Cardiac Risk: Understand Your Heart Danger Signs and What You Can Do
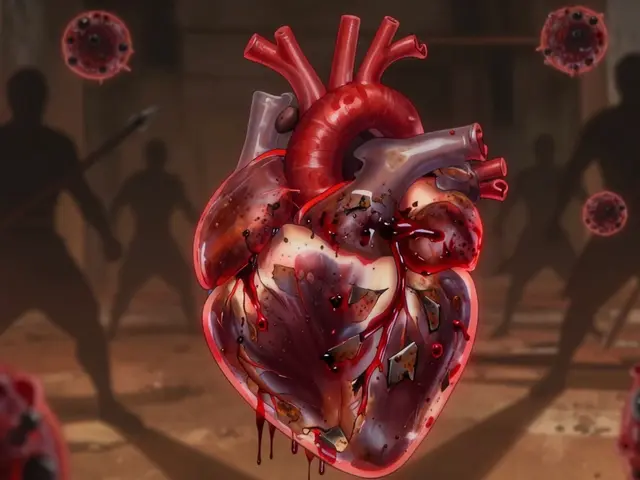
When we talk about cardiac risk, the chance of developing heart disease or having a heart event like a heart attack or stroke. Also known as heart disease risk, it’s not just about being overweight or eating too much salt—it’s a mix of genetics, lifestyle, and even the medicines you take every day. Many people think cardiac risk is something you either have or you don’t. But the truth is, it builds slowly. High blood pressure, high cholesterol, diabetes, smoking, and even long-term use of certain painkillers or antibiotics can quietly raise your risk without you noticing until it’s too late.
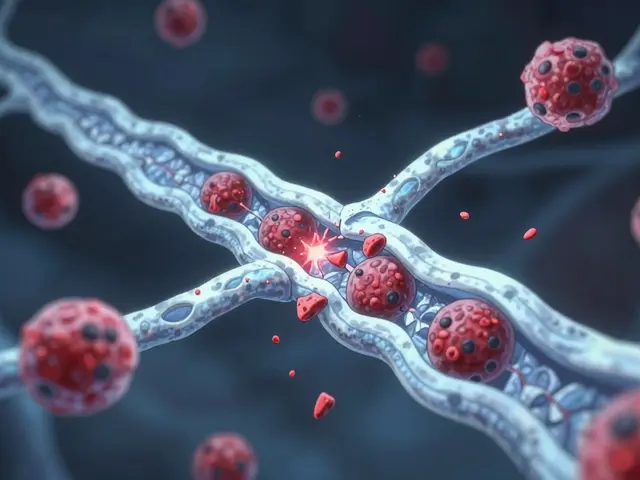
One of the most overlooked parts of cardiac risk is how everyday drugs affect your heart. For example, statins, medicines used to lower cholesterol. Also known as cholesterol-lowering drugs, they’re lifesavers for millions—but they can sometimes cause minor liver enzyme changes that signal stress on your body’s systems. That’s why monitoring isn’t just a formality—it’s part of keeping your heart safe. Same goes for NSAIDs, pain relievers like ibuprofen or naproxen. Also known as nonsteroidal anti-inflammatory drugs, they’re common for arthritis or menstrual pain, but studies show long-term use can increase blood pressure and strain the heart. Even something as simple as a cold medicine with pseudoephedrine can spike your heart rate if you’re already at risk.
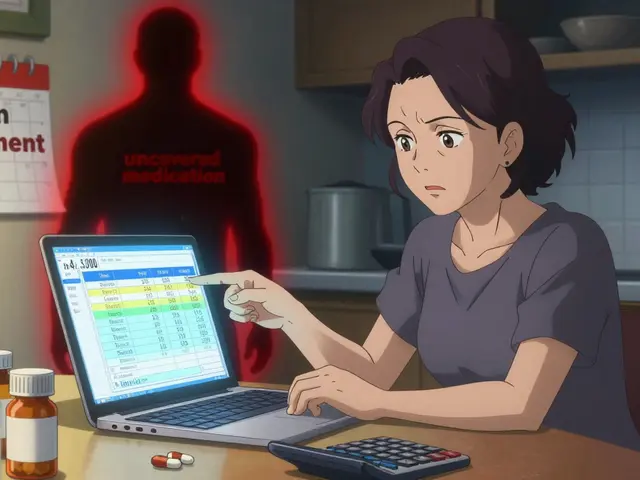
Cardiac risk doesn’t happen in a vacuum. It’s tied to other conditions like kidney disease, where phosphate binders like PhosLo are used, or diabetes, where GLP-1 drugs like Rybelsus help control blood sugar but need careful heart monitoring. If you’re on multiple meds, especially for chronic issues, your heart is often the silent witness to their combined effects. That’s why understanding organ-specific side effects, how drugs impact liver, kidneys, nerves, and especially the heart. Also known as drug toxicity, this isn’t just a side note—it’s central to staying healthy over time. A medication that helps your lungs or joints might be quietly working against your heart.
You don’t need to be scared of every pill you take. But you do need to be aware. Know your numbers—blood pressure, cholesterol, blood sugar. Ask your doctor if your meds could be adding to your cardiac risk. And if you’ve noticed unexplained swelling, fatigue, or irregular heartbeat, don’t brush it off. These aren’t normal aging signs—they could be your body’s way of saying something’s off.
Below, you’ll find real comparisons and clear breakdowns of medications that affect your heart, whether it’s how statins impact liver enzymes, how NSAIDs raise blood pressure, or what alternatives exist if your current treatment is putting you at risk. No fluff. Just facts that help you make smarter choices for your heart.
Antipsychotics and QT-Prolonging Drugs: What You Need to Know About Arrhythmia Risk
Combining antipsychotics with other QT-prolonging drugs can dangerously stretch the heart's electrical cycle, raising the risk of sudden cardiac arrest. Learn which medications increase this risk, who's most vulnerable, and how to prevent life-threatening arrhythmias.