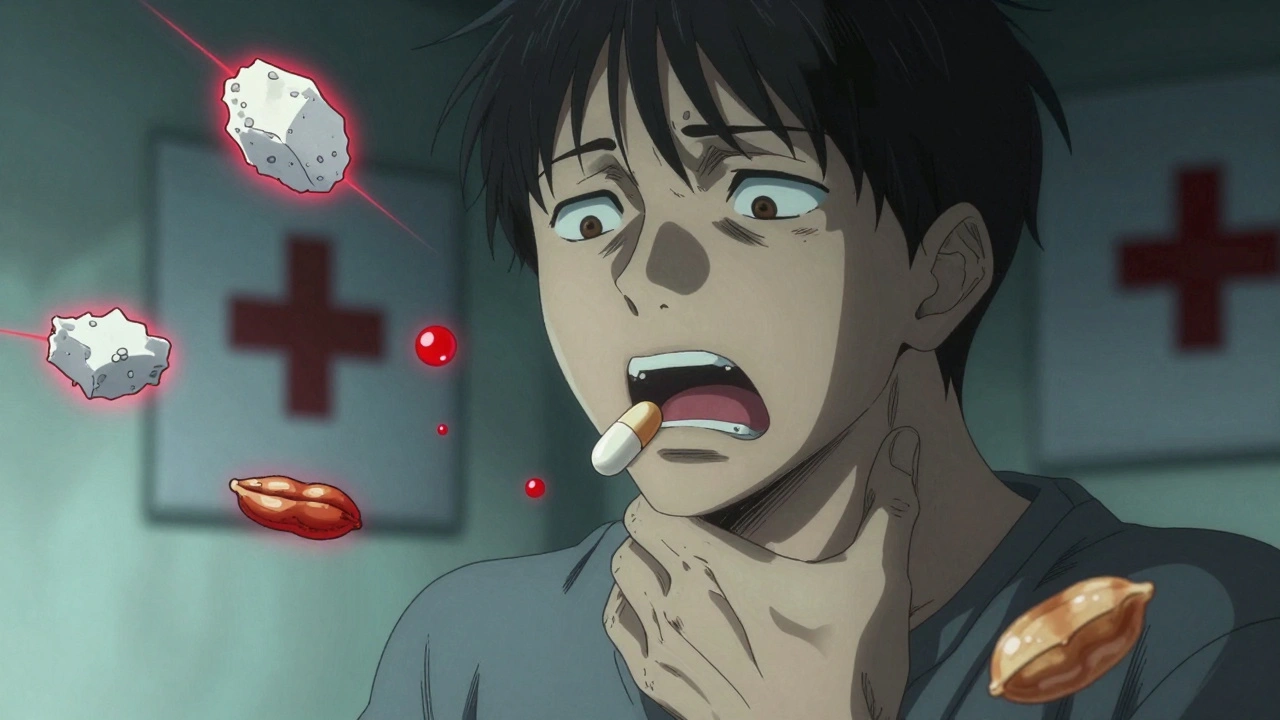
When your body overreacts to something harmless—like peanuts, bee stings, or certain medicines—it can trigger anaphylaxis, a sudden, severe, and potentially deadly allergic reaction. Also known as anaphylactic shock, it doesn’t wait for permission—it hits fast, and without quick action, it can stop your breathing or your heart. This isn’t just a bad rash or a stuffy nose. Anaphylaxis is a medical emergency that demands immediate treatment, usually with epinephrine, a life-saving medication that reverses airway swelling and low blood pressure.
Anaphylaxis can start within seconds or minutes after exposure to an allergen, a substance your immune system wrongly sees as dangerous. Common triggers include foods like peanuts, shellfish, and eggs; insect stings from bees or wasps; and medications like penicillin or NSAIDs. Even latex or exercise in rare cases can set it off. The reaction isn’t always predictable—someone might eat peanuts for years with no issue, then suddenly go into anaphylaxis. That’s why knowing the signs matters more than ever.
Signs of anaphylaxis include swelling of the lips, tongue, or throat; trouble breathing or wheezing; hives or skin turning pale or blue; dizziness, fainting, or a rapid, weak pulse. Nausea, vomiting, or a feeling of doom often come with it. If you or someone else shows even one of these symptoms after exposure to a known trigger, don’t wait. Use an epinephrine injector right away—even if you’re not 100% sure. Then call 911. Epinephrine works fast, but the reaction can bounce back. You still need to go to the ER.
Many people carry epinephrine pens because they’ve had a reaction before. But even if you’ve never had one, you should know what to do. Kids with food allergies, adults with bee sting allergies, and anyone on new medications are at higher risk. Keeping an epinephrine pen in your bag, car, or workplace isn’t overkill—it’s smart. And teaching family, coworkers, or teachers how to use it could save a life.
There’s no cure for allergies that cause anaphylaxis, but you can control your risk. Avoid known triggers, read labels carefully, wear a medical alert bracelet, and have a plan. If you’ve ever had a serious reaction, seeing an allergist helps you understand what you’re reacting to and how to stay safe. Most people who use epinephrine quickly recover fully—but delay can be fatal.
Below, you’ll find real-world guides on managing allergies, avoiding dangerous drug interactions, and protecting yourself and others from hidden triggers. Whether you’re dealing with a known risk or just want to be prepared, these posts give you the clear, practical steps you need to stay safe.
Severe Adverse Drug Reactions: When to Seek Emergency Help
Severe drug reactions can kill in minutes. Learn the warning signs of anaphylaxis, Stevens-Johnson Syndrome, and other life-threatening reactions-and exactly when to call 911.
Allergic Reactions to Generics: When to Seek Medical Care
Generic medications can cause allergic reactions due to inactive ingredients like dyes, lactose, or gluten - even when the brand-name version is safe. Learn the warning signs, when to seek emergency care, and how to protect yourself.